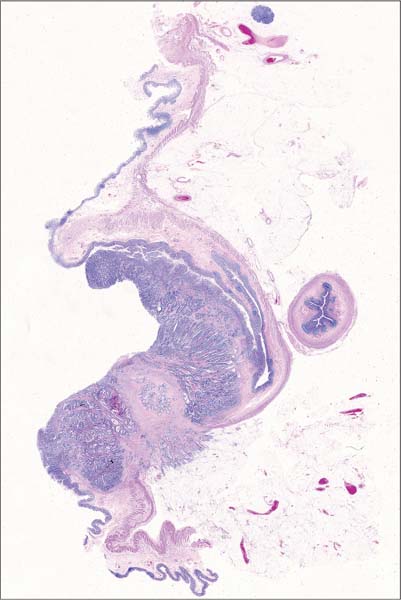
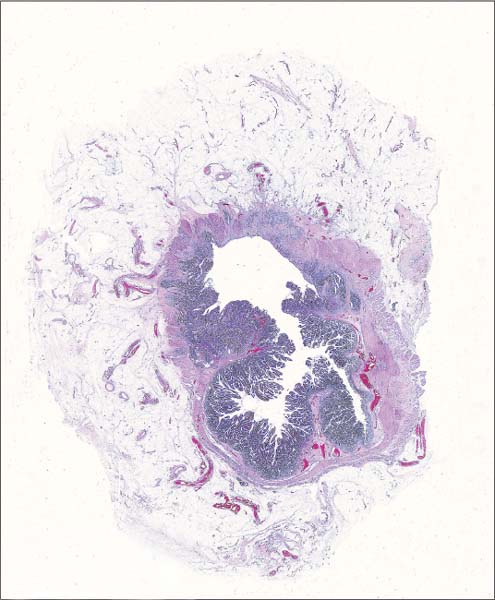
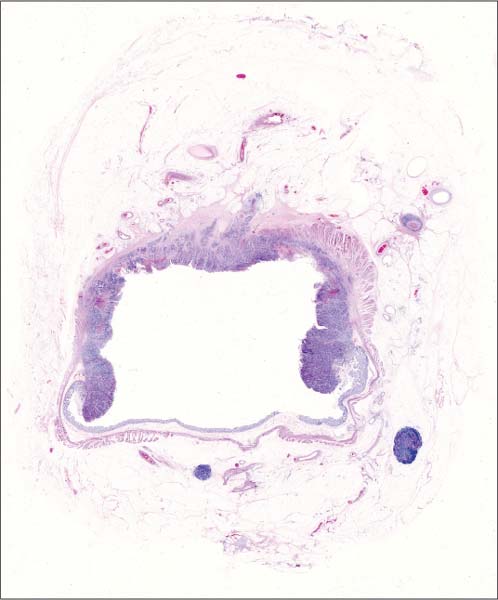
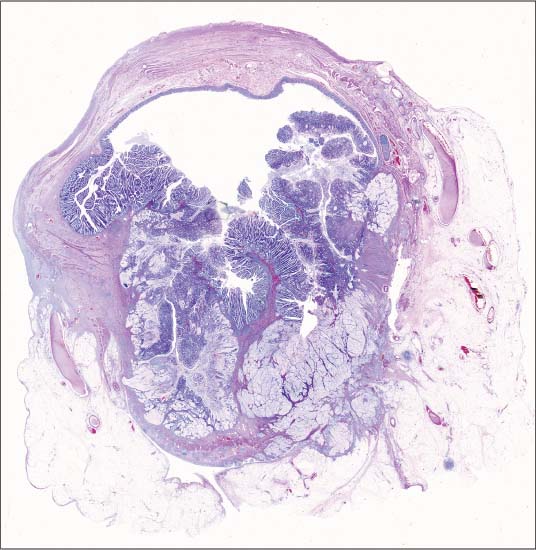
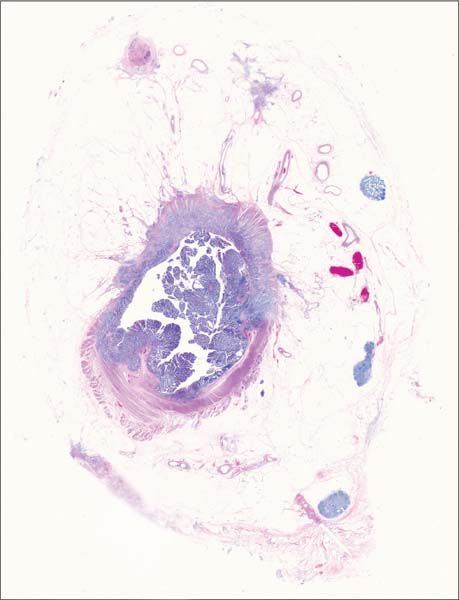
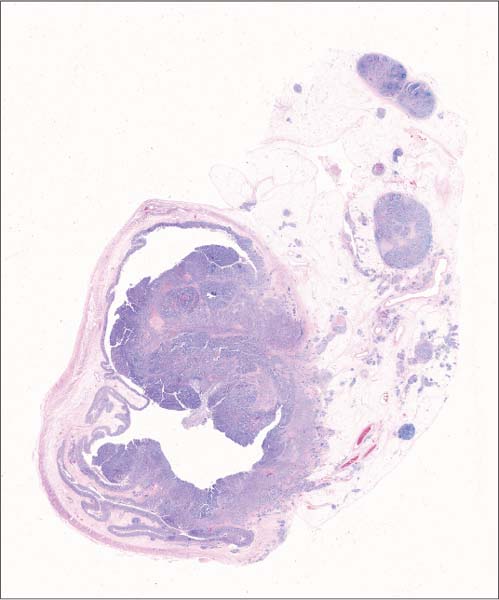
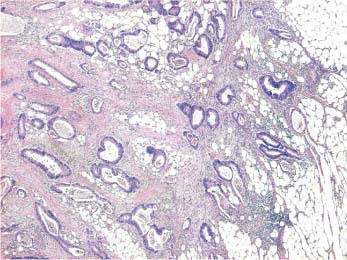
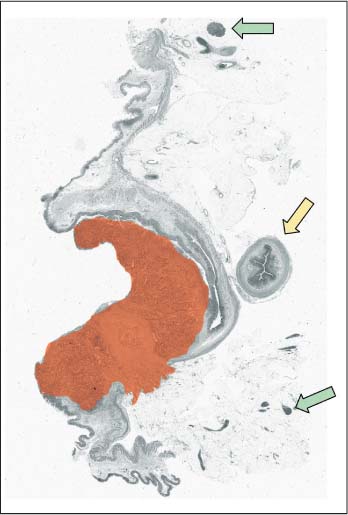
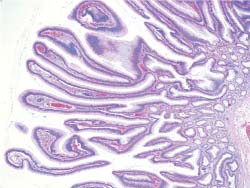
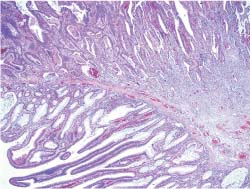
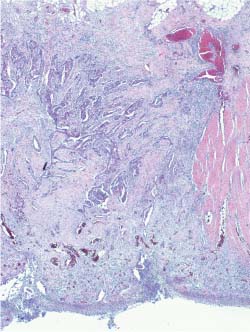
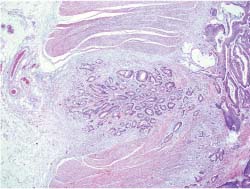
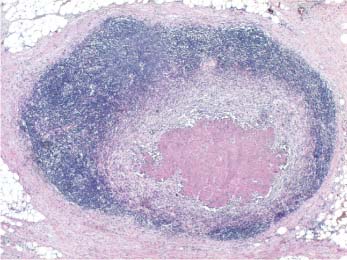
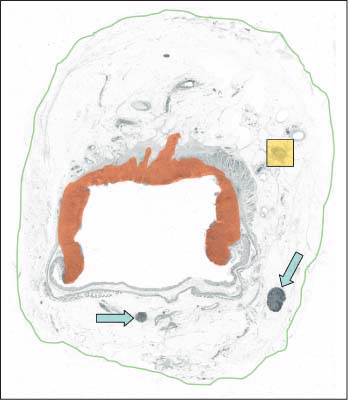
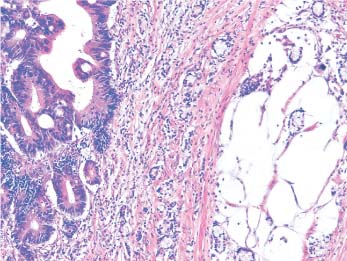
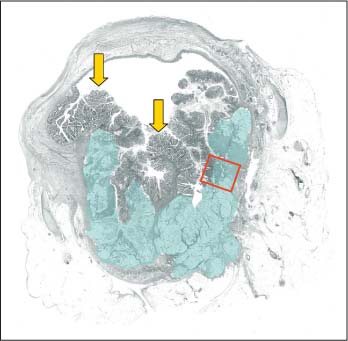
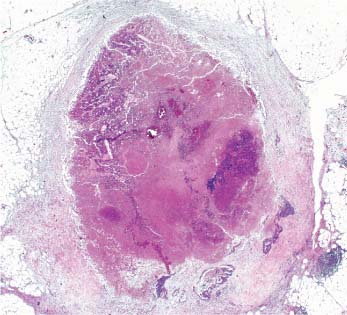
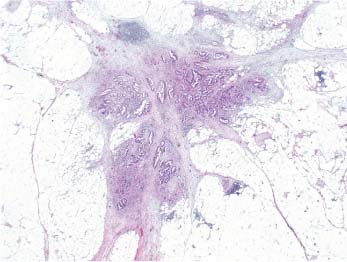
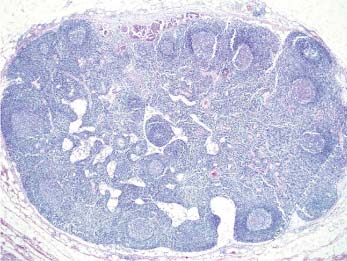
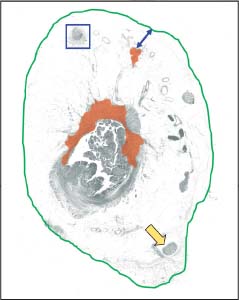
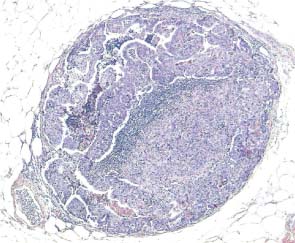
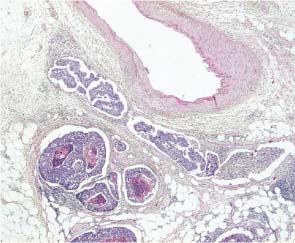
3 Advanced Colorectal Cancer Patient data: 77-year-old male patient presenting with sideropenic anemia. An ulcerated tumor was found endoscopically in the cecum, diagnosed as invasive carcinoma on preoperative biopsy. Surgical treatment: Right hemicolectomy, no preoperative irradiation. Specimen: 36-cm-long colon segment with a 5-cm part of the terminal ileum containing an exophytic tumor in the cecum 4cm in diameter. Histopathologic diagnosis: Moderately differentiated adenocarcinoma infiltrating through the lamina muscularis propria into the pericolic tissue, 13 lymph nodes without signs of metastasis, radical excision. TNM stage: IIA (T3N0M0), Dukes B. Follow-up: 49 months, no signs of disease recurrence. Infiltration of the tumor structures beyond the level of the muscularis propria into the subserosa or into the pericolic/ perirectal tissue (as illustrated in Fig. 3.1a) indicates B stage in Dukes’ classification. Many other classification systems, including the TNM classification, recognize this level of infiltration as a crucial unfavorable prognostic factor. As was already demonstrated, a large histologic section, taken in the plane of the deepest infiltration of the tumor, shows the level of infiltration without the aid of a microscope. The large section shown in Figure 3.1 demonstrates an infiltrating carcinoma of the cecum, corresponding to the red-colored area in the schematic image (Fig. 3.1b). The deepest tumor structures infiltrating into the fatty tissue are microscopically magnified in Figure 3.1a. Note the reactive lymph nodes (indicated with green arrows in Fig. 3.1b). Since the tumor developed in the cecum, a transection of the terminal part of the ileum (indicated with the yellow arrow in Fig. 3.1b) was also included in the large section. Fig. 3.1a Fig. 3.1b Schematic guide to the morphologic details in the large section in Fig. 3.1. Fig. 3.1 Large-section histology image of a colon carcinoma infiltrating beyond the level of the lamina muscularis propria. Patient data: 72-year-old female patient presenting with rectal bleeding. An ulcerated tumor was found endoscopically in her rectum 7 cm from the anus, diagnosed as invasive carcinoma on endoscopic biopsy. Surgical treatment: Mesorectal resection, no preoperative irradiation. Specimen: 18-cm-long rectum with a 6 × 5-cm partly exophytic, partly ulcerated tumor, 2 cm from the distal margin. Histopathologic diagnosis: Moderately differentiated adenocarcinoma infiltrating through the lamina muscularis propria into the pericolic tissue. Ten lymph nodes without signs of metastasis. Radical excision. TNM stage: IIA (T3N0M0), Dukes B. Follow-up: 17 months, no signs of disease recurrence. In this particular case, the large histologic section (Fig. 3.2) demonstrates a villous adenoma covering the anterior part of the rectal circumference and an invasive carcinoma that developed in the adenoma covering the posterior half. The villous structures of the adenoma (corresponding to the area of the blue circle in Fig. 3.2e) are also seen magnified in Figure 3.2a. The interface of the structures of the adenoma and the carcinoma is microscopically magnified in Figure 3.2b, corresponding to the area of the red rectangle in the schematic image (Fig. 3.2e). The cancer infiltrated beyond the level of the lamina muscularis propria, interrupting the muscle layer at several points, two of which are magnified in Figure 3.2c, d (corresponding to the green and yellow rectangles in the schematic image, Fig. 3.2e, respectively). The blue arrow indicates the free mesorectal resection margin. A narrow white line in Figure 3.2e marks the border between the adenoma (under the line) and the carcinoma (above the line). Fig. 3.2a Fig. 3.2b Fig. 3.2c Fig. 3.2d Fig. 3.2 Large-section histology image of a rectal carcinoma developed in a villous adenoma. Fig. 3.2e Schematic guide to the morphologic details in the large section in Fig. 3.2. Patient data: 77-year-old male presenting with watery diarrhea. A large tumor was found endoscopically in his rectum, 10 cm from the anus, diagnosed as invasive carcinoma on endoscopic biopsy. Surgical treatment: Preoperative irradiation and mesorectal resection. Specimen: 25-cm-long rectum with an 8×7-cm ulcerated tumor, 5 cm from the distal margin. Histopathologic diagnosis: Moderately differentiated adenocarcinoma infiltrating through the lamina muscularis propria into the pericolic tissue. Three of the 14 examined lymph nodes contained metastasis. Radical excision. TNM stage: IIIB (T3N1M0), Dukes C. Follow-up: 46 months, no signs of disease recurrence. The large histologic section in Figure 3.3 demonstrates an advanced rectal carcinoma (corresponding to the red-colored area in the schematic image, Fig. 3.3b), which had developed in a tubulovillous adenoma. The rests of the adenoma are well seen on the periphery of the tumor. The cancer infiltrated through the muscular wall following the perivascular spaces. Examination of the tumor after preoperative irradiation showed some regression of the cancer as well as peritumoral fibrosis. The two lymph nodes in the specimen (marked with the blue arrows in Fig. 3.3b) were free of metastases. However, the third lymph node (marked with the yellow rectangle) contained a necrotic mass corresponding to a necrotic metastasis after irradiation. This node is histologically magnified in Figure 3.3a. Fig. 3.3a Fig. 3.3b Schematic guide to the morphologic details in the large section in Fig. 3.3. Fig. 3.3 Large-section histology image of a rectal carcinoma with lymph node metastasis. Patient data: 66-year-old man with sideropenic anemia and celiac disease. A large tumor was found endoscopically in the area of the ileocecal valve. The endoscopic biopsy contained only adenoma structures. Surgical treatment: Ileocecal resection, no preoperative irradiation. Liver metastases were seen on laparotomy. Specimen: 12-cm-long ileocecal specimen with a 6-cm-long appendix. The cecum contained an exophytic 7 ×5-cm tumor, 6 cm from the distal margin. Histopathologic diagnosis: Well-differentiated mucinous adenocarcinoma infiltrating through the lamina muscularis propria into the pericolic tissue. Four of 10 lymph nodes with metastases. Radical excision. TNM stage: IV (T3N2M1), Dukes C. Follow-up: Died of the disease 9 months after the operation. The mucinous carcinoma demonstrated in Figure 3.4 had also developed in a villous adenoma. Both the structures of the adenoma (some of them marked with yellow arrows in the schematic image, Fig. 3.4b) and the areas of the mucinous cancer (corresponding to the blue-colored area in the schematic image) are well seen in the large histologic section. The tumor infiltrated the pericolic fatty tissue. The cancer exhibited obvious intratumoral heterogeneity, as demonstrated in Figure 3.4a, which shows a microscopic detail from the area marked with the red rectangle in Figure 3.4b. Mucinous carcinoma in the colorectum is defined as a cancer with dominating mucinous structures (more than 50% of the tumor). The large histologic section allows proper assessment of the proportions of different tumor types in cases of heterogeneous tumors, and assists in proper tumor typing. It also helps in appreciating the difficulties in obtaining biopsies representative of the invasive part of the tumor, as in the present case. Fig. 3.4a Fig. 3.4b Schematic guide to the morphologic details in the large section in Fig. 3.4. Fig. 3.4 Large-section histology image of a mucinous colon carcinoma that developed in a villous adenoma. Patient data: 72-year-old woman with anemia. A large malignant lesion was found endoscopically 7 cm from the anus in her rectum. The diagnosis of invasive carcinoma was made on endoscopic biopsy. Surgical treatment: Mesorectal resection, no preoperative irradiation. Specimen: 18-cm-long rectum with a tumor 6cm in diameter and 2 cm from the distal margin. Histopathologic diagnosis: Moderately differentiated rectal adenocarcinoma infiltrating through the lamina muscularis propria into the pericolic tissue. Four of the 15 examined lymph nodes contained metastases. In addition, isolated tumor foci were found in the perirectal tissue. Radical excision, mesorectal margin 4 mm. TNM stage: IIIC (T3N2M0V2), Dukes C. Follow-up: 14 months, no signs of disease recurrence. The large histologic section in Figure 3.5 demonstrates an invasive carcinoma (corresponding to the red-colored area in the schematic image, Fig. 3.5d), the rest of the tumor being tubulovillous adenoma filling the lumen of the large intestine. An enlarged, tumor-containing, necrotic lymph node is seen on the left upper edge of the image marked with the blue rectangle in Figure 3.5d and is histologically magnified in Figure 3.5a. Isolated foci of infiltrating tumor tissue without histologic evidence of residual lymph node structures in their surroundings are also seen in the mesorectum (partly marked in red and indicated with a blue double arrow in Fig. 3.5d; magnified microscopically in Fig. 3.5b). According to the TNM classification, if the foci have the round form and smooth contour of a lymph node, they should be classified as lymph node metastases. If they are irregular, as in this case, they should be classified as vascular invasion (V1 if seen only microscopically, V2 if seen upon examination with the naked eye). The isolated tumor foci should also influence the measurement of the surgical margin, as indicated with the blue double arrow in Figure 3.5d. In this case, additional lymph nodes are seen in the large section, one of them, marked with the yellow arrow, containing metastasis in the subcapsular sinus (Fig. 3.5c, upper edge of the image). Fig. 3.5a Fig. 3.5b Fig. 3.5c Fig. 3.5 Large-section histology image of a rectal carcinoma with lymph node metastases and isolated tumor foci in the perirectal fatty tissue. Fig. 3.5d Schematic guide to the morphologic details in the large section in Fig. 3.5. Patient data: 68-year-old woman with subileus and a large palpable tumor in the cecal region. Surgical treatment: Right hemicolectomy, no preoperative irradiation. Specimen: 24-cm-long segment of the colon and an 11-cm part of the terminal ileum with a 5 cm in diameter exophytic tumor in the vicinity of the ileocecal valve; free margins, large palpable nodes in the mesenterium. Histopathologic diagnosis: Moderately differentiated adenocarcinoma infiltrating through the lamina muscularis propria into the pericolic tissue; 26 of the 31 examined lymph nodes contained metastases. In addition, isolated tumor foci were found in the pericolic tissue. Vascular invasion and infiltration of the serosal surface were also evidenced. TNM stage: IIIC (T3N2M0V1), Dukes C. Follow-up: The patient died of the disease 17 months after the operation. The large histologic section in Figure 3.6 is very informative as it demonstrates the large exophytic and infiltrating carcinoma in the posterior parts of the cecum (corresponding to the red-colored area in the schematic image, Fig. 3.6c) together with a large area of the mesocolon. The tumor infiltrated the intestinal wall and the pericolic fatty tissue, partly forming continuous extensions, partly forming isolated tumor foci (also red-colored in Fig. 3.6c) lacking any connection with the main tumor mass. Some of the isolated tumor foci (marked with arrows in Fig. 3.6c) are round or oval shaped and have smooth contours. One of them (marked with the yellow arrow) is magnified in Figure 3.6a. This lesion represents a borderline structure between a metastatic lymph node and an isolated round tumor focus, as only a minimal rest of the lymphoid tissue is present in the central part of the lesion. However, this borderline image justifies classification of the smooth-contoured isolated tumor foci as lymph node metastases. Figure 3.6b is a microscopic magnification of the area of the blue rectangle in Figure 3.6c and demonstrates an irregular, isolated tumor focus partially with vascular invasion. Several enlarged lymph nodes containing metastatic tumor structures are also seen (green-colored in Fig. 3.6c). Fig. 3.6a Fig. 3.6b Fig. 3.6c Schematic guide to the morphologic details in the large section in Fig. 3.6.
Case 3.1 Infiltrating Colon Carcinoma, Dukes B
Practical points
Case 3.2 Rectal Carcinoma That Developed in a Villous Adenoma
Practical points

Case 3.3 Rectal Carcinoma, Dukes C
Practical points
Case 3.4 Mucinous Carcinoma of the Colon
Practical points
Case 3.5 Invasive Rectal Carcinoma, Dukes C
Practical points
Case 3.6 Advanced Colon Carcinoma

Practical points
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree