FIGURE 23-1 Left anterior oblique (LAO 35°) image during transseptal VT ablation.
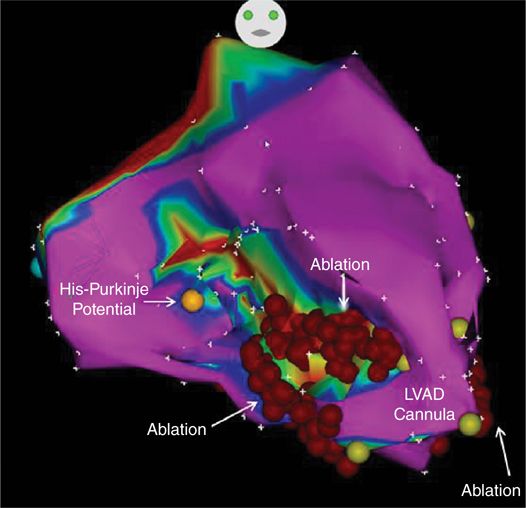
Electroanatomical mapping showed endocardial scar (<0.5 mV) involving the mid to apical anteroseptum and the posterolateral walls with border zone surrounding the LVAD cannula. The endocardial scar seen was out of proportion to his cardiomyopathy. Linear ablation lines were extended from the LVAD cannula through both scar zones; the posterolateral line was extended to the mitral valve annulus while the anteroseptal line was limited to sites below the His-Purkinje system (Figure 23-2).
FIGURE 23-2 Electroanatomical CARTO bipolar voltage map (<0.5 mV and 1.5 mV color range). Orange dot shows most inferior His-Purkinje potential. Yellow dots depict apical LVAD cannula. Linear ablation lines extending from anteroseptal LVAD cannula to mid septum. The apical aspect of the posterior lateral ablation line is also seen.
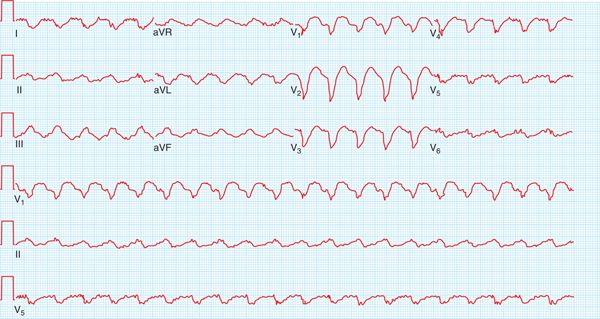
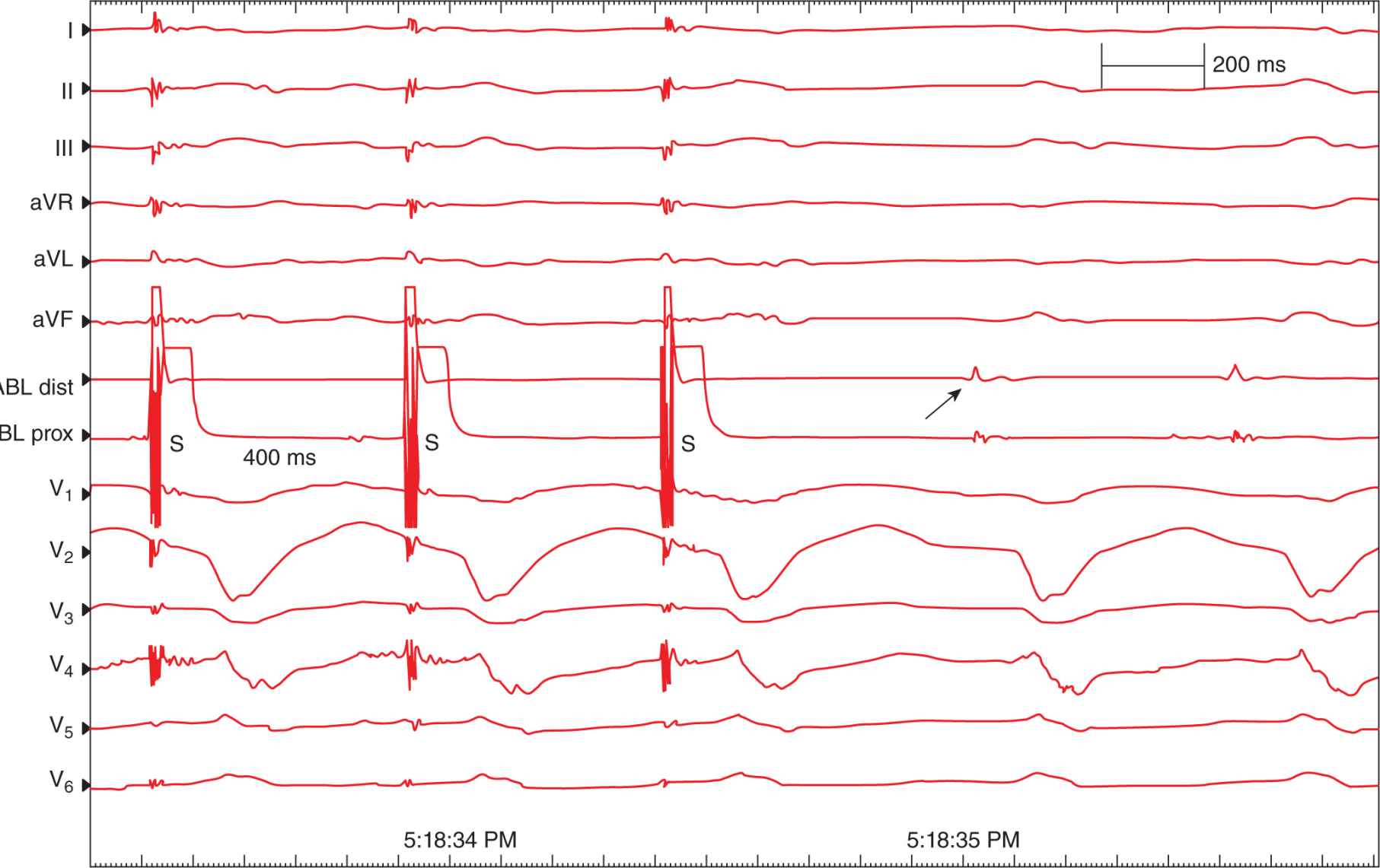
Postablation, he had recurrent VT, and mexiletin was added to amiodarone. He initially did well on this regimen, but several months later he had recurrent slow VT 120 bpm below his detection limit (Figure 23-3) and was referred to the EP lab for repeat VT ablation. With programmed ventricular stimulation, his clinical VT (left bundle inferior axis CL 520 ms) was induced and hemodynamically tolerated. Activation and entrainment mapping was performed throughout the LV via a transseptal approach without sites of early activation being detected. Mapping of the right ventricle showed earliest activation with concealed entrainment (Figure 23-4) at 12 o’clock on the tricuspid annulus. During ablation, there was prolongation of the CL with termination of VT. Postablation, VT was no longer inducible.
FIGURE 23-3 Surface ECG showing left bundle inferior axis morphology VT 122 bpm. The artifact seen throughout the ECG is noise from the LVAD.
FIGURE 23-4 Concealed fusion during ventricular pacing during VT. The 12-lead ECG and intracardiac recordings from the proximal and distal electrodes of the ablation catheter are shown. Ventricular pacing stimuli (S) are delivered from the distal electrode of the ablation catheter at a cycle length of 400 ms showing concealed fusion. Ablation at this site (arrow) leads to slowing and then termination of the VT.
VENTRICULAR TACHYCARDIA DURING VAD SUPPORT
As seen with this patient, over one-third of patients will have ventricular tachyarrhythmia events (VTEs) within 30 days following LVAD implantation.1,2 While concomitant ICD implantation has increased survival in VAD supported patients, there is a 25% incidence of appropriate ICD therapies.3 The highest rates of VTEs are seen within the first 2 weeks following VAD support,1,4–7 and recurrent VTEs are common with an average of 5 events per patient during VAD support.8 Unfortunately, a lack of VTEs early following VAD support does not preclude late VTEs. While VTEs may be hemodynamically tolerated in the setting of VAD support,9,10 they are associated with increased hospitalization rates, need for antiarrhythmic drug therapy, and increased mortality.1,9,11–13
Several factors predict the likelihood of VTEs during VAD support. The most consistent risk factor for VTEs is a history of VTEs prior to VAD support which doubles the risk of VTEs during VAD support.13 Early studies showed patients with ischemic heart disease had a greater risk for VTEs during VAD support,1,5 while a more recent study in patients with continuous support found that those with nonischemic heart disease had a 2.3-fold greater risk of VTEs.8
MECHANISMS OF VT
Inflow cannula effects, pathologic fibrosis of the failing heart, and electrical remodeling within the VAD-supported heart are mechanisms for ventricular arrhythmias in VAD patients. With continuous flow VADs, increased VAD speed, increased pulmonary venous return,14 and transient changes in venous return15
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree