Ampullary Adenocarcinoma and Variants
Mari Mino-Kenudson, MD
Key Facts
Terminology
Ampullary adenocarcinoma comprises both adenocarcinomas arising in ampullary region and periampullary duodenal adenocarcinomas
Clinical Issues
5-year survival rate after surgical resection is approximately 50%
Significantly better than that of pancreatic adenocarcinoma
Macroscopic Features
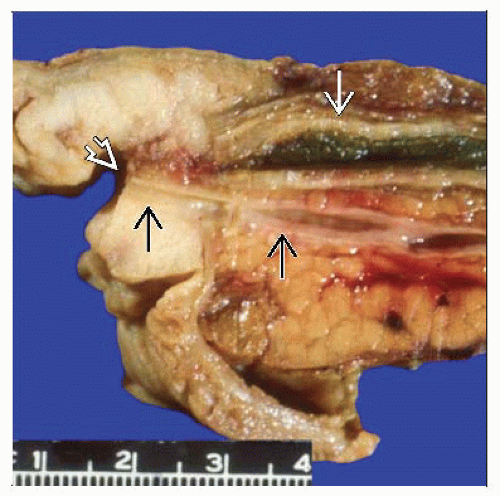
Tumors may be intraampullary, periampullary duodenal, mixed exophytic, or mixed ulcerated
Microscopic Pathology
Intestinal type
Pancreatobiliary type
Papillary carcinoma (noninvasive)
Invasive papillary carcinoma
Mucinous (colloid) carcinoma
Adenosquamous carcinoma
Ancillary Tests
Intestinal type usually positive for CK20 and CDX2; often negative for CK7
Pancreatobiliary type usually positive for CK7; often negative for CK20 and CDX2
Diagnostic Checklist
Intestinal type of histologic differentiation is associated with favorable outcome in comparison to pancreatobiliary type
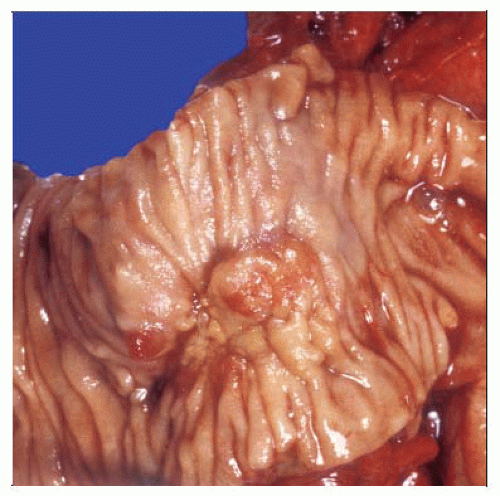 From the luminal aspect of this resection specimen, the ampulla is replaced by a protruding tumor grossly involving the duodenal mucosa of the papilla and periampullary duodenum. |
TERMINOLOGY
Synonyms
Periampullary adenocarcinoma
Definitions
Adenocarcinoma arising in ampullary region and periampullary duodenal adenocarcinoma are collectively termed “ampullary adenocarcinoma”
Approximately 90% of all carcinomas of region
CLINICAL ISSUES
Epidemiology
Incidence
Relatively uncommon
Approximately 0.2% of GI tract malignancies
Ampulla is most common site of small bowel adenocarcinoma
Age
Most common in 7th-8th decade of life
Patients with familial adenomatous polyposis develop ampullary carcinoma at younger age than patients with sporadic cases
Gender
Slightly more common in men (M:F = 1.48:1)
Presentation
Jaundice
Weight loss
Abdominal pain
Distended, palpable gallbladder (Courvoisier sign)
Treatment
Resection (Whipple procedure)
Resectability is approximately 60%
Role of adjuvant chemoradiation therapy (5-FU based) is controversial
Prognosis
5-year survival rate after surgical resection is approximately 50%
Significantly better than that of pancreatic adenocarcinoma
Comparable to that of duodenal adenocarcinoma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree