Cytomegalovirus Nephritis
Anthony Chang, MD
Key Facts
Terminology
CMV infection in kidneys, usually associated with systemic CMV in immunocompromised patient
Etiology/Pathogenesis
Cytomegalovirus
Immunocompromised patients at risk
Clinical Issues
Presentation
Renal dysfunction
Flu-like symptoms
Antiviral agents
Ganciclovir or valganciclovir
CMV immune globulin
Reduce or alter immunosuppressive agents
Microscopic Pathology
Nuclear inclusions
Most prominent in tubular epithelium
Glomerular capillary &/or peritubular capillary endothelial cells
Interstitial inflammation, mononuclear
Acute glomerulonephritis (rare)
Top Differential Diagnoses
Polyomavirus nephropathy
Adenovirus tubulointerstitial nephritis
Acute cellular rejection
Acute allograft glomerulopathy (form of rejection)
Diagnostic Checklist
Coinfection with other fungal or viral organisms may occur
TERMINOLOGY
Abbreviations
Cytomegalovirus (CMV) nephritis
Synonyms
CMV tubulointerstitial nephritis (TIN)
CMV nephropathy
CMV glomerulonephritis
Definitions
Direct CMV infection of kidneys, usually associated with systemic CMV involvement and immunocompromise
CMV may promote indirect effects on kidney, particularly in renal transplants, including acute allograft glomerulopathy
ETIOLOGY/PATHOGENESIS
Infectious Agents
Cytomegalovirus (human herpesvirus-5 [HHV-5])
Family Herpesviridae
β-subfamily
Double-stranded DNA virus
Risk Factors
Immunocompromised patients at risk for systemic CMV
Transplant recipients on immunosuppression
Transplant CMV from donor organ or reactivation in recipient
Matching CMV serologic status in renal transplant patients has minimized incidence of CMV TIN
Infants
Neonatal CMV infection from maternal transmission
HIV-infected patients
Causes benign, self-limited mononucleosis syndrome in normal individuals
Site of Infection
Epithelium, endothelium, monocytes
Renal involvement almost always associated with systemic infection
Lungs, liver, adrenals, retina, GI tract, epididymis, pancreas, bone marrow
Latent Virus
Most individuals infected before adulthood
Benign self-limited disease in normal individuals
Seroprevalence (90%)
Virus remains present in latent state for life
Effects on Immune System
Increased IL-6 and IL-10, decreased Th1 cytokines (interferon-γ)
Decreased expression of HLA antigens
CLINICAL ISSUES
Epidemiology
Incidence
Neonatal CMV
Most common neonatal infection
0.2-2% of live births in USA
9.4 per 100,000 infants ages 1-4 years in Australia
Transplant CMV
˜ 20% incidence of CMV disease with ganciclovir prophylaxis
˜ 45% incidence without prophylaxis
Frequency of CMV infection in renal transplant biopsies < 1%
Age
Neonatal, intrauterine
Immunocompromised adults
Gender
Male predilection
Ethnicity
No ethnic predilection
Presentation
Fever
Malaise
Leukopenia
Renal dysfunction
Acute renal failure
Proteinuria
Laboratory Tests
CMV IgM antibodies
Suggest recent or active infection
False positives due to rheumatoid factor
CMV IgG antibodies
Suggests chronic/latent infection
CMV antigen test
Indirect IF test to detect pp65 protein of CMV in peripheral blood leukocytes
CMV polymerase chain reaction (PCR)
Viral culture
Shell vial assay
Treatment
Drugs
Ganciclovir or valganciclovir
Prophylaxis
Intravenous therapy
Foscarnet
Side effects include crystal formation leading to glomerulopathy
Multinucleation of tubular epithelial cell nuclei may persist after foscarnet therapy
Cidofovir
CMV intravenous immune globulin (IVIG)
Reduce or alter immunosuppressive agents
Vaccination to prevent maternal transmission
Prognosis
Neonatal CMV
30% mortality among symptomatic infants
Survivors commonly have neurologic deficits
CMV disease in transplant recipient
Increased graft loss in past (10-20%)
Less adverse effect of CMV in patients on current immunosuppressive protocols
MICROSCOPIC PATHOLOGY
Histologic Features
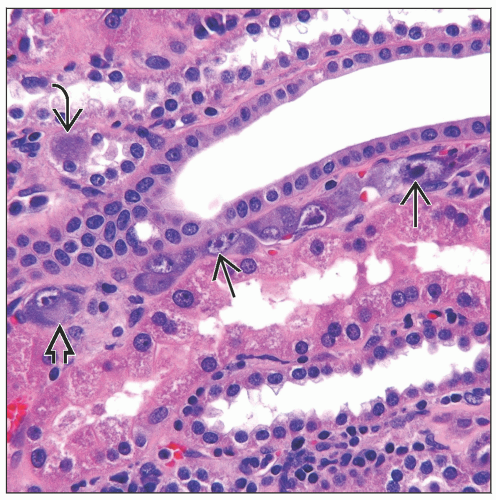
Pattern 1: Large intranuclear inclusions in tubular epithelial cells with interstitial nephritis
Variable interstitial inflammation
Occasional granulomatous inflammation
Rare or no intranuclear inclusions in endothelial cells
Monocyte inclusions in interstitial infiltrate
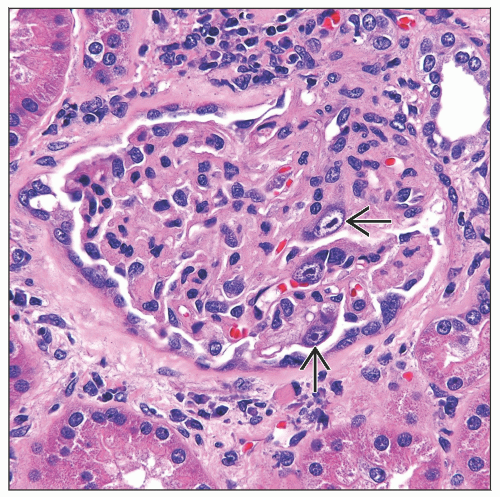
Pattern 2: Large eosinophilic intranuclear inclusions in endothelial cells
Glomerular and peritubular capillary endothelial cells may be infected
When endothelial cells are predominant cell infected by CMV, epithelial cells tend to be spared
Thrombotic microangiopathy may be present
Interstitial inflammation not prominent in cases with primarily endothelial cell infection
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree