Allergic Rhinitis
KEY CONCEPTS
![]() Allergic rhinitis is a common disease. Prevention measures and treatment are justified in most cases because of the potential for complications.
Allergic rhinitis is a common disease. Prevention measures and treatment are justified in most cases because of the potential for complications.
![]() Because an immune response to allergens results in release of inflammatory mediators that cause allergic rhinitis symptoms, patients must understand the rationale for proper timing and administration of prophylactic regimens.
Because an immune response to allergens results in release of inflammatory mediators that cause allergic rhinitis symptoms, patients must understand the rationale for proper timing and administration of prophylactic regimens.
![]() Avoidance of allergens is difficult and it may be impractical to expect full success.
Avoidance of allergens is difficult and it may be impractical to expect full success.
![]() Antihistamines offer an effective option for treating both seasonal and persistent allergic rhinitis.
Antihistamines offer an effective option for treating both seasonal and persistent allergic rhinitis.
![]() Intranasal steroids are highly effective in patients who use them properly.
Intranasal steroids are highly effective in patients who use them properly.
![]() While immunotherapy is the only disease-modifying treatment of allergic rhinitis, expense, potential risks, and the major time commitment required make patient selection critical.
While immunotherapy is the only disease-modifying treatment of allergic rhinitis, expense, potential risks, and the major time commitment required make patient selection critical.
Allergic rhinitis involves inflammation of the nasal mucous membrane. In a sensitized individual, allergic rhinitis occurs when inhaled allergenic particles contact mucous membranes and elicit a specific response mediated by immunoglobulin E (IgE). This acute response involves the release of inflammatory mediators and is characterized by sneezing, nasal itching, and watery rhinorrhea, often associated with nasal congestion. Itching of the throat, eyes, and ears frequently accompanies allergic rhinitis.
Allergic rhinitis may be regarded as seasonal allergic rhinitis, commonly known as hay fever, or persistent allergic rhinitis (formerly known as perennial rhinitis). Seasonal rhinitis occurs in response to specific allergens usually present at predictable times of the year, during plants’ pollination (typically the spring or fall). Seasonal allergens include pollen from trees, grasses, and weeds. Persistent allergic rhinitis is a year-round disease caused by nonseasonal allergens, such as house dust mites, animal dander, and molds, or multiple allergic sensitivities. It typically results in less variable, chronic symptoms. Many patients have a combination of these two types of allergic rhinitis, with symptoms year-round and seasonal exacerbations.
EPIDEMIOLOGY
![]() Allergic rhinitis is one of the most common medical disorders found in humans, affecting 400 million people worldwide.1 It is the second leading cause of chronic disease in the United States, affecting one person in every four households.2 In the populations of Europe, United States, Australia, and New Zealand, the prevalence of an IgE sensitization to aeroallergens measured by allergen-specific IgE in serum or skin tests is more than 40% to 50%.3 Patients may be limited in their ability to carry out normal daily functions; higher levels of general fatigue, mental fatigue, anxiety, depressive disorders, and learning disabilities (secondary to sleep loss and fatigue) are possible.
Allergic rhinitis is one of the most common medical disorders found in humans, affecting 400 million people worldwide.1 It is the second leading cause of chronic disease in the United States, affecting one person in every four households.2 In the populations of Europe, United States, Australia, and New Zealand, the prevalence of an IgE sensitization to aeroallergens measured by allergen-specific IgE in serum or skin tests is more than 40% to 50%.3 Patients may be limited in their ability to carry out normal daily functions; higher levels of general fatigue, mental fatigue, anxiety, depressive disorders, and learning disabilities (secondary to sleep loss and fatigue) are possible.
In addition, the impact of allergic rhinitis goes well beyond these CNS issues. Allergic rhinitis is associated with several other serious medical conditions, including asthma, chronic rhinosinusitis, otitis media, nasal polyposis, respiratory infections, and orthodontic malocclusions.
ETIOLOGY
The development of allergic rhinitis is determined by genetics, allergen exposure, and the presence of other risk factors. A family history of allergic rhinitis, atopic dermatitis, or asthma suggests that rhinitis is allergic. The risk of developing allergic disease appears to increase if one parent is atopic and further increases if two are allergic; however, small sample sizes and the lack of reproducibility prevent generalization.3
Allergen exposure is another necessary factor. For allergic rhinitis to occur, an individual must be exposed over time to a protein that elicits the allergic response in that individual. Many potential sufferers never develop symptoms because they do not come into contact with the allergen that would produce symptoms in them.
Evidence suggests microbial exposure in the first years of life could help prevent allergic disease by stimulating a nonatopic immune response.4 Farm children are exposed to higher concentrations of endotoxin, derived from cell walls of gram-negative bacteria, in barns and dust around the farmhouse. Consumption of nonpasteurized farm milk may cause further exposure. These observations have led to the idea that allergic disease could be prevented by proactively increasing exposure to harmless bacteria early in life (see Alternative Treatment Options below). This could explain why positive skin tests indicating allergen sensitization have been observed more frequently for people in higher socioeconomic classes and for people who live in suburban areas.
Other predisposing factors include an elevated serum IgE (>100 international units/mL [>100 kIU/L]) before the age of 6 years, eczema, and heavy exposure to secondhand cigarette smoke.5
Allergens
Allergens that produce seasonal rhinitis include protein components of airborne pollen grains, often enzymes, from a variety of trees, grasses, and weeds. Ragweed and grass pollen are the most common offenders in the United States; however, this varies with the geographic region. In general, tree pollens cause symptoms in the spring, grass pollens cause symptoms in the late spring and summer, and weed pollens are the culprits from late summer through fall. Patients who are hypersensitive to all three may have overlapping problem periods and may be described as having perennial rhinitis when they are actually experiencing prolonged seasonal rhinitis. For this reason and the fact that most patients with seasonal problems are sensitive to at least some of the perennial allergens, there is little practical difference between the two types of allergic rhinitis. To complicate matters further, the antigenic components of many grasses—including fescue, Kentucky bluegrass, orchard, redtop, and timothy—cross-react extensively. By contrast, most tree allergens are antigenically distinct. Trees with allergenic pollen include ash, beech, birch, cedar, hickory, maple, oak, poplar, and sycamore. Flowering plants that depend on insect pollination do not cause allergic rhinitis because their pollen is too heavy and sticky and is not carried in the air.
Smaller mold spores are also important but cause allergy much less frequently. Various spores are present year-round; however, mold growth on decaying vegetation increases seasonally. Just walking through uncut fields or raking leaves can increase exposure. Thus, mold spores can be responsible for both perennial and seasonal allergies.
Indoor allergens are always present. Most important among these are house-dust mite fecal proteins, animal dander, cockroaches, and certain mold species. Dust mite levels are on the rise, possibly because of the construction of energy-efficient homes and offices with reduced ventilation and increased humidity, use of wall-to-wall carpeting, and the popularity of cool-water detergents and cold-water washing.3
PATHOPHYSIOLOGY
Knowledge of nasal physiology aids in the understanding of allergic rhinitis. The nose performs three “air conditioning” functions to prepare incoming gases for the lungs. During the fraction of a second that air is in the nose, it is heated, humidified, and cleaned. The cleaning process plays a role in the development of allergic rhinitis. As the air passes through the nose, the turbulence throws particulate matter against a mucous blanket. The rhythmic movements of the nasal cilia cause the mucous blanket to move posteriorly at approximately 9 mm/min, where it is eventually swallowed; thus, trapped foreign particles are removed via the GI tract and do not reach the lungs. It also concentrates foreign protein material into the posterior nasopharynx, where lymph tissues identify them and produce most of the allergic antibody that drives allergic rhinitis.
The vascular tissue in the nose is erectile. Stimulation of sympathetic fibers causes vasoconstriction, reduction in erectile tissue size and the size of the membranes and turbinates, and airway widening. Parasympathetic stimulation causes opposite effects.
Mast cells, in the nasal membranes, participate in the regulation of nasal patency by releasing mediators such as histamine. These are described below.
Immune Response to Allergens
![]() Allergic reactions in the nose are mediated by antigen–antibody responses when allergens interact with specific IgE molecules bound to nasal mast cells and basophils. In allergic people, these cells are increased in both number and reactivity. During inhalation, airborne allergens enter the nose and are processed by lymphocytes, which produce antigen-specific IgE, thereby sensitizing genetically predisposed hosts to those agents. Upon nasal reexposure, IgE bound to mast cells interacts with airborne allergen, triggering release of inflammatory mediators in vastly increased quantities (Fig. 76–1).6
Allergic reactions in the nose are mediated by antigen–antibody responses when allergens interact with specific IgE molecules bound to nasal mast cells and basophils. In allergic people, these cells are increased in both number and reactivity. During inhalation, airborne allergens enter the nose and are processed by lymphocytes, which produce antigen-specific IgE, thereby sensitizing genetically predisposed hosts to those agents. Upon nasal reexposure, IgE bound to mast cells interacts with airborne allergen, triggering release of inflammatory mediators in vastly increased quantities (Fig. 76–1).6
FIGURE 76-1 Allergen sensitization and the allergic response. A. Exposure to antigen stimulates IgE production and sensitization of mast cells with antigen-specific IgE antibodies. B. Subsequent exposure to the same antigen produces an allergic reaction when mast cell mediators are released.
Both immediate and late-phase reactions are observed after allergen exposure. The immediate reaction occurs within seconds to minutes, resulting in the rapid release of preformed mediators and newly generated mediators from the arachidonic acid cascade as the mast cell membrane is disturbed (Table 76–1). These mediators of immediate hypersensitivity include histamine, some leukotrienes, prostaglandin D2, tryptase, and kinins.6 In addition, the mast cell has been found to be a source of several cytokines that probably are relevant to the chronicity of the mucosal inflammation that characterizes allergic rhinitis.7 Sensory nerve stimulation produces itching, and sneezing occurs via reflex stimulation of efferent vagal pathways. Neuropeptides substance P and calcitonin gene-related peptide from nonadrenergic, noncholinergic nerves affect vascular engorgement directly and via modulation of sympathetic tone. Histamine produces rhinorrhea, itching, sneezing, and obstruction, with the obstruction only partially blocked by H1– or H2-blocking agents.8 Nasal obstruction is also caused by kinins, prostaglandin D2, and leukotrienes C4/D4. Kinins, when directly administered, produce pain rather than itching.9 These inflammatory mediators also produce vasodilation, increased vascular permeability, and production of increased nasal secretions.10
TABLE 76-1 Mast Cell Mediators
Four to 8 hours after the initial exposure to an allergen, a late-phase reaction occurs symptomatically in 50% of allergic rhinitis patients.11 This response, thought to be caused by cytokines released primarily by mast cells and thymus-derived helper lymphocytes, is characterized by profound infiltration and activation of migrating cells. This inflammatory response likely is responsible for the persistent, chronic symptoms of allergic rhinitis, including nasal congestion. The inflamed mucosa becomes hyperresponsive, a state characterized by exacerbation of nasal reactions to non-specific or irritant triggers. In this state, the patient also reacts to increasingly lower amounts of the same allergen.12 The process also causes significant increases in non-specific irritability (as seen in asthma) and the notion among patients that they have become “allergic to everything.”
CLINICAL PRESENTATION
The patient with allergic rhinitis typically complains of clear rhinorrhea, paroxysms of sneezing, nasal congestion, postnasal drip, and pruritic eyes, ears, nose, or palate. Symptoms of allergic conjunctivitis are associated more frequently with seasonal than perennial allergic rhinitis, because a majority of the perennial allergens, such as dust mites and molds, are indoors, where air velocity is too low for substantial deposition of allergenic particles on the conjunctivae. However, with heavy exposure from animal or mold allergens, allergic conjunctivitis can be pronounced.
Symptoms secondary to the late-phase reaction, predominantly nasal congestion, begin 3 to 5 hours after antigen exposure and peak at 12 to 24 hours. Subsequent symptoms, both allergic and irritant, are elicited more easily because of the priming effect. For instance, a ragweed-sensitive patient, when exposed to ragweed pollen out of season, responds with modest symptoms and may be very tolerant of irritants such as air pollution or tobacco smoke. During the ragweed season, however, when the nasal mucosa is already inflamed, exposure to small doses of pollen or to irritants to which the patient is usually tolerant elicits a response clinically indistinguishable from the patient’s allergy.
Diagnostic Considerations
Allergic rhinitis is distinguished from other causes of rhinitis by a thorough history, physical examination, and certain diagnostic tests. The medical history consists of a careful description of symptoms, environmental factors and exposures, results of previous therapy, use of other medications, previous nasal injuries, previous nasal or sinus surgery, family history, and the presence of other medical problems and medications. Historical identification of specific causative allergens may be difficult. For example, a reaction induced by mowing the lawn may not be caused by grass pollens but may be caused by the disturbance of various weeds, molds, or other plants in the lawn. With perennial allergic rhinitis, the cause–effect and temporal relationships are less clear, making the diagnosis of specific causes more difficult, especially with such covert allergens as house dust mites and molds.
In children, physical examination may reveal allergic shiners—a transverse nasal crease caused by repeated rubbing of the nose—and adenoidal breathing. Pale, bluish, edematous nasal turbinates coated with thin, clear secretions are characteristic of a purely allergic reaction. Tearing, conjunctival injection and edema, and periorbital swelling may be present. Physical findings are generally less clear-cut for adults.
Nasal scrapings will provide a representative sample of cells infiltrating the nasal mucosa and can be helpful in supporting the diagnosis.13 Microscopic examination of the nasal smear from an allergic individual typically will show numerous eosinophils. The blood eosinophil count may be elevated in allergic rhinitis, but it is nonspecific and has limited usefulness.14
Allergy testing can help determine whether a patient’s rhinitis is caused by an allergen. Immediate-type hypersensitivity skin tests are used for the diagnosis of allergic rhinitis. These include skin tests performed by the percutaneous route, where the diluted allergen is pricked or scratched into the skin surface, or by the intradermal route, where a small volume (0.01 to 0.05 mL) of diluted allergen is injected between the layers of skin. Percutaneous tests are more commonly performed and are safer and more generally accepted, with intradermal tests reserved for patients requiring confirmation in special circumstances.
In all allergy testing, a positive control (histamine) and a negative control are essential for correct interpretation. After 15 minutes of the application of the allergen, the site is examined for a positive reaction (defined as a wheal-and-flare reaction). Because correct testing is done with extremely minute doses, undetectable by nonsensitized individuals, this reaction is evidence of the presence of mast cell-bound IgE specific to the allergen tested. Many, but not all, common allergens are available as standardized allergenic extracts.
Antihistamines and a few other medications interfere with the wheal-and-flare reaction. First-generation antihistamines should be stopped at least 3 to 5 days before testing, and second-generation, nonsedating antihistamines should be stopped for 10 days before testing.15 Medications with antihistamine properties (e.g., sympathomimetic agents, phenothiazines, and tricyclic antidepressants) should be discontinued if possible before skin testing.
The radioallergosorbent test (RAST) was the first commonly used method for detecting IgE antibodies in the blood that are specific for a given allergen. Several other quantitative assays that include a reference curve calculated against standardized IgE are available. These tests are highly specific but may be slightly less sensitive than percutaneous tests.
Complications
Not only is allergic rhinitis aggravating, it frequently leads to further complications, particularly if the patient does not receive adequate treatment. Symptoms of untreated rhinitis may lead to disturbed sleep, chronic malaise, fatigue, and poor work or school performance. Patients often are plagued by loss of smell or taste, with sinusitis or polyps underlying many cases of allergy-related hyposmia. Postnasal drip with cough, hoarseness, and even vocal polyps also can be bothersome.
The role of allergic rhinitis in the development of acute otitis media or chronic middle ear effusion is often less clear. Children with allergic rhinitis appear to be at greater risk of these conditions because of nasal obstruction and negative middle ear pressure. Hearing problems in children related to middle ear effusion may lead to delayed development of language in young children or to school problems in older children.
Permanent facial disfigurement can result from chronic allergic rhinitis.16 The chronic edema and venous stasis may contribute to the development of a high-arched, V-shaped palate. Mouth breathing caused by nasal obstruction can be responsible for dental malocclusion and orthodontic problems. Constant upward rubbing of the nose (allergic salute) can cause a transverse crease across the lower nose; nasal congestion often leads to venous pooling and dark circles under the eyes known as allergic shiners.
Allergic rhinitis is clearly associated with asthma. The prevalence of asthma in patients without rhinitis is <2%, while the prevalence of asthma in patients with rhinitis is 10% to 40%.17 It is not known if allergic rhinitis is an early clinical manifestation of asthma or if the nasal disease itself is causative for asthma.
Recurrent sinusitis and chronic sinusitis are relatively common complications of allergic rhinitis. The structure of the mucus blanket breaks down, with decreased water production by serous glands, leaving hair cells trapped in the thicker mucus layer. This greatly reduces the clearance of trapped bacteria and offers ideal breeding grounds for the bacteria. Nasal polyps are less common but nonetheless bothersome; they require specific therapy but may improve with management of the underlying allergic state. Epistaxis also can be a problem; it is related to mucosal hyperemia and inflammation.
TREATMENT
A number of options exist for the treatment of allergic rhinitis, both nonpharmacologic and pharmacologic. Many of the pharmacologic options are available over-the-counter requiring that patients receive guidance in the selection process by a healthcare professional to obtain the most appropriate therapy. Both over-the-counter and prescription choices must be guided by patient-specific symptomatology and patient characteristics as described in this chapter.
Desired Outcomes
The therapeutic goal for patients with allergic rhinitis is to minimize or prevent symptoms and prevent long-term complications. This goal should be accomplished with no or minimal adverse medication effects and reasonable medication expenses. The patient should be able to maintain a normal lifestyle, including participating in outdoor activities, yard work, and playing with pets as desired.
General Approach to Treatment
Once the causative allergens and the specific symptoms are identified, management consists of three possible approaches: (a) allergen avoidance, (b) pharmacotherapy for prevention or treatment of symptoms, and (c) specific immunotherapy. The pharmacotherapy for symptoms approach includes several options that are based on patient-specific information (Table 76–2). Figure 76–2 depicts an algorithm for treatment options.
TABLE 76-2 Pharmacotherapeutic Options for Allergic Rhinitis
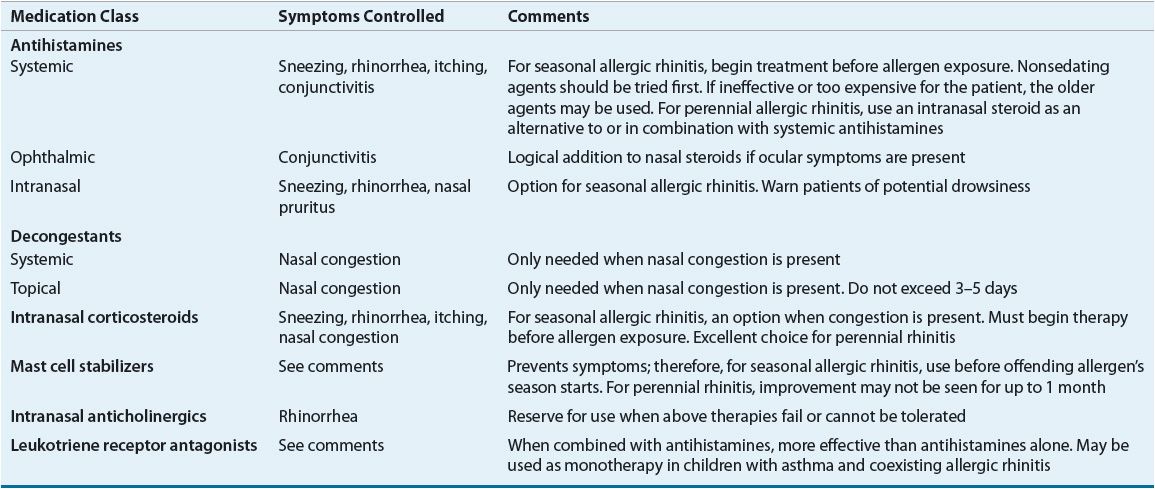
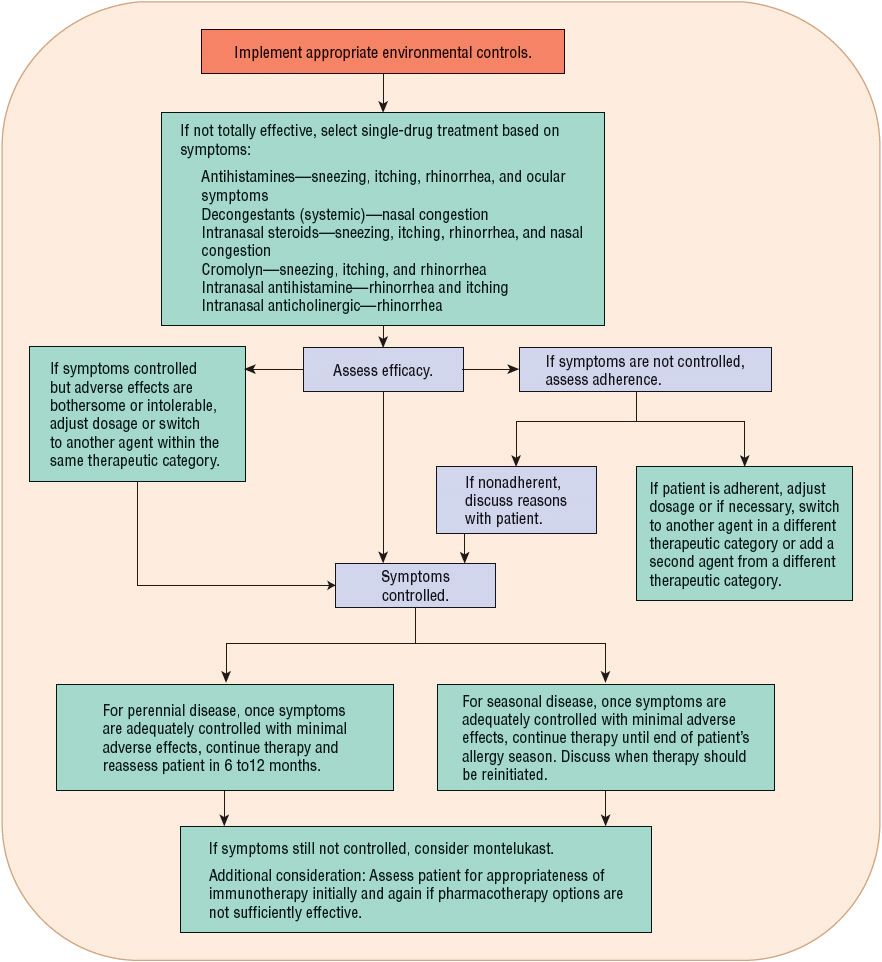
FIGURE 76-2 Treatment algorithm for allergic rhinitis.
Nonpharmacologic Therapy
![]() Avoidance of offending allergens is the most direct method of preventing allergic rhinitis, but it is often the most difficult to accomplish, especially for perennial allergens. Mold growth can be reduced by maintaining household humidity below 50% and removing obvious growth with bleach or disinfectant. Patients sensitive to animals will benefit most by removing pets from the home18; however, most animal lovers are reluctant to comply with this approach. Dog and cat allergens may produce symptoms in sensitized individuals.7 After removing a cat from the home, it may take as long as 20 weeks for the home to reach allergen levels of a pet-free home. Washing cats weekly may reduce allergens but studies are inconclusive.7 Some dogs display antigens more profusely than do others; clinically, a sensitized person may tolerate one animal better than another.
Avoidance of offending allergens is the most direct method of preventing allergic rhinitis, but it is often the most difficult to accomplish, especially for perennial allergens. Mold growth can be reduced by maintaining household humidity below 50% and removing obvious growth with bleach or disinfectant. Patients sensitive to animals will benefit most by removing pets from the home18; however, most animal lovers are reluctant to comply with this approach. Dog and cat allergens may produce symptoms in sensitized individuals.7 After removing a cat from the home, it may take as long as 20 weeks for the home to reach allergen levels of a pet-free home. Washing cats weekly may reduce allergens but studies are inconclusive.7 Some dogs display antigens more profusely than do others; clinically, a sensitized person may tolerate one animal better than another.
Evidence to support avoidance measures for house dust mites suggests that accepted notions for reducing exposure have little practical effect.18 While some evidence shows allergen levels can be reduced by washing bedding on a hot cycle, replacing carpets with hard flooring and using vacuum cleaners with HEPA filters, there is no documented evidence for a clinical benefit. Only encasing bedding in impermeable covers has some clinical benefit in children but not adults. Future studies are needed to determine if environmental control of allergens may be helpful in forestalling further rhinitis and preventing later asthma.
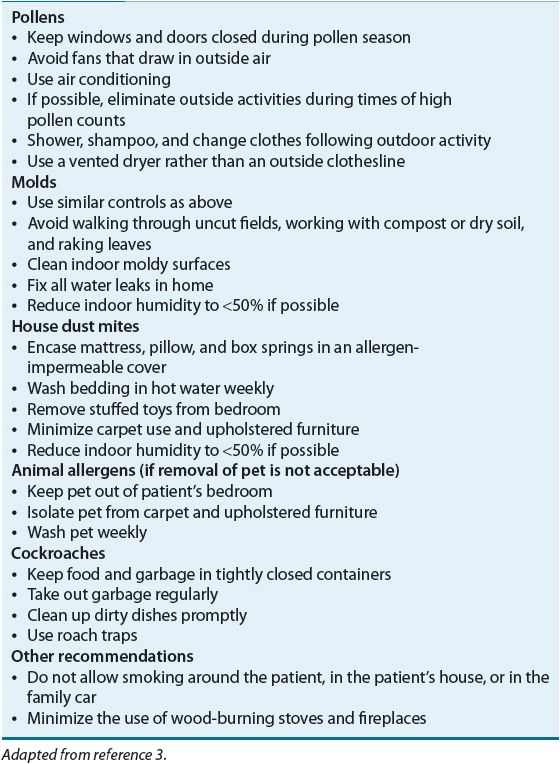
General recommendations have been made to prevent poor air quality in homes.19 Steps include avoiding wall-to-wall carpeting, using moisture control to prevent the accumulation of molds, and controlling sources of pollution such as cigarette smoke. Patients with seasonal allergic rhinitis should keep windows closed and minimize time spent outdoors during pollen seasons. Immediate hair washing and change of clothes are recommended upon returning indoors. Use of fans that direct outside air into the house should be avoided. Filter masks can be worn while gardening or mowing the lawn. Avoidance of upholstery and stuffed toys in the bedroom are easy steps to accomplish. Table 76–3 summarizes recommendations for environmental control. While these steps are logical, there is little existing evidence that environmental control measures provide clinical benefit. These measures are intended to be a part of a comprehensive treatment strategy that will likely include pharmacotherapy and, in selected cases, immunotherapy.
TABLE 76-3 Environmental Controls to Prevent Allergic Rhinitis