Acquired Multilocular Thymic Cyst
Key Facts
Etiology/Pathogenesis
Acquired reactive process resulting from underlying infectious or inflammatory stimulus
Clinical Issues
Generally cured by complete surgical excision
Rare cases can recur when incompletely excised
Chest pain
Dyspnea
Often seen in children with AIDS
Macroscopic Features
Large, multilocular cystic structure
May show fibrous adhesions to pleura and pericardium
3-25 cm in diameter
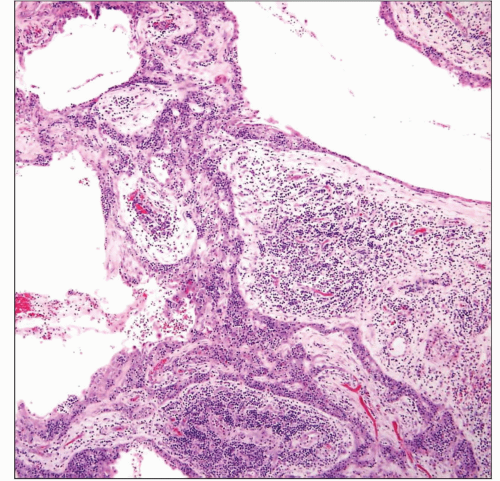
Microscopic Pathology
Cystic spaces lined by flat, cuboidal to squamous epithelium
Squamous epithelium may show pseudoepitheliomatous hyperplasia
Lining of cysts can be traced to dilated Hassall corpuscles
Prominent stromal hemorrhage, fibrosis, and chronic inflammation in wall of cysts
Prominent granulation tissue and cholesterol cleft granulomas in stroma
Prominent lymphoid follicular hyperplasia
Residual thymus showing branching, elongated strands of thymic epithelium
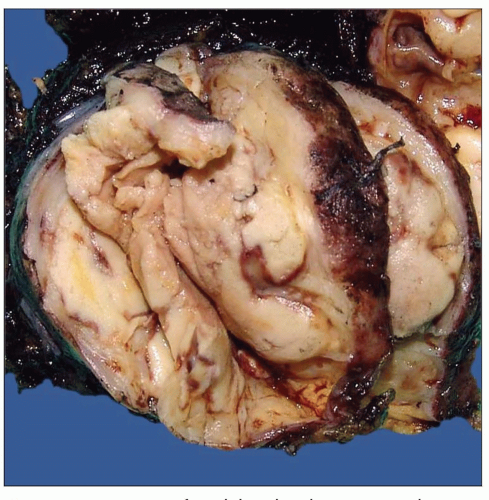 Gross appearance of multilocular thymic cyst shows a well-circumscribed cystic mass with hemorrhage in the walls of the cyst. |
TERMINOLOGY
Abbreviations
Acquired multilocular thymic cyst (AMTC)
Synonyms
Lymphoepithelial thymic cyst
Definitions
Acquired reactive process that results in cystic dilatation of thymic epithelium
ETIOLOGY/PATHOGENESIS
Pathogenesis
Acquired reactive process resulting from underlying infectious or inflammatory stimulus
CLINICAL ISSUES
Presentation
Chest pain
Dyspnea
Chest fullness
Associated with AIDS in children
Treatment
Surgical excision
Prognosis
Excellent prognosis
Generally cured by complete surgical excision
Rare cases can recur when incompletely excised
MACROSCOPIC FEATURES
General Features
Large, multilocular cystic structure
Cysts may contain clear or hemorrhagic fluid
May show fibrous adhesions to pleura and pericardium
Sections to Be Submitted
At least 1 section per centimeter of greatest diameter
Submit all solid areas in the walls of cysts
Size
3-25 cm in diameter
MICROSCOPIC PATHOLOGY
Histologic Features
Cystic spaces lined by flat, cuboidal to squamous epithelium
Squamous epithelium may show pseudoepitheliomatous hyperplasia
Lining of cysts can be traced to dilated Hassall corpuscles
Prominent stromal hemorrhage, fibrosis, and chronic inflammation in wall of cysts
Prominent granulation tissue and cholesterol-cleft granulomas in stroma
Prominent lymphoid follicular hyperplasia
Residual thymus showing branching, elongated strands of thymic epithelium
DIFFERENTIAL DIAGNOSIS
Cystic Hodgkin Lymphoma
Microscopic islands containing Reed-Sternberg cells should be present
Positive identification of Reed-Sternberg cells with antibodies to CD30/CD15 required for diagnosis of Hodgkin disease
Cystic Seminoma
Cystic Thymoma
Solid, confluent areas showing features of thymoma should be present in walls of cyst
Identification of keratin(+) cells amidst immature CD1a/CD3(+) thymocytes required for diagnosis of thymoma
Cysts may also result from massive dilatation and confluence of perivascular spaces
Cystic Teratoma
Heterologous elements should be identified in walls of cyst (i.e., cartilage, glial tissue, squamous or glandular epithelium, etc.)
May contain immature neural elements (immature teratoma)
MALT Lymphoma of Thymus
Cystic spaces in MALT lymphoma show infiltration of small lymphocytes into epithelial lining of cyst
Monotonous population of monocytoid B cells is present surrounding lymphoid follicles in MALT lymphoma
Infiltration of Hassall corpuscles by lymphocytes create lymphoepithelial lesions in MALT lymphoma
Thymic Carcinoma
Cystic mucoepidermoid carcinoma will show solid areas exhibiting epidermoid features and mucocytes in the walls of cysts
Basaloid carcinoma of thymus will show cystic dilatation of tumor cell islands that are lined by atypical, basaloid cells
Secondary MTC-like changes can be observed in surrounding, uninvolved thymic parenchyma in any type of thymic carcinoma
DIAGNOSTIC CHECKLIST
Clinically Relevant Pathologic Features
Multiple cysts lined by epithelium that is in continuity with cystically dilated Hassall corpuscles
Cyst walls show prominent fibrosis and chronic inflammation
Many cases also show prominent lymphoid follicular hyperplasia
Cases with pseudoepitheliomatous hyperplasia of lining epithelium may be confused for invasive squamous cell carcinoma arising in a cyst
Pathologic Interpretation Pearls
Most important feature is to make sure that malignant thymic neoplasm with secondary cystic changes (such as thymoma, lymphoma, or seminoma) has been ruled out by thorough sampling
SELECTED REFERENCES
1. Izumi H et al: Multilocular thymic cyst associated with follicular hyperplasia: clinicopathologic study of 4 resected cases. Hum Pathol. 36(7):841-4, 2005
2. Choi YW et al: Idiopathic multilocular thymic cyst: CT features with clinical and histopathologic correlation. AJR Am J Roentgenol. 177(4):881-5, 2001
3. Chhieng DC et al: Multilocular thymic cyst with follicular lymphoid hyperplasia in a male infected with HIV. A case report with fine needle aspiration cytology. Acta Cytol. 43(6):1119-23, 1999
4. Kontny HU et al: Multilocular thymic cysts in children with human immunodeficiency virus infection: clinical and pathologic aspects. J Pediatr. 131(2):264-70, 1997
5. Mishalani SH et al: Multilocular thymic cyst. A novel thymic lesion associated with human immunodeficiency virus infection. Arch Pathol Lab Med. 119(5):467-70, 1995
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree