Chapter 16 Abdominal Pain and Diarrhea in a 43-Year-Old Female (Case 6)
PATIENT CARE
Clinical Thinking
Though diarrhea is not usually associated with surgical conditions, I keep in mind the following:
• Diarrhea associated with appendicitis is usually related to direct irritation of the lower colon or rectum by the inflamed appendix.
• Diarrhea associated with ischemic colitis is bloody, but the dx is more likely in an older age group.
History
• Gastroenteritis usually presents with a hx of nausea/vomiting in addition to the diarrhea, often with recent onset and associated viral illness or sick contacts at home, and absence of peritoneal signs.
• Infectious colitis may have a hx of recent illness, bloody diarrhea, employment at a daycare center or as a food handler, recent antibiotic use, swimming in or drinking unsafe water, oral to anal sexual contact, or a visit to a foreign country or petting zoo. Antibiotic-associated diarrhea, including C. difficile colitis, has an identifiable antecedent hx of antibiotic use.
• With food poisoning, there is usually a hx of consuming unpasteurized dairy products, raw or undercooked meat or fish, or spoiled mayonnaise or other egg-related products.
Physical Examination
• VS: Fever suggests an inflammatory or invasive process. Tachycardia and hypotension can be associated with dehydration and/or sepsis.
• Peritoneal findings (tenderness, guarding, rebound) are more likely in appendicitis, infectious colitis or complicated C. difficile colitis. Not expected in gastroenteritis, uncomplicated IBD, or IBS.
Tests for Consideration
| $68 | |
| $53 | |
| $29 | |
| $63 | |
| $56 | |
| $125 | |
| $850 |
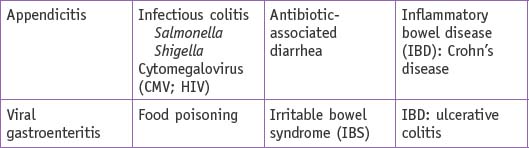
| Clinical Entities | Medical Knowledge |
|---|---|
| Appendicitis | |
| Appendicitis is covered in Chapter 11, Right Lower Quadrant Pain (Case 1). Associated diarrhea may relate to rectal or colonic irritation by the inflamed appendix or intra-abdominal fluid related to the inflammatory process. | |
| Tx of appendicitis is an urgent appendectomy (laparoscopic or open). | |
| Infectious Colitis | |
| PΦ | Infectious colitis is caused by infection with various pathogenic bacteria, viruses, or protozoa, including: Salmonella, Shigella, Campylobacter, enterohemorrhagic Escherichia coli, C. difficile, Rotavirus, Isospora, Cyclospora, adenovirus, Norwalk-agent, and Entamoeba histolytica. These pathogens either directly invade or adhere to colonocytes and interfere with normal absorption and secretion. |
| TP | Patients typically present with diarrhea of various durations and may have associated symptoms of dehydration, including postural light-headedness and low urine output. There may also be a hx of pathogen exposure. |
| Dx | Dx is based on hx, clinical examination, and presence of fecal leukocytes. Patients with a recent hx of antibiotic use should also have a stool test for C. difficile toxin. Fever, bloody diarrhea, or hypotension may warrant a more extensive workup including stool cultures and stool sent for ova and parasites. Specifically request tests for enterohemorrhagic E. coli when it is high on the list of differential dx. |
| Tx | Tx includes oral and/or IV hydration since dehydration is usually the most acute and life-threatening issue. Due to the development of antibiotic-resistant pathogens, empiric antibiotic tx should be limited to patients who have febrile illness or are definitively established to have shigellosis or Campylobacter infection. Tx of enterohemorrhagic E. coli with antibiotics is currently very controversial and most authorities would recommend supportive nonantibiotic tx only. |
| Antibiotic-Associated Diarrhea | |
| PΦ | Antibiotics can disrupt the normal GI tract flora and lead to a secretory diarrhea from incomplete absorption of simple starches. This diarrhea typically resolves on a low-starch diet. However, C. difficile, which is a pathogenic bacterium, can colonize the human GI tract after the normal gut flora have been altered by antibiotic therapy and release two toxins, Toxin A and Toxin B, that bind to intestinal cell receptors and lead to secretory diarrhea and inflammation. If a C. difficile infection remains undetected or the patient is immunocompromised, C. difficile can develop into pseudomembranous colitis with yellowish-white plaques approximately 1 cm in diameter scattered throughout the colon or rectum. A small minority of patients progress to fulminant colitis. |
| TP | The inflammation caused by C. difficile is typically associated with abdominal pain, fever, and an elevated white blood cell count. Any antibiotic can lead to C. difficile colonization, but the ones historically associated with C. difficile infection include ampicillin, amoxicillin, clindamycin, and cephalosporins. Fluoroquinolones are now a common cause of a new endemic strain of C. difficile. Fulminant colitis presents with abdominal pain, hypotension, fever, and a markedly elevated white blood cell count (>30,000) |
| Dx | Dx is based on hx, clinical examination, and the presence of C. difficile toxin on ELISA-based stool tests. If the dx is in doubt, flexible sigmoidoscopy or colonoscopy allows direct examination of the colorectal mucosa for signs of colitis and pseudomembranes. |
| Tx | The patient should discontinue the offending antibiotic if possible and then start 500 mg of metronidazole TID for 10 to 14 days. If the patient is pregnant or cannot take metronidazole, vancomycin 125 mg QID is an alternative therapy. Patients who have fulminant colitis with impending perforation may require subtotal colectomy. See Sabiston 14. |
| Food Poisoning | |
| PΦ | Patients ingest either massive amounts of pathogen or pathogen toxin. The resulting preformed or formed toxins prevent normal food absorption and increase stool water and mucous secretion. |
| TP | Patients will often present with a hx of pathogen consumption, usually at an event (picnic, baseball game, restaurant, etc.), and may recall other people at the same event experiencing identical GI symptoms. Symptoms within 6 hours suggest ingestion of a preformed toxin of Staphylococcus aureus or Bacillus cereus. Symptoms that begin at 8 to 14 hours suggest infection with Clostridium perfringens. |
| Dx | Dx is typically clinical, based on hx and lack of peritoneal signs. |
| Tx | This illness is typically self-limiting and patients should be instructed to avoid medications that may slow colonic transit of pathogens out of the body and should be advised to stay well hydrated. |
| Viral Gastroenteritis | |
| PΦ | Gastroenteritis is usually virally mediated (Norwalk or Norwalk-related) and causes small histopathological lesions in the jejunum that result in transient malabsorption syndromes. |
| TP | Usually associated with nausea/vomiting, but can present with diarrhea only. Malaise and low-grade fever may be present. Look for hx of a recent viral illness, sick contacts in the family (especially if there are children in daycare), and travel hx (especially cruise ships). |
| Dx | Dx is clinical only, and gastroenteritis is typically a dx of exclusion. |
| Tx | Symptomatic tx only, as this illness is self-limiting for most patients, with complete resolution of symptoms within 48 to 72 hours. |
| Infectious Colitis in the Immunocompromised Host | |
| PΦ | The pathogenesis is the same as for infectious colitis assuming adequate T-cell host defenses. If T-cell counts are low (CD4 <50) one must also consider AIDS-related CMV GI disease, and Mycobacterium avian complex (MAC). |
| TP | AIDS patients can present with acute or chronic diarrhea and mucosal hemorrhaging that may lead to intestinal perforation. |
| Dx | These diagnoses are usually discovered via hx/physical examination and a comprehensive diagnostic workup that includes stool studies for bacteria, C. difficile toxin, ova and parasites, and modified acid-fast smear for Cryptosporidium, Cyclospora or Isospora. If MAC is suspected, the workup should also include blood cultures for acid-fast bacteria. Sigmoidoscopy or colonoscopy may also be helpful to obtain biopsy samples for CMV. Imaging tests are generally not useful in these patients. |
| Tx | Tx may require empiric therapy with a quinolone and metronidazole until all diagnostic test results are back. For CMV, current tx includes induction therapy with ganciclovir or foscarnet for 3 to 6 weeks and consideration of maintenance therapy. See Sabiston 46, 48. |
| Irritable Bowel Syndrome | |
| PΦ | The pathogenesis of this syndrome is currently unknown, but is often associated with psychological stress. |
| TP | Patients typically present with altered bowel habits, often alternating between constipation and diarrhea. The diarrhea is often described as mucus-filled with feelings of incomplete evacuation. The diarrhea typically occurs only during the day and does not wake the patient at night. Associated symptoms may include dysmenorrhea, dyspareunia, reactive airway disease, and fibromyalgia. |
| Dx | By definition, results of all diagnostic tests, including CBC, thyroid function tests, and endoscopy, will be normal. |
| Tx | Tx for IBS includes dietary modification and patient education. Other therapeutic considerations include antispasmodic agents, antidepressants, and serotonin receptor antagonists. |
| Inflammatory Bowel Disease: Crohn’s Disease | |
| PΦ | Crohn’s disease is an IBD of uncertain etiology which is characterized by transmural inflammation. |
| TP | The typical patient usually presents with a chronic, episodic hx of abdominal pain and diarrhea, although it is possible that the patient will first present with abscess, frank perforation, or fistula. Patients may also present with extraintestinal manifestations, such as oral aphthous ulcers, perianal disease, arthritis, skin disease, or fat malabsorption. |
| Dx | Dx is typically via clinical hx and colonoscopy. Radiological studies (abdominal CT or barium small bowel follow-through) may help define Crohn’s strictures or lesions in the small bowel. |
| Tx | Initial therapy for Crohn’s disease usually begins with 5-aminosalicylic acid (5-ASA) drugs, but may progress to tx with antibiotics, corticosteroids, or immunosuppressive agents. Surgical tx in Crohn’s disease is for complications of the disease: obstruction, perforation, significant fistulae, or intractability despite medical tx. See Sabiston 48, 50; Becker 22. |
| Inflammatory Bowel Disease: Ulcerative Colitis | |
| PΦ | Ulcerative colitis is an IBD typically limited to the colonic and rectal mucosa. Pathogenesis is unknown, but may be part of a continuum of IBD along with Crohn’s disease. |
| TP | Patients usually present with a gradual onset of abdominal pain, and diarrhea is frequently bloody. |
| Dx | Dx is typically made through colonoscopy and pathologic findings on biopsy (crypt abscesses, chronic gland changes, etc.). |
| Tx | Tx of ulcerative colitis is initially medical. First-line agents include topical 5-ASA suppositories, enemas, or steroid foams. Oral steroids may be required. |
| The ileoanal reservoir procedure (J-pouch) is a surgical tx option for chronic ulcerative colitis that allows removal of the entire colon and all rectal mucosa and reconstruction without a permanent ostomy. See Sabiston 50, Becker 22. | |
a. Cholera: Vibrio cholerae, a gram-negative bacterium endemic in many developing countries in the world, secretes a toxin that causes persistent activation of adenylate cyclase and leads to increased chloride secretion and decreased sodium absorption, producing massive fluid and electrolyte loss. See Sabiston 26.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree