Objectives
- Define the contributors to the level of ammonia in the circulation, and explain why a mechanism for disposal of this metabolite is needed
- Outline the pathways that lead to ammonia production in the intestinal lumen
- Describe extraintestinal sources of ammonia
- Outline the pathways that lead to ammonia production in the intestinal lumen
- Describe the metabolic steps involved in the conversion of ammonia to urea in the hepatocyte
- Understand the routes for eventual disposal of urea
- Explain the consequences of excessive ammonia in the circulation, and the disease states that can lead to this outcome
- Discuss treatments for hepatic encephalopathy
Basic Principles of Ammonia Metabolism
 Ammonia (NH3) is a small metabolite that results predominantly from protein and amino acid degradation. It is highly membrane-permeant and readily crosses epithelial barriers in its nonionized form.
Ammonia (NH3) is a small metabolite that results predominantly from protein and amino acid degradation. It is highly membrane-permeant and readily crosses epithelial barriers in its nonionized form.
 Ammonia does not have a physiologic function. However, it is important clinically because it is highly toxic to the nervous system. Because ammonia is being formed constantly from the deamination of amino acids derived from proteins, it is important that mechanisms exist to provide for the timely and efficient disposal of this molecule. The liver is critical for ammonia catabolism because it is the only tissue in which all elements of the urea cycle, also known as the Krebs–Henseleit cycle, are expressed, providing for the conversion of ammonia to urea. Ammonia is also consumed in the synthesis of nonessential amino acids, and in various facets of intermediary metabolism.
Ammonia does not have a physiologic function. However, it is important clinically because it is highly toxic to the nervous system. Because ammonia is being formed constantly from the deamination of amino acids derived from proteins, it is important that mechanisms exist to provide for the timely and efficient disposal of this molecule. The liver is critical for ammonia catabolism because it is the only tissue in which all elements of the urea cycle, also known as the Krebs–Henseleit cycle, are expressed, providing for the conversion of ammonia to urea. Ammonia is also consumed in the synthesis of nonessential amino acids, and in various facets of intermediary metabolism.
Ammonia Formation and Disposition
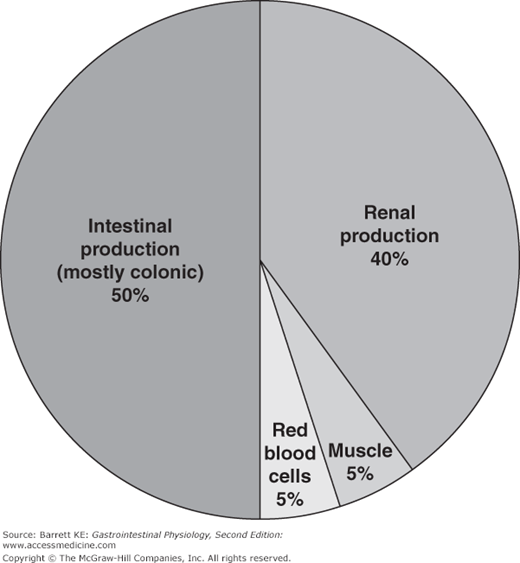
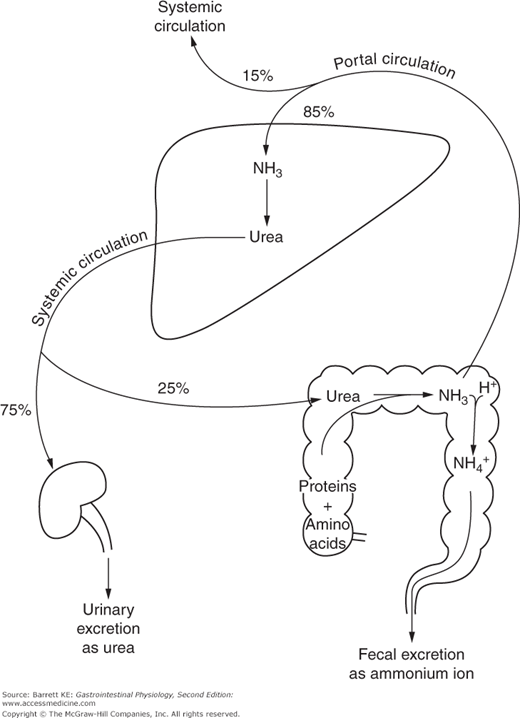
Ammonia in the circulation originates in a number of different sites. A diagram showing the major contributors to ammonia levels is shown in Figure 14–1. Note that the liver is efficient in taking up ammonia from the portal blood in health, leaving only approximately 15% to spill over into the systemic circulation (Figure 14–2).
 The major contributor to plasma ammonia is the intestine, supplying about 50% of the plasma load. Intestinal ammonia is derived via two major mechanisms. First, ammonia is liberated from urea in the intestinal lumen by enzymes known as ureases. Ureases are not expressed by mammalian cells, but are products of many bacteria, and convert urea to ammonia and carbon dioxide. Indeed, this provides the basis for a common diagnostic test, since H. pylori, which colonizes the gastric lumen and has been identified as a cause of peptic ulcer disease, has a potent urease. Therefore, if patients are given a dose of urea labeled with carbon-13, rapid production of labeled carbon dioxide in the breath is suggestive of infection with this microorganism.
The major contributor to plasma ammonia is the intestine, supplying about 50% of the plasma load. Intestinal ammonia is derived via two major mechanisms. First, ammonia is liberated from urea in the intestinal lumen by enzymes known as ureases. Ureases are not expressed by mammalian cells, but are products of many bacteria, and convert urea to ammonia and carbon dioxide. Indeed, this provides the basis for a common diagnostic test, since H. pylori, which colonizes the gastric lumen and has been identified as a cause of peptic ulcer disease, has a potent urease. Therefore, if patients are given a dose of urea labeled with carbon-13, rapid production of labeled carbon dioxide in the breath is suggestive of infection with this microorganism.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree