2 Adverse drug reactions and interactions
The aim of this chapter is to introduce you to the concepts of adverse drug reactions and drug interactions and side-effects. According to the Department of Health (DH), between 5 and 17 per cent of hospital admissions are associated with adverse drug reactions (DH 2001). The likelihood of drug interactions and adverse reactions is increased in patients on more than one medicine and higher in those who take more than four medications (polypharmacy). The incidence is also increased in elderly patients. As many elderly people are on many medicines, it can be seen that they as a group are often at a higher risk of interactions and adverse reactions.
Main mechanisms of drug interactions
Drug interactions can be described as being:
- pharmacokinetic; and
- pharmacodynamic.
Pharmacokinetic interactions can occur in any of the four pharmacokinetic processes:
- absorption;
- distribution;
- metabolism;
- excretion.
Absorption
The most common absorption interactions occur when medicines are taken by the oral route. Many drugs require precise conditions for optimal absorption in the stomach and upper gastrointestinal (GI) tract. Anything which disrupts these conditions can affect drug absorption. Examples include:
- Taking medication with or after a meal: the presence of food in the stomach can delay drug absorption. Sometimes we use this to our advantage, but some drugs need to be taken on an empty stomach.
- Taking medication at the same time as an antacid preparation. Antacids such as Gaviscon coat the stomach and delay drug absorption, so taking them at the same time as some drugs must be avoided.
- Crushing or splitting tablets. Some tablets need to travel intact through the stomach before being absorbed optimally in the small intestine, or have a coating which delays their absorption. By crushing or splitting tablets we may change the rate of absorption of these drugs.
The main message is to always follow any special instructions given with oral medicines to ensure optimal absorption.
Distribution
Some drugs are bound to plasma proteins during their distribution through body fluids. The efficiency of a drug can be affected by the degree to which it binds to proteins within the blood plasma. The less a drug binds to a plasma protein, the more efficient it is in diffusing and crossing cell membranes. An example of a common blood protein that drugs can bind to would be albumin. Due to protein binding of a drug, the drug exists in two forms, namely protein bound and unbound (free), the unbound being the active component of the drug. The bound portion remains inactive unless displaced from the protein. Any medications that may displace other medicines from plasma proteins could change the level of free drug in the plasma. Drugs with this sort of interaction are usually listed as incompatible in Appendix 1 of the BNF.
Metabolism
Some drugs can interfere with the effectiveness of drug metabolizing enzymes in the liver. This can have one of two effects:
1. Enzyme inducer: this is where the drug increases the effectiveness of the enzyme and metabolizes more quickly. This means that the effectiveness of other drugs and their duration of action may be reduced.
2. Enzyme inhibitor: this is where the drug decreases the effectiveness of the enzyme and metabolizes more slowly. This means that the effectiveness of other drugs and their duration of action may be increased.
Drugs which modify metabolizing enzymes should be given with caution to patients on other medicines, and effects should be monitored. The daily presence of the pharmacist on the ward, monitoring prescriptions, while liaising with both the medical and nursing team, is of great importance in recognizing any such problems.
Excretion
Relatively few drugs have a dramatic effect on drug excretion. Non-steroidal anti-inflammatory drugs (NSAIDs) can affect the kidney tubule and modify the excretion and reabsorption of some drugs. Pharmacodynamic interactions are more common and come into two categories.
1. Additive effects of drugs with similar actions. For example, giving an angiotensin-converting enzyme (ACE) inhibitor (e.g. Lisinopril) with a diuretic (e.g. Bendro-flumethazide) may lead to an adverse drop in blood pressure.
2. Competing effects of drugs with opposite actions. For example, giving a beta blocker drug for hypertension (e.g. Propranalol) to an asthmatic patient may render their beta agonist drug (e.g. salbutamol) ineffective in managing their asthma symptoms.
Adverse drug reactions
An adverse drug reaction (ADR) (sometimes called an adverse drug event – ADE) is a reaction that is always unwanted by the patient. It is a negative event following the prescription and administration of a medication. The term ADR differs from a side-effect. This is because some side-effects can be beneficial. The study of ADRs is called pharmacovigilance.
- Type A: augmented effects.
- Type B: bizarre effects.
- Type C: chronic effects.
- Type D: delayed effects.
- Type E: end-of-treatment effects.
- Type F: failure of therapy.
The most common types of ADR are augmented and bizarre.
Type A: augmented
This is where the reaction is an augmentation of the drug’s pharmacology. This means we can often predict these reactions from our knowledge of the pharmacodynamic properties of a drug. For example, a patient on an antihypertensive drug may develop dizziness and fainting due to too great a lowering of their blood pressure. Patients on NSAIDs can develop gastric irritation due to the drug’s action on protective gastric mucous. These types of reactions are mainly dose dependent: the greater the dose of the drug, the higher the likelihood of adverse reaction. They are the most common ADRs but are associated with lower morbidity and mortality.
Type B: bizarre
This is where the reaction is wholly unexpected and could not be predicted from the pharmacodynamic properties of the drug. An example would be anaphylaxis to any drug, or a red pinprick rash with penicillin. These types of reactions are not dose dependent and can occur even at low starting doses. They are rarer than Type A ADRs but are associated with a higher morbidity and mortality.
Clinical significance of drug interactions to the patient
The significance of a drug reaction to the patient depends on many factors and can determine how health care professionals respond to the reaction. Some patients can tolerate side-effects or ADRs of medications if the benefit of the drug is greater than the inconvenience. When side-effects cannot be tolerated, this may be classed as a Type A ADR.
Type A ADR
If a patient reports an ADR there are a variety of responses. The prescriber should be informed immediately so that appropriate action can be taken. This could include:
- stopping the drug altogether;
- reducing the dose of the drug;
- switching to an alternative drug.
The ADR should always be recorded in the patient’s notes. Poor management of ADRs can lead to problems with patients adhering to their medication regimens, so this is an area that should be taken very seriously.
Type B ADR
Type B ADRs are more serious than Type A and require prompt detection and rapid action. The drug suspected of causing this reaction should be withheld and the prescriber informed immediately. Any resuscitative measures should be undertaken at once to prevent serious complications. The drug should be stopped and an alternative found where necessary. This type of ADR should always be recorded in the patient’s notes and be easily visible to any future prescriber.
All Type B and many Type A ADRs should be reported to the Medicines & Healthcare Products Regulatory Agency (MHRA) via the yellow card found in the back of the BNF or online. This allows pharmacovigilance and builds up a fuller profile of the drugs.
Pharmacovigilance is the study relating to the detection, assessment, understanding and prevention of adverse drug effects. The origin of the word is a combination of the Greek pharmakon, ‘drug’ and the Latin vigilare, ‘to keep awake or alert, to keep watch’. In common practice we are mostly concerned with side-effects of medicines that may be intolerable by our patients or cause them to have adverse effects as described above. Pharmacovigilance involves collecting, monitoring, researching, assessing and evaluating information from health care providers and patients on the adverse effects of medications with a view to:
- identifying new information about medicines to inform prescribing practice;
- preventing harm to patients.
A very helpful website in relation to this area can be found at www.mhra.gov.uk/Howweregulate/Medicines/Inspectionandstandards/GoodPharmacovigilancePractice/index.htm.
The yellow card system
The yellow card system is vital in helping the MHRA monitor the safety of the medicines and vaccines on the market. Before a medicine is granted a licence so that it can be made available in the UK, it must pass strict tests and checks to ensure that it is acceptably safe and effective. All effective medicines, however, can cause side-effects (or ADRs, see above), which can range from minor to very serious. Even if it is only a suspicion that a medicine or combination of medicines have caused a side-effect, patients and health professionals should send the MHRA a yellow card. Yellow card reports on suspected side-effects are evaluated, together with other sources of information such as clinical trial data, medical literature or data from international medicines regulators, to pinpoint previously unidentified safety issues. The MHRA will take action, whenever necessary, to ensure that medicines are used in a way that minimizes risk, while maximizing patient benefit.
Major groups of drugs involved in adverse drug reactions
Some drugs are more likely to cause ADRs than others. This means that their prescribing and administration should be closely monitored. These drug groups include:
- antibiotics;
- antipsychotics;
- NSAIDs;
- drugs with a narrow therapeutic index (e.g. warfarin and Digoxin);
- lithium;
- diuretics;
- benzodiazepines;
- newly-licensed medicines.
Many of these medications have few alternatives that are as effective for some patients, which can mean that reactions may be inevitable.
Steps in minimizing the effects of adverse drug reactions
There are a number of steps that can be taken to minimize or prevent ADRs:
- drugs should only be prescribed for a good indication, particularly during pregnancy;
- a check should be made on all previous medication;
- any previous reactions to medicines should be assessed;
- any non-drug allergies should be identified including food allergies/sensitivities or topical allergies (e.g. sticking plasters);
- other drug use should be verified, including over the counter (OTC) medications, herbal remedies and any illicit or recreational drugs taken;
- age should always be taken into consideration (e.g. is the patient elderly or a young child?);
- check for any hepatic and/or renal disease;
- always maintain yellow card reporting to uphold pharmacovigilance;
- prescribing should be according to any established protocols;
- clear instructions should always be provided regarding medication administration to the patient;
- familiar drugs should be prescribed where possible, as side-effect profiles are better known;
- always inform the patient of possible side-effects to help them identify ADRs.
- other drug use should be verified, including over the counter (OTC) medications, herbal remedies and any illicit or recreational drugs taken;
Nurses have an important role in ADR monitoring. They are well placed to spot ADRs as they are often the people administering the medication to the patient and patients may find it easier to talk to nurses about their medicines during the drug round than to the prescribing doctor. If you suspect a reaction, you must follow local policies and procedures for its reporting and management.
Anaphylaxis
Anaphylaxis is an acute multi-system severe type I hypersensitivity allergic reaction. The term comes from the Greek words ana, ‘against’, and phylaxis, ‘protection’. Anaphylactic shock or true anaphylaxisis is associated with systemic vasodilation that results in low blood pressure. It is also associated with severe bronchoconstriction to the point where the individual finds in increasingly difficult to breathe. Anaphylaxis can present with many different symptoms. These usually develop quickly over a few minutes. The most common systems affected include the skin, the respiratory system, the gastrointestinal system, the heart and vasculature, and the central nervous system. Anaphylaxis can occur in response to any allergen. Common triggers include insect bites or stings, foods, medications and latex. The most common medicines to trigger anaphylaxis are antibiotics, aspirin, ibuprofen and other analgesics.
Treatment
The Resuscitation Council (UK) issues guidelines for the treatment and management of anaphylaxis (Resuscitation Council 2008). The key points are:
Treatment of an anaphylactic reaction should be based on general life support principles:
- use the airway, breathing, circulation, disability, exposure (ABCDE) approach to recognize and treat problems;
- call for help early;
- treat the greatest threat to life first;
- initial treatments should not be delayed by the lack of a complete history or definite diagnosis.
Patients having an anaphylactic reaction in any setting should expect the following as a minimum:
- recognition that they are seriously unwell;
- an early call for help;
- initial assessment and treatments based on an ABCDE approach;
- adrenaline therapy if indicated;
- investigation and follow-up by an allergy specialist.
The full guidance can be downloaded from the Resuscitation Council website at www.resus.org.uk/pages/reaction.pdf.
Age-related adverse drug reactions
As previously noted, the elderly and the very young are at a higher risk of drug reactions and should be closely monitored when prescribed medications which have a higher incidence of drug reactions or side-effects. The elderly often have changes in sensitivity to drugs due to:
- reductions in drug binding sites;
- impaired organ function (liver/kidneys);
- altered metabolizing enzyme systems in the liver.
All of these can lead to potentiation of drug action which in turn can cause more side-effects.
Medicine-related problems are more likely to be associated with older people who:
- take four or more medicines (polypharmacy);
- take Digoxin, warfarin, NSAIDs, diuretics or benzodiazepines;
- have recently been discharged from hospital;
- have a low level of social support;
- have poor hearing, vision or dexterity;
- experience confusion, disorientation or depression.
Children cannot just be viewed as small adults when it comes to medication. They respond differently to drugs for many reasons, most of which can be related to pharmacokinetics (see Chapter 1; see also Box 2.1).
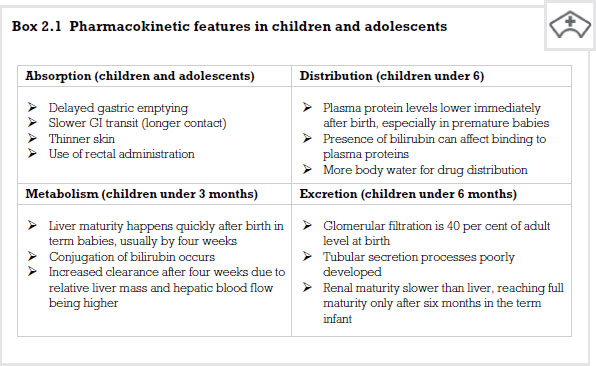
Absorption
This can be a major factor in drug problems with children under the age of 12. Delayed gastric emptying means drugs taken orally stay in the stomach longer, which can in turn delay the absorption of drugs from the small intestine. Children have a longer GI transit of gut contained materials which means drugs stay in contact with their absorbing sites for longer. Also, young children have trouble swallowing tablets and often cannot tolerate liquid medicines well.
Plasma protein levels are lower immediately after birth, especially in premature babies. This can be a problem in drugs which are extensively bound to plasma proteins. If proteins are reduced there are less sites to bind, which increases the available drug, hence effectively increasing the dose which can lead to Type A reactions.
Metabolism
Children metabolize drugs differently to adults, especially in the first few weeks of life. This can lead to higher levels of an active drug being present for longer and produces a risk of Type A reactions.
Excretion
Children’s kidneys are immature at birth and cannot efficiently process drug molecules. This leads to delays in excreting drug molecules which can continue to circulate for longer, again with a risk of Type A reactions.
All of these effects mean that children need lower doses of medicine than adults, not simply because they are smaller, but due to immaturity of many organ systems.
Doses of drugs can be increased at 6 months and slowly raised to adult doses for many drugs by the age of 12, when organ maturity is achieved.
Recommended further reading
Beckwith, S. and Franklin, P. (2007) Oxford Handbook of Nurse Prescribing. Oxford: Oxford University Press.
Brenner, G.M. and Stevens, C.W. (2006) Pharmacology, 2nd edn. Philadelphia, PA: Saunders Elsevier.
Clayton, B.D. (2009) Basic Pharmacology for Nurses, 15th edn. St Louis, MO: Mosby Elsevier.
Coben, D. and Atere-Roberts, E. (2005) Calculations for Nursing and Healthcare, 2nd edn. Basingstoke: Palgrave Macmillan.
DH (Department of Health) (2001) National Service Framework: Medicines and Older People. London: DH.
Downie, G., Mackenzie, J. and Williams, A. (2007) Pharmacology and Medicines Management for Nurses, 4th edn. Edinburgh: Churchill Livingstone.
Gatford, J.D. and Phillips, N. (2006) Nursing Calculations, 7th edn. Edinburgh: Churchill Livingstone Elsevier.
Karch, A.M. (2008) Focus on Nursing Pharmacology, 4th edn. Philadelphia, PA: Lippincott Williams & Wilkins.
Lapham, R. and Agar, H. (2003) Drug Calculations for Nurses: A Step-by-step Approach, 2nd edn. London: Arnold.
Resuscitation Council UK (2008) Emergency Treatment of Anaphylactic Reactions: Guidelines for Healthcare Providers. London: Resuscitation Council UK.
Simonson, T., Aarbakke, J., Kay, I., Coleman, I., Sinnott, P. and Lyssa, R. (2006) Illustrated Pharmacology for Nurses. London: Hodder Arnold.
Trounce, J. (2000) Clinical Pharmacology for Nurses, 16th edn. New York: Churchill Livingstone.
< div class='tao-gold-member'>