Patient Story
A 43-year-old man falls and presents with acute back and diffuse abdominal pain. He has had back pain on and off for years. Also, his wife notes that he has become “stooped” forward in the last few years. The radiographs show flowing ligamentous ossification and syndesmophyte formation about the cervical, thoracic, and lumbar spine consistent with ankylosing spondylitis (bamboo spine) (Figure 98-1). The KUB (kidneys, ureters, bladder) view film also shows fusion of the sacroiliac joints consistent with ankylosing spondylitis (Figure 98-2). No fracture, dislocation, or abdominal pathology is identified. The patient’s symptoms are treated and nonsteroidal antiinflammatory drugs (NSAIDs) are started. On follow-up a blood test reveals that he is human leukocyte antigen (HLA)-B27-positive.
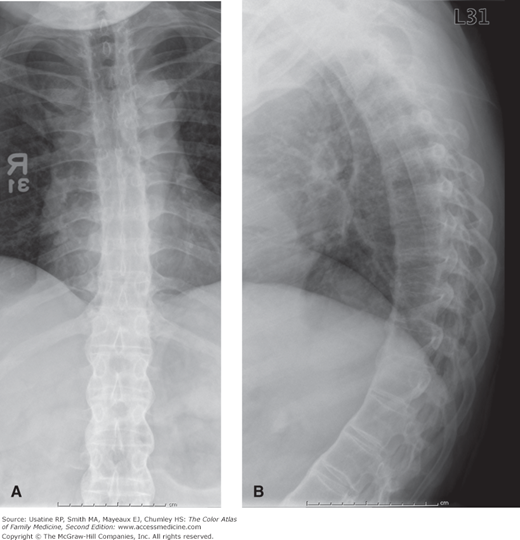
Figure 98-1
A. Fusion of the vertebral bodies and posterior elements gives the spine the classic “bamboo” appearance seen in ankylosing spondylitis. B. Note the marked kyphosis and the syndesmophytes that are the thin vertical connections between the anterior aspects of the vertebral bodies. They are located in the outer layers of the annulus fibrosis. (Courtesy of Richard P. Usatine, MD.)
Introduction
Epidemiology
- Prevalence in general population is approximately 0.2% to 0.5%.
- Five percent of patients in primary care with low back pain have a spondyloarthritis, a spectrum of diseases that includes ankylosing spondylitis.1
- More common in males than in females (approximate ratio: 4:1).
- Ninety percent of patients are HLA-B27-positive.2 However, many people with HLA-B27 do not develop the disease.
Etiology and Pathophysiology
Diagnosis
Mean delay of 7 to 8 years until diagnosis. Consider screening patients younger than 45 years of age with chronic low back pain for more than 3 months.3
- Younger patient (younger than 40 years of age at start of disease).
- Inflammatory (pain and stiffness worsen with immobility and improve with motion; symptoms are worse at night or early morning).
- Good response to NSAIDs—Sensitivity = 77%, specificity = 85%, positive likelihood ratio (LR+) 5.1.1
- Symptoms of inflammatory back pain have fair sensitivity (75%) and specificity (75%). LR+ 3.1. Number needed to screen is 7.1,3
- Limited range of motion of the spine.
- Tenderness over the spine and sacroiliac joints.
- In the advanced stages, kyphosis may occur with a stooped posture (Figure 98-1).
- Uveitis of the eye is the most common extraarticular manifestation occurring in 20% to 30% of patients. This can present with a red painful eye along with photophobia. The involved eye may have an irregular pupil and a 360-degree perilimbal injection (see Chapter 18, Uveitis and Iritis).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree