Adenocarcinoma
Key Facts
Terminology
Malignant epithelial neoplasm with glandular differentiation
Etiology/Pathogenesis
Close association with tobacco smoking
Clinical Issues
Cough
Weight loss
Chest pain
Difficulty breathing
Macroscopic Features
Peripheral or central tumors
Varying size from 0.6 cm to > 10 cm
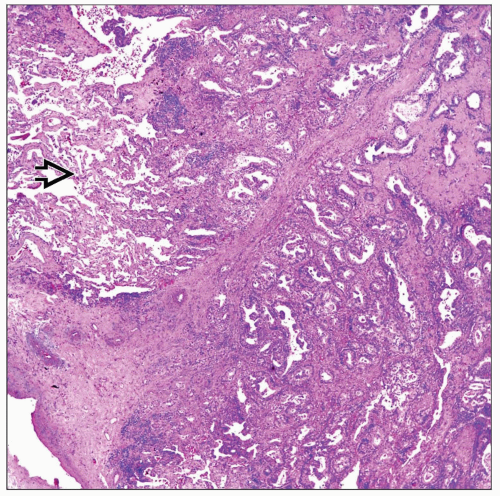
Microscopic Pathology
Acinar
Solid
Papillary
Ancillary Tests
EGFR by FISH
Analysis of exons 18, 19, 20, and 21
Top Differential Diagnoses
Adenocarcinoma from extrathoracic origin
Atypical adenomatous hyperplasia (AAH)
Adenoid cystic carcinoma (ACC)
Fetal adenocarcinoma (monophasic pulmonary blastoma)
Papillary carcinoma of thyroid origin
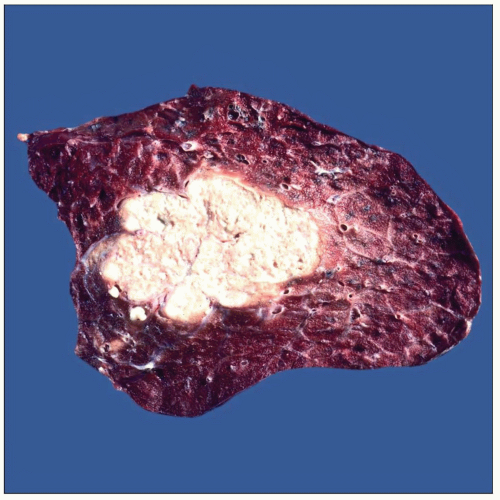 Gross photograph shows a peripherally located lung adenocarcinoma. The mass is relatively well demarcated but not encapsulated. It is tan and nodular. |
TERMINOLOGY
Abbreviations
Adenocarcinoma (AdenoCa)
Definitions
Malignant epithelial neoplasm with glandular differentiation
ETIOLOGY/PATHOGENESIS
Environmental Exposure
Close association with tobacco use
Etiology
Tumor probably originates from endobronchial glands
CLINICAL ISSUES
Epidemiology
Incidence
In last decade, adenocarcinomas have become more prevalent than any other non-small cell carcinoma
Currently is most common non-small cell carcinoma
Age
Although more common in adults, adenocarcinomas also occur in younger individuals
Adenocarcinomas are more common in 6th and 7th decades of life
Presentation
Cough
Weight loss
Difficulty breathing
Chest pain
Cushing syndrome
Superior vena cava syndrome
Pancoast syndrome
Hemoptysis
Treatment
Surgical approaches
Segmentectomy, lobectomy, pneumonectomy
Adjuvant therapy
Chemotherapy, radiation therapy, or both
Cases positive for epidermal growth factor receptor (EGFR) mutation may receive different treatment
Prognosis
Depends on stage at time of diagnosis
Patients with carcinomas positive for EGFR mutation may have better prognosis
It is also possible that tumors with better differentiated histology have more favorable outcome
It may also be related to other pulmonary function factors as well as other medical conditions
MACROSCOPIC FEATURES
General Features
Peripheral or central tumors
Tumors may show necrosis &/or hemorrhage
Homogeneous tan surface
Well-circumscribed but not encapsulated
Sections to Be Submitted
Tumor in relation to pleural surface
Pleural involvement crucial for staging tumors < 3 cm in size
Size
Varying size from 0.6 cm to > 10 cm
MICROSCOPIC PATHOLOGY
Histologic Features
Malignant glandular component
Predominant Pattern/Injury Type
Acinar
Solid
Papillary
Mixed
Predominant Cell/Compartment Type
Epithelial
True Papillary Carcinoma
Should be composed of at least 75% true papillae with fibrovascular cores
This particular pattern is believed to be more aggressive
Lymph node metastases in this pattern are commonly seen
TTF-1(+) and thyroglobulin(-)
Papillary Carcinoma with Morular Component
Similar criteria to true papillary carcinoma
Presence of morular component in alveolar spaces
“Morules” are of different sizes and always in intraalveolar location
TTF-1(+) and thyroglobulin(-)
Micropapillary Carcinoma
Composed of small micropapillae without fibrovascular cords
This pattern is often seen in combination with true papillary carcinoma
TTF-1(+) and thyroglobulin(-)
Hepatoid Adenocarcinoma
Composed of cords of neoplastic cells resembling hepatic parenchyma
This pattern is commonly placed among large cell carcinomas of lung
TTF-1 may show focal positive staining
Warthin-like Adenocarcinoma
Prominent lymphoid component similar to tumors in salivary gland
Some cases of mucoepidermoid carcinoma may also display similar features
Glandular proliferation with cells producing mucin embedded in inflammatory background
TTF-1 may show positive staining
Adenomatoid Tumor-like Adenocarcinoma
Bland appearance similar to true adenomatoid tumor
In some cases, can be confused with so-called alveolar adenoma
TTF-1 and keratin 7 positive
ANCILLARY TESTS
Histochemistry
Mucicarmine
Reactivity: Positive
Staining pattern
Cytoplasmic
PAS-diastase
Reactivity: Positive
Staining pattern
Cytoplasmic
EGFR by Fluorescent In Situ Hybridization (FISH)
Analysis of exons 18, 19, 20, and 21
DIFFERENTIAL DIAGNOSIS
Adenocarcinoma from Extrathoracic Origin
Immunohistochemistry positive for TTF-1; keratin 7 would favor lung origin in vast majority of cases
Atypical Adenomatous Hyperplasia (AAH)
Lesion ≤ 0.5 cm in diameter
Shares similar histological features with BAC
Adenoid Cystic Carcinoma (ACC)
Fetal Adenocarcinoma (Monophasic Pulmonary Blastoma)
Presence of morules and embryonic-type glandular structures
Presence of cytoplasmic mucin content in favor of AdenoCa
Papillary Carcinoma of Thyroid Origin
Histologically tumors with papillary pattern may show similar histological features
Positive TTF-1 and negative staining for thyroglobulin favors primary lung cancer
DIAGNOSTIC CHECKLIST
Pathologic Interpretation Pearls
Size of lesion will separate carcinoma from AAH
Cases designated as AAH are under 5 mm in diameter
GRADING
Low Grade
Well-differentiated adenocarcinoma composed of easily identifiable glandular structures & arranged in back-to-back arrangement
Absence of necrosis, increased mitotic activity, and nuclear atypia
Glandular tumoral structures may be separated by extensive areas of collagenization
Intermediate Grade
Moderately differentiated adenocarcinoma composed of identifiable glands
Tumor may show more nuclear atypia and mitotic activity
Glandular structures may show more disarray
High Grade
Poorly differentiated adenocarcinoma may show solid areas with ↑ mitotic activity and nuclear atypia
Necrosis and hemorrhage may be present
SELECTED REFERENCES
1. Wahbah M et al: Changing trends in the distribution of the histologic types of lung cancer: a review of 4,439 cases. Ann Diagn Pathol. 11(2):89-96, 2007
2. Moran CA: Pulmonary adenocarcinoma: the expanding spectrum of histologic variants. Arch Pathol Lab Med. 130(7):958-62, 2006
3. Prudkin L et al: Epidermal growth factor receptor abnormalities in lung cancer. Pathogenetic and clinical implications. Ann Diagn Pathol. 10(5):306-15, 2006
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree