Adult T-cell Leukemia/Lymphoma
Aaron Auerbach, MD, PhD
Key Facts
Etiology/Pathogenesis
Long latency period between HTLV-1 infection and tumor development
Small risk of ATLL in HTLV-1 infected people
Tax viral oncoprotein linked to tumorigenesis
Clinical Issues
4 clinical presentations: Acute, chronic, lymphoma, and smoldering
Microscopic Pathology
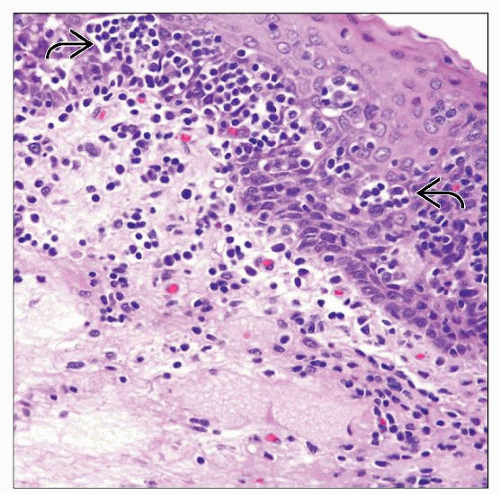
Skin with T-cell infiltrate in epidermis, dermis, &/or subcutis
Epidermotropism &/or Pautrier microabscesses
Peripheral blood with multilobated “flower” cells
Lymph nodes with effaced architecture and diffuse infiltrate
Ancillary Tests
Confirmation of HTLV-1 infection by serology
Immunophenotype: Regulatory T cells CD3(+), CD4(+), CD25(+), FOXP3(+), CCR4(+); often loses CD7; cytotoxic markers negative
Clonal T-cell receptor gene rearrangement
Complex chromosomal abnormalities; no one abnormality is characteristic of ATLL
Top Differential Diagnoses
Mycosis fungoides
Similar clinical picture with epidermotropism and peripheral blood lymphocytosis
Also CD4(+), CD8(−) T cells, but CD25(−), FOXP3(−), and CD30(−)
Anaplastic large cell lymphoma
TERMINOLOGY
Abbreviations
Adult T-cell leukemia/lymphoma (ATLL)
Synonyms
Adult T-cell leukemia
Definitions
T-cell lymphoma/leukemia of regulatory T cells (CD4[+], CD25[+], FOXP3[+]) caused by human T-cell leukemia virus type 1 (HTLV-1)
ETIOLOGY/PATHOGENESIS
Infectious Agents
Human T-cell leukemia virus type 1
Progresses to leukemia/lymphoma in < 5% of infected individuals
Long latency period
Most exposed as infants/children
Tumor often after 20 years of viral exposure
Transmitted through blood or breast milk
Also causes tropical spastic paraparesis
Encodes Tax (a viral oncoprotein)
Plays a role in development of ATLL
Activates transcription factors for T-cell proliferation genes
CLINICAL ISSUES
Epidemiology
Age
Adults, most commonly in 50s or 60s
Gender
Male:female = 1.5:1.0
Ethnicity
Endemic to southwest Japan, Caribbean islands, South America, and central Africa
Presentation
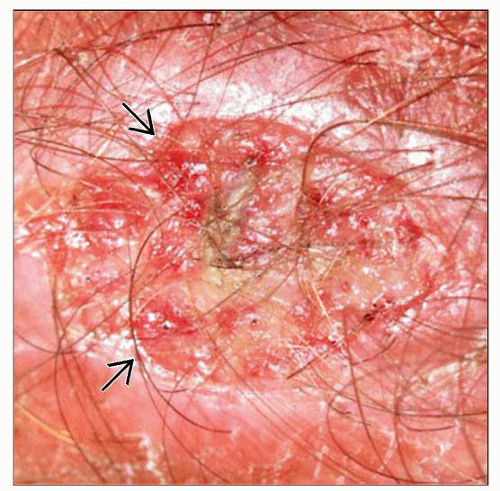
Skin lesions
Develop in 50% of ATLL patients
Usually multiple nodules/tumors, papules, plaques, or macules
Papules may cover large segments of body
Rarely, erythroderma, purpura, prurigo, or erythema multiforme
Other sites of disease include lymph nodes, peripheral blood, bone, spleen and sometimes lung, liver, and CNS
Most patients have generalized lymphadenopathy
Hypercalcemia from increased osteoclast bone resorption
4 clinical presentations: Acute, chronic, lymphoma, and smoldering
Acute subtype
Most common subtype
Severe peripheral blood lymphocytosis, ↑ WBC, ↑ LDH, skin lesions, lymphadenopathy
Hypercalcemia and lytic bone lesions
Immunodeficiency leads to other opportunistic infections
Chronic subtype
Lymphocytosis, but ↓ WBC than acute subtype
No hypercalcemia, exfoliative skin rash
Lymphomatous subtype
↑ lymphadenopathy; usually no peripheral blood involvement
Less hypercalcemia than acute subtype; skin often involved
Smoldering subtype
> 5% tumor cells in peripheral blood, even though normal WBC count
Tumor cells small with less pleomorphism and lobation
No hypercalcemia or lymphadenopathy
Treatment
Adjuvant therapy
Multiagent chemotherapy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree