Acute Antibody-Mediated Rejection, Kidney
Lynn D. Cornell, MD
Key Facts
Etiology/Pathogenesis
DSA usually directed against HLA class I or II on endothelium
May be against ABO blood group antigens in ABO-incompatible grafts
Clinical Issues
Acute renal failure
Oliguria
Serum donor-specific antibody (DSA)
Worse allograft survival in acute AMR compared to C4d negative ACR
Increased risk of developing transplant glomerulopathy (chronic AMR) after acute AMR
Microscopic Pathology
Glomerulitis, neutrophils, monocytes, fibrin
Glomerular thrombi or mesangiolysis
Peritubular capillary neutrophils
Dilated peritubular capillaries
Diffuse, bright positive staining of peritubular capillaries for C4d
Top Differential Diagnoses
Acute cellular rejection
Pyelonephritis
Acute tubular necrosis
Accommodation
C4d deposition without histologic injury or graft dysfunction
Most likely seen in stable ABO-incompatible grafts
TERMINOLOGY
Abbreviations
Antibody-mediated rejection (AMR)
Synonyms
Acute humoral rejection (AHR)
ETIOLOGY/PATHOGENESIS
Donor-Specific Antibody (DSA)
DSA usually directed against HLA class I or II on endothelium
Blood group antigen in ABO-incompatible grafts
Other, unknown, non-MHC antigens on endothelium
DSA activates complement via classical pathway
C4d is inactive fragment of C4b of classical complement pathway
C4d is covalently bound at site of complement activation on endothelium
Complement-fixing DSA associated with greater acute graft injury
Terminal complement blockade with C5 inhibitor reduces early acute AMR in recipients with preformed DSA
Results provide evidence that most acute AMR is not only antibody mediated but also complement mediated
CLINICAL ISSUES
Epidemiology
Incidence
˜ 25% of acute rejection episodes are due to antibody
Can occur any time post transplant
Presensitized patients at highest risk for acute AMR in 1st month post transplant
Some late acute AMR cases associated with immunosuppressive medication nonadherence (combined with acute cellular rejection)
Presentation
Acute renal failure
Oliguria
Laboratory Tests
Circulating donor-specific anti-HLA class I or II antibody in 88-95% of acute AMR with C4d deposition
Minority (5-10%) have undetectable DSA
May be due to non-HLA antibody
Possible antibody absorption by graft
High serum DSA levels in acute AMR
Can be measured by B- or T-cell flow crossmatch or by single-antigen bead tests
Serum DSA levels correlate with C4d immunofluorescence and severity of changes seen by light microscopy
Treatment
Plasmapheresis
Removes serum DSA from circulation
Increased immunosuppression
Anti-lymphocyte therapies
Intravenous immunoglobulin (IVIG)
Rituximab (anti-CD20)
Monoclonal antibody directed against B cells
Prevents B cell differentiation to plasma cells
Does not affect existing antibody-secreting plasma cells
Anti-plasma cell therapy (experimental)
Bortezomib
Complement inhibition (experimental)
Eculizumab (anti-C5)
Inhibits terminal complement pathway and prevents formation of membrane attack complex
Does not affect serum DSA level
Kidney biopsies show C4d(+) PTCs, as C4 is upstream of C5 in complement cascade
Prognosis
Worse allograft survival in acute AMR compared to C4d(-) acute cellular rejection (ACR)
˜ 30% graft loss within 1 year vs. 4% graft loss for ACR
Increased risk of developing transplant glomerulopathy (chronic AMR)
Plasma cell-rich variant resistant to treatment; poor clinical outcome
MICROSCOPIC PATHOLOGY
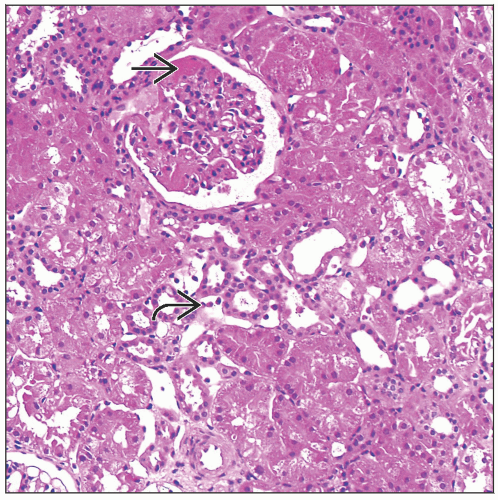
Histologic Features
Glomeruli
Glomerulitis
Neutrophils
Monocytes
Enlarged/swollen endothelial cells
Mitotic figures sometimes seen
Fibrin or thrombi in capillary loops
Glomerular thrombi or mesangiolysis, particularly in ABO blood group-incompatible grafts
Peritubular capillaries (PTCs)
Dilated
Neutrophils and mononuclear cells, termed peritubular capillaritis
Peritubular capillaritis usually mild in early acute AHR
Arteries
Fibrinoid necrosis in minority of cases
Possible endothelialitis (typically an acute cellular rejection lesion)
Interstitium
Edema, sparse infiltrate
Hemorrhage occasionally
Plasma cell-rich variant of acute humoral rejection
Associated with edema, high interferon-γ, and increased plasma cells
Tubules
Acute tubular injury
Little or no tubulitis
Sometimes neutrophils in lumen
Banff Classification of AMR
Histologic patterns
Type I: Acute tubular injury, minimal inflammation
Type II: Peritubular capillary &/or glomerular capillary inflammation &/or thrombi
Type III: Arterial fibrinoid necrosis or transmural inflammation (v3 lesion)
In addition to these histologic patterns, biopsies should show diffuse peritubular capillary (PTC) C4d deposition and serologic evidence of DSA
C4d immunofluorescence intensity should be at least 1+
If only 1 of these 2 criteria (C4d, DSA) is present with histologic changes, then biopsy is “suspicious” for acute AMR
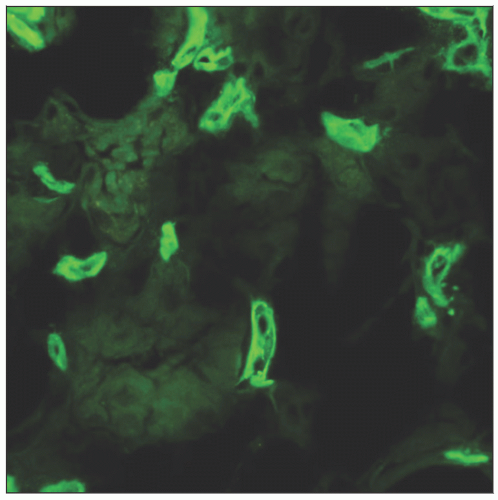
ANCILLARY TESTS
Immunohistochemistry
Diffuse PTC staining by immunohistochemistry (IHC)
IHC less sensitive than immunofluorescence (IF)
Circumferential peritubular capillary endothelial staining
Pitfall of IHC staining interpretation is serum staining for C4; may give false-positive result
Immunofluorescence
Electron Microscopy
Peritubular and glomerular capillary endothelial changes
Cell enlargement, loss of fenestrations, microvillous changes
Detachment from the basement membrane, lysis, apoptosis
DIFFERENTIAL DIAGNOSIS
Chronic AMR (CAMR)
CAMR biopsy features
Transplant glomerulopathy (TG)
Peritubular capillaropathy
PTC basement membrane multilamination
Best seen by electron microscopy
Transplant arteriopathy
Pattern may be due to chronic AMR or cellular rejection
“Accelerated arteriosclerosis” is another pattern of transplant arteriopathy due to CAMR and may be indistinguishable from arteriosclerosis due to hypertension
C4d may be negative or focally, multifocally, or diffusely positive
Mononuclear cells in capillaries; fewer neutrophils present
Peritubular capillaritis may be moderate to severe (Banff PTC score 2-3)
Usually a stable or slowly declining clinical course
Proteinuria often found in patients with TG
If acute renal insufficiency, acute AMR may occur together with features of CAMR
Diffuse C4d(+) PTCs
CAMR may be seen admixed with features of acute AMR and ACR, particularly later post transplant in patients with medication nonadherence
Acute Cellular Rejection
Tubulitis and interstitial inflammation
Endothelialitis
20-30% of ACR cases are C4d positive, indicative of concurrent antibody-mediated rejection
Accommodation
C4d deposition without histologic evidence of graft injury and without graft dysfunction
Commonly seen in ABO blood group-incompatible grafts
Subclinical AMR
Seen on surveillance biopsy or incidentally on biopsy for clinical indication
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree