TABLE 46-1 CAGE Questionnaire
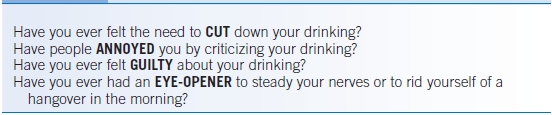
TABLE 46-2 Alcohol Use Disorders Identification Test
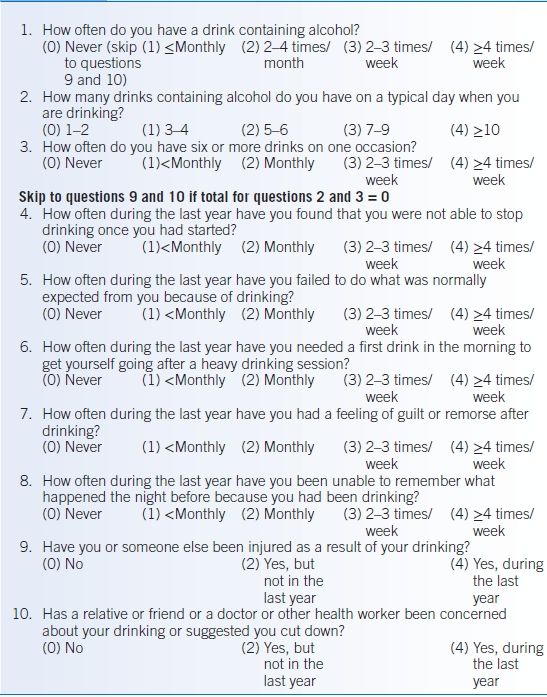
Total score ≥8 indicates hazardous and harmful alcohol use, as well as possible alcohol dependence (≥7 for women and men >65 years).Modified from Babor TF, Higgins-Biddle JC, Saunders JB, et al. AUDIT. The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care, 2nd ed. Geneva, Switzerland: World Health Organization Department of Mental Health and Substance Dependence; 2001.
TABLE 46-3 AUDIT-C Questionnaire
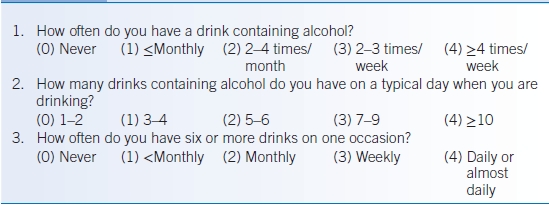
Scoring: ≥4 points for men or ≥3 points for women constitutes a positive screen.
TREATMENT
- The first step in treating patients with alcohol abuse and dependence is making the patient aware that they have a disease. This should be done in an empathic and nonjudgmental manner.
- Patients must be willing to change. The physician must listen to the patient and assess their readiness and willingness to change.
- Involving family members and friends is a good strategy to ensure that the patient has a strong support network when they leave the office. This should not be done without approval of the patient.
- Brief interventions have been shown to reduce alcohol consumption.17
- Physicians should remember the Five As when conducting a brief intervention8,18:
- Ask: Ask about alcohol use (see the “Diagnosis” section).
- Advise: Advise patients that their drinking puts them at high risk for alcoholism and alcohol-related problems. The specific effects of high-risk drinking should be explained.
- Assess: Assess the patient’s readiness to change and advise accordingly (see below).
- Assist: Provide specific self-help information.
- Arrange: Arrange follow-up.
- Ask: Ask about alcohol use (see the “Diagnosis” section).
- Although not without critics, the Prochaska transtheoretical model of stages of change is relatively well known to many clinicians, and may serve to provide some very general guidelines regarding how much and what type of effort to invest.19,20 To some extent, the dividing lines between stages are arbitrary, individuals may not progress in a sequential manner between the stages, and the stages may not be mutually exclusive.
- Precontemplation stage: The person is unaware or underaware of the problem and has no intention of changing the behavior. The physician’s role is to advise the patient about the need to reduce alcohol consumption and the hazards of drinking. The counseling can be quite brief, just a minute or two, but should be repeated at every visit.
- Contemplation stage: The patient is aware that a problem exists but is not yet ready to make a full commitment to take action. This stage may last for long periods of time. The physician’s role is to continue stressing the hazards of drinking and the benefits of behavior change. How to choose a goal can also be discussed.
- Preparation stage: The patient intends to take action in the next few months; this may be a brief stage. The physician should increase the intensity and specificity of counseling and help the patient choose a goal and give advice and encouragement. When a patient is really ready to commit to change, this should be the main focus of the office visit.
- Action stage: This is the most visible stage in which the addictive behavior is altered (for 1 day to 6 months). Review specific advice and continue to provide encouragement.
- Maintenance stage: The patient maintains the change and works to prevent relapse. This stage extends beyond 6 months and may last a lifetime. The physician should provide follow-up and continued encouragement.
- Relapse stage: This can also be termed recycle because the patient again moves through the cycle and may achieve long-term success on subsequent cycles. The physician should assist the patient in renewing the process.
- Precontemplation stage: The person is unaware or underaware of the problem and has no intention of changing the behavior. The physician’s role is to advise the patient about the need to reduce alcohol consumption and the hazards of drinking. The counseling can be quite brief, just a minute or two, but should be repeated at every visit.
- Patients should be encouraged to avoid bars and social gatherings which may strongly encourage the patient to drink, and to seek help when relapse is near. Patients must learn how to cope with stress and anxiety once they abstain from alcohol.
- Constant follow-up is an integral part of treating patients. Unfortunately, <25% of patients will stay abstinent after a year. Given this high relapse rate, physicians and patients may find treatment difficult and frustrating. Nevertheless, continued and consistent interaction with the patient is key to successful recovery.
Medications
- Disulfiram, an inhibitor of the enzyme aldehyde dehydrogenase, has been used to treat patients with AUDs once they become abstinent. Consumption of alcohol results in the accumulation of acetaldehyde and the development of symptoms including tachycardia, dyspnea, flushing, nausea, vomiting, headache, hypotension, and dizziness. Data supporting the use of disulfiram is equivocal.21,22 It may be more effective when compliance is monitored.8
- Naltrexone, an opiate antagonist, has been used in alcoholics to decrease use. Several reviews have generally supported the use of naltrexone.8,23–27 The COMBINE study found better outcomes with the addition of naltrexone to medical management.28
- Acamprosate is a structural analog of γ-amino butyric acid but its mechanism of action is not fully understood. Reviews also support its use.8,23,25,27,29 However, in the COMBINE study, acamprosate was not more effective than placebo.27,28
- Benzodiazepines, β-blockers, clonidine, and anticonvulsants have all been used to treat alcohol withdrawal.
Other Nonpharmacologic Therapies
- Brief interventions are 10 to 15 minutes patient encounters where counseling, feedback, goal setting, and follow-up are discussed. Numerous trials have shown these encounters to be effective in reducing drinking and increasing abstinence.17
- The COMBINE study also demonstrated that cognitive behavior therapy was a helpful addition to medical management.28

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


