Chapter 8 Acute Upper Gastrointestinal Bleed
Definitions
The major causes of upper GI bleeding are gastric and duodenal ulcers, esophageal varices, and Mallory-Weiss tears. Other less common causes are Dieulafoy’s lesions (an arterial branch protruding through a mucosal defect, most commonly found in the gastric fundus), arteriovenous malformations, esophagitis, and neoplasms (Box 8-1).
Box 8-1 Causes of Acute Upper GI Bleeding
Rockey DC. Gastrointestinal Bleeding. In: Feldman M, Friedman LS, and Sleisenger MH, editors. Sleisenger and Fordtran’s Gastrointestinal and Liver Disease, 7th ed. Philadelphia. WB Saunders; 2002. p. 215. Reproduced with permission, 2005.
Initial Evaluation
History
The history should focus on determining risk factors and potential etiologies for gastrointestinal hemorrhage, and assessment of rebleeding risk. In addition, potential complications due to coexisting medical conditions (such as myocardial ischemia in patients with coronary artery disease) should also be evaluated.
Rebleeding risk is highest in elderly patients with many comorbidities, and those with persistent hypotension, hematemesis, or hematochezia (Box 8-2). There are many prognostic scoring systems, but their overall reliability remains low.
Initial Management
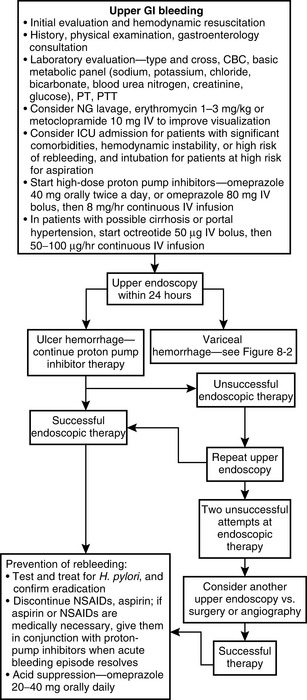
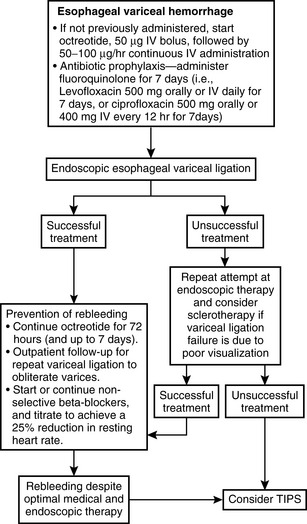
See Fig. 8-1 and Fig. 8-2 for an algorithmic approach to acute upper GI bleeding, with details for gastroduodenal ulcer and gastroesophageal variceal hemorrhage.
Hemodynamically stable patients with acute upper GI bleeding may be managed in a telemetry unit, whereas those with hemodynamic instability or persistent bleeding should be admitted to the intensive care unit.
Placement of two large-bore IV catheters, determination of hemodynamic status, and volume resuscitation (if necessary) should be performed, and patients should be kept NPO. Laboratory testing should include:
EKG and cardiac enzymes should be obtained in patients with risk factors for coronary artery disease.
Nasogastric lavage with tap water should be performed in patients with upper GI bleeding.
High-dose proton pump inhibitors, such as omeprazole 40 mg orally twice a day, should be initiated. Intravenous administration may also be used (i.e., omeprazole 80 mg bolus, then 8 mg/hr for 72 hr). A neutral pH enhances clot formation and decreases clot breakdown.
Radiologic Imaging
Plain films of the abdomen may be obtained to rule out complications, such as perforation, but have little role in the diagnosis and management of upper gastrointestinal bleeding.
Barium studies may obscure visualization of a bleeding source during upper endoscopy and should not be performed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree