CHAPTER 61 Anterior abdominal wall
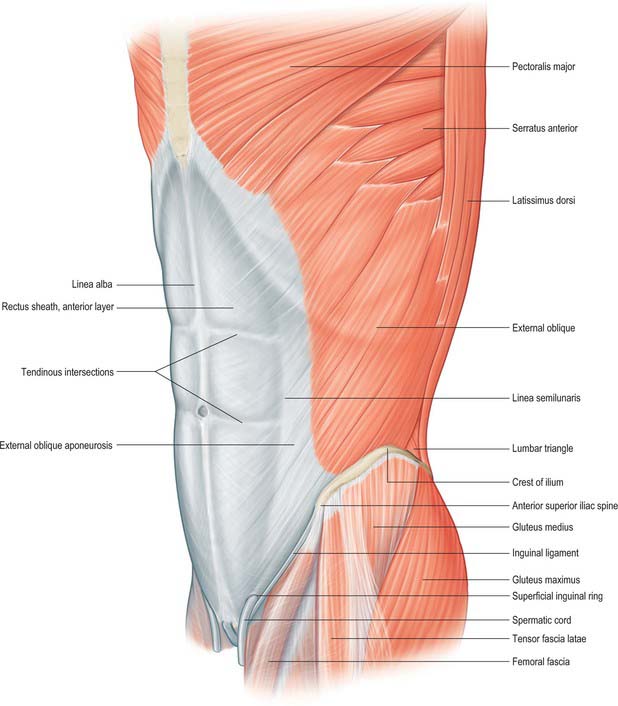
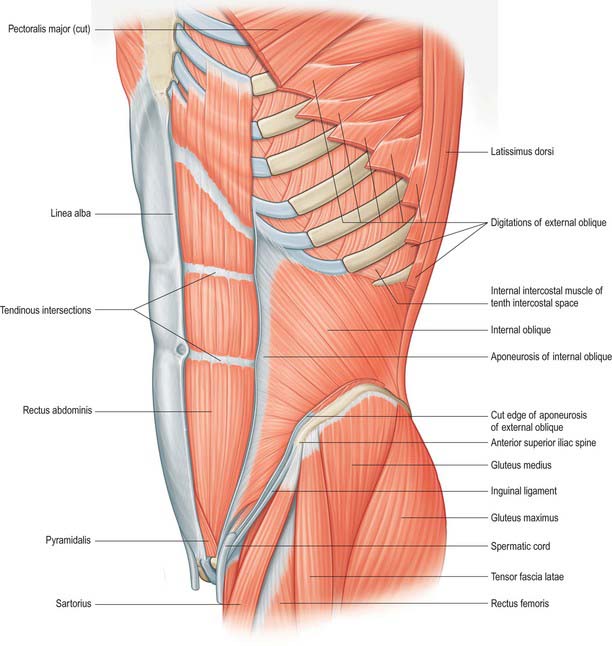
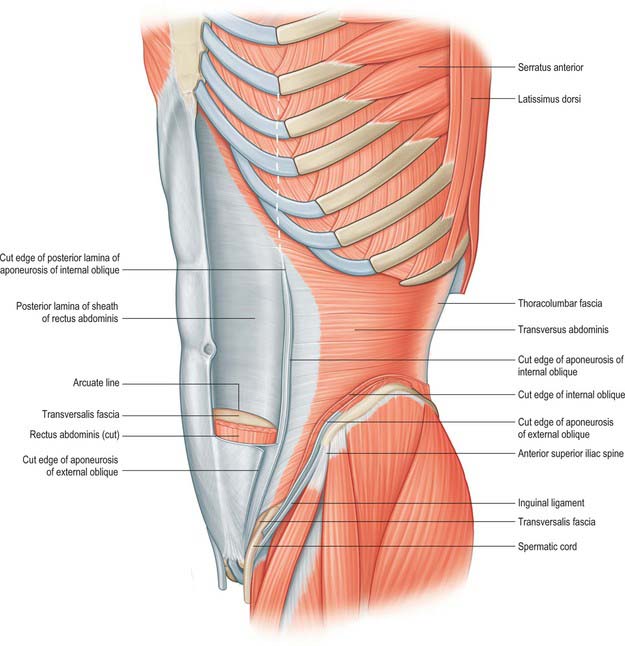
The anterior abdominal wall extends from the costal margins and xiphoid process superiorly to the iliac crests, pubis and pubic symphysis inferiorly. It overlaps and is connected to both the posterior abdominal wall and paravertebral tissues. It forms a continuous but flexible sheet of tissue across the anterior and lateral aspects of the abdomen. The anterior abdominal wall is composed of the integument, muscles and connective tissue lining the peritoneal cavity (Figs 61.1–61.5). It has an important role in maintaining the form of the abdomen and is involved in many physiological activities. Anterior abdominal wall tissues form the inguinal canal that connects the abdominal cavity to the scrotum in men or labia majora in women, and also form the umbilicus; both of these sites are of considerable clinical importance.
SKIN AND SOFT TISSUE
VASCULAR SUPPLY AND LYMPHATIC DRAINAGE
Superior epigastric artery and veins
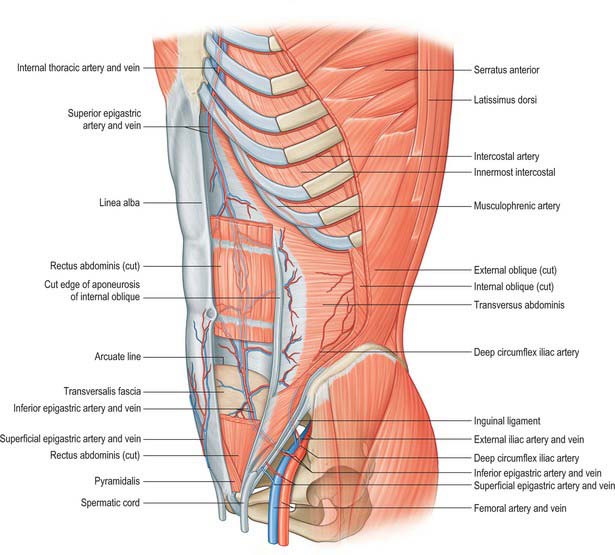
The superior epigastric artery is a terminal branch of the internal thoracic artery. It descends between the costal and xiphoid slips of the diaphragm, accompanied by two or more veins (Fig. 61.4). The vessels pass anterior to the lower fibres of transversus thoracis and the upper fibres of transversus abdominis. The artery enters the rectus sheath behind rectus abdominis and runs down to anastomose with the inferior epigastric artery usually above the level of the umbilicus. Branches supply rectus abdominis and perforate the sheath to supply the abdominal skin. A branch given off in the upper rectus sheath passes anterior to the xiphoid process of the sternum and anastomoses with the same contralateral branch. This vessel may give rise to troublesome bleeding during surgical incisions that extend up to and alongside the xiphoid process. The superior epigastric artery supplies small branches to the anterior part of the diaphragm. On the right, small branches reach the falciform ligament, where they anastomose with branches arising from the hepatic artery.
Inferior epigastric artery and veins
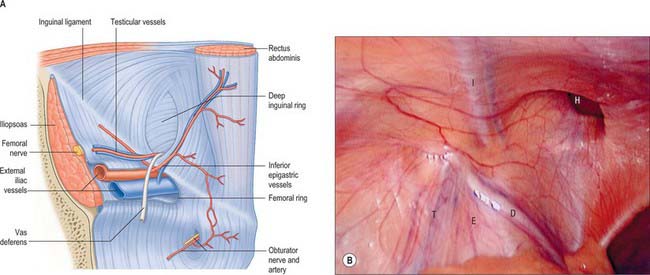
The inferior epigastric artery originates from the external iliac artery posterior to the inguinal ligament (Fig. 61.6). Its accompanying veins, usually two, drain into the external iliac vein. It curves forwards in the anterior extraperitoneal tissue and ascends obliquely along the medial margin of the deep inguinal ring. It lies posterior to the spermatic cord, but is separated from it by the transversalis fascia. It pierces the transversalis fascia which forms the flimsy posterior support of rectus abdominis, and ascends between the muscle and the fascia and overlying pre-peritoneal connective tissue. In this part of its course, it raises the parietal peritoneum of the anterior abdominal wall as the lateral umbilical fold but has little supporting tissue posteriorly. Disruption of the artery, by surgical incisions e.g. for laparoscopic ports or drains, is not uncommon and the resulting haematoma may expand to considerable size because of the lack of tissue against which the bleeding is effectively compressed. The artery divides into numerous branches. Those which anastomose with branches of the superior epigastric artery do so posterior to rectus abdominis at a variable height above the umbilicus. The inferior epigastric vessels are usually significantly larger than the superior vessels and provide the ‘dominant’ supply to rectus abdominis. Preparatory ligation of the inferior epigastric artery is often performed for myo(cutaneous) flaps using the mid or lower rectus abdominis based on the superior epigastric artery to allow expansion of the superior arterial flow to improve viability of the flap. Branches anastomose with terminal branches of the lower six posterior intercostal arteries posterior to rectus abdominis at the lateral border close to the sheath. The artery is an important inferomedial relation of the deep inguinal ring, and may be damaged during extensive medial dissection of the deep ring during hernia repair, particularly when this is performed in the preperitoneal plane. The vas deferens in the male, or round ligament in the female, wind laterally round it. It has the following branches: the cremasteric artery, a pubic branch, and muscular and cutaneous branches.
The cremasteric artery accompanies the spermatic cord in males and supplies the cremaster and other coverings of the cord. It anastomoses with the testicular artery. In females it is small and accompanies the round ligament. A pubic branch, near the femoral ring, descends posterior to the pubis and anastomoses with the pubic branch of the obturator artery. Occasionally, the pubic branch of the inferior epigastric artery is larger than the main obturator artery origin, and it supplies the majority of flow into the obturator artery in the thigh. It is then referred to as the aberrant obturator artery. It lies close to the medial border of the femoral ring and may be damaged in medial dissection of the ring during femoral hernia repair. Muscular branches supply the abdominal muscles and peritoneum, and anastomose with the circumflex iliac and lumbar arteries. Cutaneous branches perforate the aponeurosis of external oblique, supply the skin and anastomose with branches of the superficial epigastric artery.
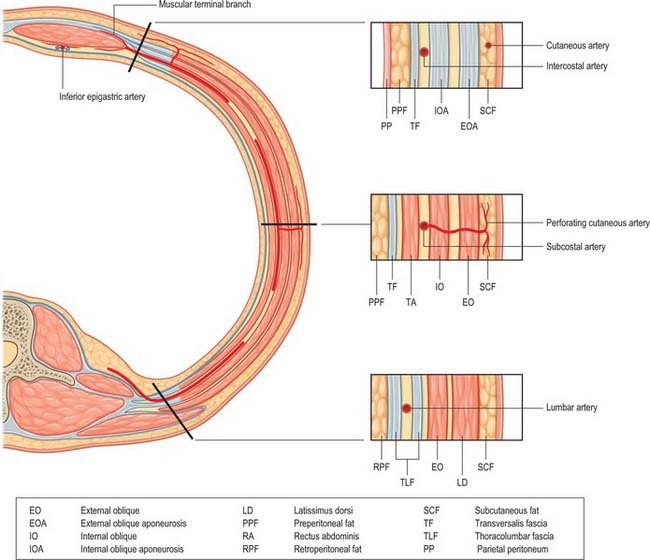
Posterior intercostal, subcostal and lumbar arteries
The 10th and 11th posterior intercostal arteries and the subcostal artery emerge from under the subcostal groove of their respective ribs and pass into the tissues of the anterior abdominal wall. They run through the aponeurosis of transversus abdominis and lie deep to the fibres of internal oblique. The lumbar arteries also cross the aponeurosis of transversus abdominis and lie deep to internal oblique. The arteries on either side run forward, giving off muscular branches to the overlying internal and external oblique, before anastomosing with the lateral branches of the superior and inferior epigastric arteries at the lateral border of the rectus sheath (Fig. 61.7). Perforating cutaneous vessels run vertically through the muscles to supply the overlying skin and subcutaneous tissue. A small contribution to the supply of the lower abdominal muscles comes from branches of the deep circumflex iliac arteries.
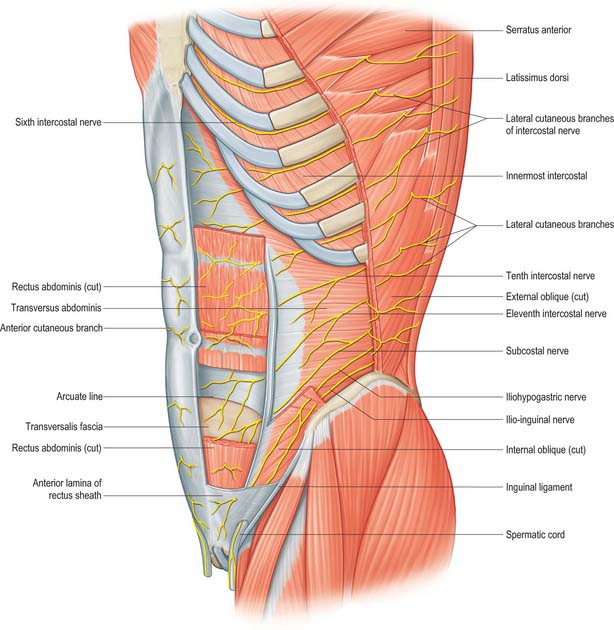
SEGMENTAL NERVES
The seventh to the 12th lower thoracic ventral rami continue anteriorly from the intercostal spaces into the abdominal wall (Fig. 61.3). Approaching the anterior ends of their respective spaces, the seventh and eighth nerves curve superomedially across the deep surface of the costal cartilages between the digitations of transverse abdominis. They reach the deep aspect of the posterior layer of the aponeurosis of internal oblique. Both the seventh and eighth nerves then run through this aponeurosis, pass posterior to rectus abdominis and supply branches to the upper portion of the muscle. They pass through the muscle near its lateral edge and pierce the anterior rectus sheath to supply the skin of the epigastrium.
The ninth to 11th intercostal nerves pass from their intercostal spaces between digitations of the diaphragm and transversus abdominis. They enter the layer between transversus abdominis and internal oblique. Here, the ninth nerve runs forwards almost horizontally, whereas the tenth and 11th pass inferomedially. At the lateral edge of rectus abdominis, the nerves pierce the posterior layer of the aponeurosis of internal oblique and pass behind the muscle to end, like the seventh and eighth intercostal nerves, with cutaneous branches. The ninth nerve supplies skin above the umbilicus, the tenth supplies skin, which includes the umbilicus, and the 11th supplies skin below the umbilicus (see Fig. 15.12 and Chapters 42, 45 and 79). The 12th thoracic nerve (subcostal nerve) connects with the first lumbar ventral ramus (dorsolumbar nerve). It accompanies the subcostal vessels along the inferior border of the 12th rib, passing behind the lateral arcuate ligament and kidney and anterior to the upper part of the quadratus lumborum. It perforates the transversus abdominis fascia, running deep to the internal oblique, to be distributed like the lower intercostal nerves. It supplies the anterior gluteal skin reaching down to the greater trochanter.
MUSCLES
ANTEROLATERAL MUSCLES OF THE ABDOMEN
Rectus abdominis, pyramidalis, external oblique, internal oblique and transversus abdominis constitute the anterolateral muscles of the abdomen. They act together to perform a range of functions, some of which involve the generation of a positive pressure within one or more body cavities. Although many of these activities may occur with no ‘forced assistance’, activities such as expiration, defecation and micturition may be aided by the generation of a positive intra-abdominal pressure. Parturition, coughing and vomiting always require such a positive pressure. Under resting conditions, the tone developed within the muscles provides support for the abdominal viscera and retains the normal contour of the abdomen. The consequences of lack of muscular support can be seen in conditions such as ‘prune belly syndrome’, where there is congenital absence of these muscles.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree