Alternative Vein Bypass
Allen D. Hamdan
Amy R. Evenson
Introduction
Ipsilateral greater saphenous vein (I-GSV) is the conduit of choice for lower extremity bypass procedures, especially bypasses to tibial or pedal target vessels. Given the utility of this conduit in coronary artery bypass grafting (CABG) and the possible use of I-GSV for prior lower extremity revascularization, I-GSV may not be available for lower extremity revascularization. Contralateral GSV (C-GSV) is an excellent alternative when I-GSV is unavailable but may be unappealing in patients with arterial insufficiency in the opposite limb, especially those who have a high likelihood of requiring contralateral revascularization for limb threatening ischemia in the near future. In recent reviews, however, the subsequent need for C-GSV as conduit for CABG is only 2% to 3% over 10 years, whereas the need for use in tibial bypass is 13% at 5 years. Therefore, if C-GSV is available, its use should be considered for lower extremity revascularization. If unavailable, however, it is important to be familiar with alternative conduits for use in patients with lower extremity ischemia. Options for vascular conduit in these situations include lesser saphenous vein (LSV), prosthetic conduit (polytetrafluoroethylene, knitted polyester), upper extremity veins, or composite or sequential grafts using combinations of these options.
Alternative Conduits
The LSV may be a good choice for a short graft or as part of a composite graft using more than one vein segment. Unfortunately, the LSV is generally smaller in diameter than the GSV and not of sufficient length for femoral-to-distal vessel bypass. Harvesting the LSV for bypass is more cumbersome than GSV and requires placing the patient in the prone position first, then repositioning supine for the bypass. Alternatively, the LSV can be removed with the patient supine with the leg elevated, an approach the authors find awkward and uncomfortable. Harvesting the LSV in the supine position by raising flap from a medial, subfascial approach has also been described.
Sequential and composite grafts are used infrequently but may provide an excellent option for the patients without sufficient GSV. Curi et al. recently reported their long-term experience with GSV, composite (LSV, arm vein, superficial femoral vein), and prosthetic grafts to infrageniculate target vessels. The GSV and all-autogenous composite vein grafts demonstrated similar survival, whereas both groups were far superior to prosthetic grafts. Compared to any autologous conduit, prosthetic grafts have lower patency, higher infection rates, and worse results when they do occlude. Generally, aside from bypass to the above-knee segment of the popliteal artery, prosthetic grafts are used as a last resort.
In our practice, arm veins have been our first alternative vein conduit for distal lower extremity revascularization when GSV is unavailable. The similar size, ability to achieve adequate length, and ease of harvest allow for a great deal of flexibility when using this conduit. Success with arm vein bypass requires a thorough understanding of the anatomy and technical principles involved in harvest and preparation that are specific to the use of arm veins.
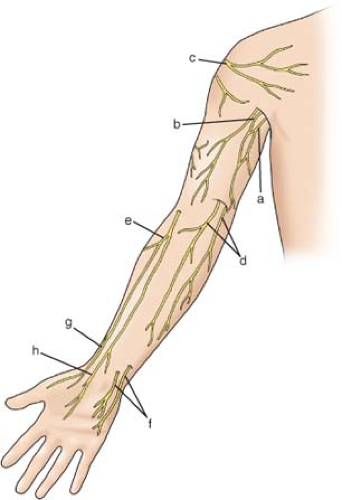
It is crucial to have a working understanding of the anatomy of the vessels and nerves of the upper extremity when the choice is made to use arm vein as a conduit for lower extremity revascularization. There is nothing more frustrating than searching for a vein when none is readily apparent and the incision has already been made (Figs. 1 and 2).
Cephalic Vein
The cephalic vein starts at the wrist on the dorsal surface of the forearm, crosses onto the anterior surface of the arm in the mid-forearm, and runs up the lateral aspect of the arm to the elbow. It is joined by multiple perforators and connects at the level of the antecubital fossa via the median cubital vein to the basilic vein. The cephalic vein then continues up the lateral aspect of the anterior upper arm to the shoulder and into the deltopectoral groove. At the level of the clavicle, the cephalic vein pierces the fascia to join the axillary vein.
Basilic Vein
The basilic vein starts posteriorly on the medial forearm receiving multiple perforators before connecting to the cephalic vein via the median cubital vein. The basilic vein then extends up the medial aspect of the upper arm into the axilla and is joined by multiple branches draining the shoulder girdle to form the axillary vein. Due to its posterior location on the forearm, harvest of this portion can be challenging and often requires two surgeons. The upper arm basilic vein is much more easily removed by a single surgeon.
 Fig. 1. Veins of the arm: cephalic vein (a); basilic vein (b); median cubital vein (c); and median antebrachial vein (d). |
Venous Relations to the Nerves of the Upper Extremity
The cephalic and basilic veins course in the cutaneous plane of the arm superficial to the fascia overlying the muscular compartments. During dissection of these vessels, a number of superficial nerves are encountered. The
distal cephalic vein is in close proximity to the superficial branch of the radial nerve at the level of the wrist. In the mid-forearm, the cephalic vein runs among the branches of the lateral antebrachial cutaneous nerve, a branch of the musculocutaneous nerve. In the upper arm, the cephalic vein crosses branches of the inferior and superior lateral brachial cutaneous nerves, whereas at the level of the shoulder, it is deep to branches of the supraclavicular nerves. The basilic vein runs in proximity to the anterior and posterior branches of the medial antebrachial cutaneous nerves throughout its course in the forearm and upper arm. At the level of the axilla, the vein runs deep to the intercostobrachial and medial brachial cutaneous nerves. Careful dissection is required to avoid damaging the many nerves found in the course of these vessels and the resultant paresthesias, numbness, or neuroma formation that may accompany their injury.
distal cephalic vein is in close proximity to the superficial branch of the radial nerve at the level of the wrist. In the mid-forearm, the cephalic vein runs among the branches of the lateral antebrachial cutaneous nerve, a branch of the musculocutaneous nerve. In the upper arm, the cephalic vein crosses branches of the inferior and superior lateral brachial cutaneous nerves, whereas at the level of the shoulder, it is deep to branches of the supraclavicular nerves. The basilic vein runs in proximity to the anterior and posterior branches of the medial antebrachial cutaneous nerves throughout its course in the forearm and upper arm. At the level of the axilla, the vein runs deep to the intercostobrachial and medial brachial cutaneous nerves. Careful dissection is required to avoid damaging the many nerves found in the course of these vessels and the resultant paresthesias, numbness, or neuroma formation that may accompany their injury.
In deciding which configuration of arm vein will be used for a specific bypass procedure, a number of factors must be considered. The characteristics of the various upper arm veins provide some guidance. In most patients, the cephalic vein is longer than the basilic vein especially when removed in its entirety, including the segment in the delto-pectoral groove. However, the cephalic vein is often damaged by intravenous catheters and phlebotomy access, resulting in significant sclerosis or webbing, especially the segment in the forearm and antecubital fossa. Additionally, the cephalic vein tends to be smaller in caliber than the basilic vein.
To select the proper arm vein conduit, it is paramount that the inflow and outflow targets are chosen ahead of time based on preoperative imaging. This requires a clear decision on both a best-case scenario for bypass (i.e., planned procedure if there was unlimited vein) as well as at least one or two alternative plans should there not be adequate conduit for the first-choice procedure that may involve originating the bypass from a more distal inflow artery or ending it at a more proximal target artery and if splicing two or more vein segments together may be necessary.
In our practice all patients having arterial bypass procedures with vein conduit undergo vein mapping using duplex ultrasound to determine vein patency as well as diameter. For patients in whom an arm vein bypass is expected, both upper extremities should be imaged including the cephalic and basilic veins. In general, vein diameters of 3 mm or greater are optimal for adequate upper extremity conduit and segments should be free of significant stenosis or stricture. Other pathology from previous vein injury may not be obvious on the duplex and requires further investigation with angioscopy at the time of surgery (see below). Some arm veins, especially the basilic vein can vary greatly in size, being quite small (1.5 mm or less) in the distal arm and become very large near the axilla (8 mm or greater) which may pose technical problems in bypasses to very small distal targets.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree