CHAPTER 60 Abdomen and pelvis: overview and surface anatomy
GENERAL STRUCTURE AND FUNCTION OF THE ABDOMINOPELVIC CAVITY
MUSCULOSKELETAL FRAMEWORK OF THE ABDOMEN AND PELVIS
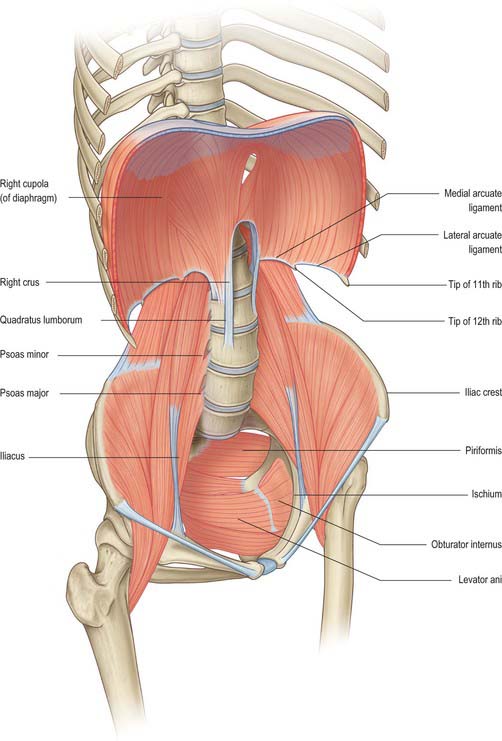
The walls of the abdominopelvic cavity consist of five lumbar vertebrae and their intervening intervertebral discs (lying in the posterior midline); three layers of skeletal muscles (transversus abdominis, internal oblique and external oblique) with associated fasciae and skin (lying lateral and anterolateral); a single muscular layer (rectus abdominis) with its associated fascial coverings (lying anterior); the bony ‘bowl’ formed by the walls of the true and false pelvis (ilium, ischium and pubis on each side); the muscles of the pelvic floor and perineum (lying inferiorly); the diaphragm (lying superiorly) (Fig. 60.1).
Thoracoabdominal interface
The thoracic and abdominal cavities interface with each other across the diaphragm. Six principle communications exist between the two cavities: the inferior vena cava, as it crosses between its short supra-hepatic portion and the intrathoracic portion below the right atrium, through the caval opening of the diaphragm (Ch. 62); the oesophagus passing inferiorly through the oesophageal opening of the diaphragm (Ch. 65); the aorta between the descending thoracic and abdominal portions, posterior to the median arcuate ligament of the diaphragm (Ch. 62); the lymphatics of the abdomen draining upwards to the thorax, mainly posterior to the median arcuate ligament via the thoracic duct lying posterolateral to the aorta, but also via peri-caval lymphatics and small vessels draining directly through and at the peripheral insertions of the diaphragm; the azygos and hemiazygos veins ascending behind the median arcuate ligament of the diaphragm into the thoracic azygos system (Ch. 62); the autonomic nervous system, both sympathetic and parasympathetic (see below) which cross between the two cavities behind the medial arcuate ligaments of the diaphragm, via the various diaphragmatic openings, and directly through the substance of the diaphragm itself (Ch. 54). Cutaneous neurovascular structures also cross between the thorax into the abdominal wall structures.
Pelvis–lower limb interface
The pelvis forms an integral part of the bony structure of both the abdominopelvic cavity and the lower limb. It transmits the weight of the upright body from the femoral heads to the lumbar spine as well as providing a stable platform about which movement of the hip joint can occur. Its bony surfaces give rise to extensive muscular attachments for the muscles of the buttock and thigh (Ch. 67) as well as for the muscles of the pelvic floor and perineal diaphragm (Ch. 63). The pelvis also transmits or gives origin to the neuro-lympho-vascular structures which supply the lower limb. The principle structures are as follows. The venous drainage includes the common femoral vein passing under the inguinal ligament to become the external iliac vein; the obturator veins passing through the obturator foramen; the superior and inferior gluteal veins draining from the buttock into the internal iliac vein via the greater and lesser sciatic foramina; multiple smaller venous channels. The arterial supply includes the external iliac artery passing under the inguinal ligament to become the common femoral artery; the obturator artery passing into the thigh via the obturator foramen; the superior and inferior gluteal arteries from the posterior division of the internal iliac artery passing out of the pelvis via the greater and lesser sciatic foramina. The lymphatic drainage principally passes under the inguinal ligament, via the femoral and obturator canals and via the sciatic foramina, to drain into the pelvic lymphatic chains (Ch. 63). The somatic neural structures include the femoral, obturator and sciatic nerves and other minor branches of the lumbosacral plexus (Ch. 62). The autonomic neural structures include those running with the arterial supply and with the branches of the lumbosacral plexus. Cutaneous neurovascular structures also cross between the lower abdomen and pelvis into the skin and superficial tissues of the lower limb.
GENERAL ARRANGEMENT OF ABDOMINOPELVIC NEUROVASCULAR STRUCTURES
AUTONOMIC SUPPLY
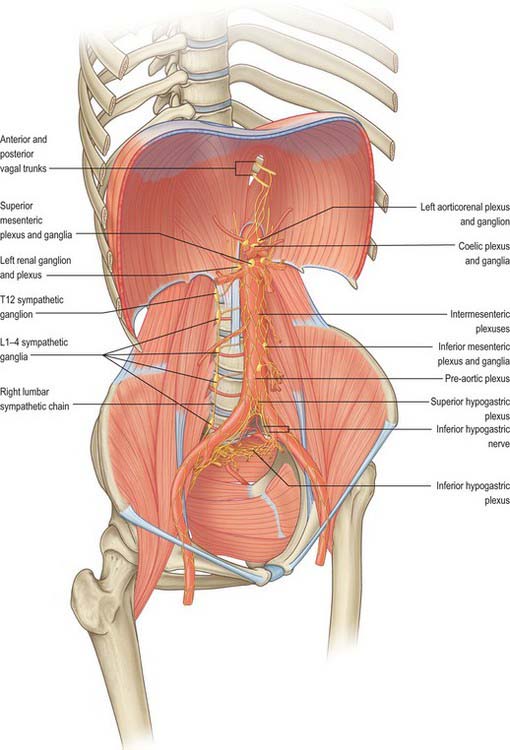
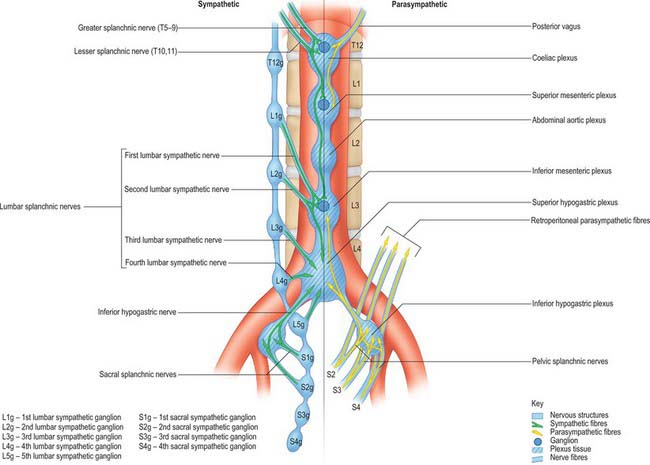
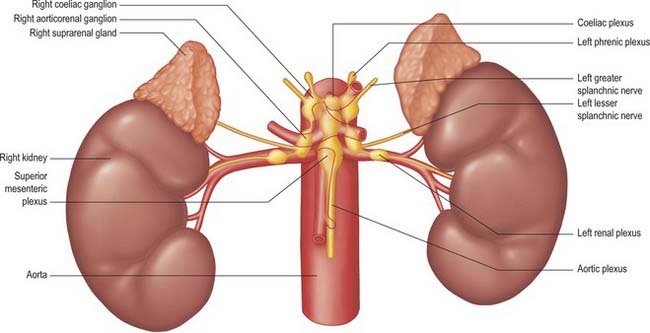
The autonomic supply to the abdominal and pelvic viscera is via the abdominopelvic part of the sympathetic chain and the greater, lesser and least splanchnic nerves (sympathetic), and the vagus and pelvic parasympathetic nerves (parasympathetic). Considerable ramification occurs between plexuses and ganglia, particularly in the major plexuses around the abdominal aorta, hence the descriptions tend to be simplifications based on the ‘main’ supply to each organ (Fig. 60.2). The details of the terminations of these fibres are given on page 1050.
Sympathetic innervation
Least splanchnic nerve
The least splanchnic nerve is derived from the medial, visceral branches of the 12th thoracic ganglia. It enters the abdomen running with the sympathetic chain under the medial arcuate ligament and runs inferiorly to enter the renal plexus. The trunk of the nerve enters the aorticorenal ganglion and may give branches to the lateral aspect of the coeliac ganglion. It is sometimes part of the lesser splanchnic nerve, when it forms a twig which enters the renal plexus just below the aorticorenal ganglion.
Lumbar sympathetic system
Vascular branches
Vascular branches from all the lumbar ganglia join the abdominal aortic plexus. Fibres of the lower lumbar splanchnic nerves pass to the common iliac arteries and form a plexus which extends along the internal and external iliac arteries. Many postganglionic fibres travel in the muscular, cutaneous and saphenous branches of the femoral nerve, supplying vasoconstrictor nerves to the femoral artery and its branches in the thigh. Other postganglionic fibres travel via the obturator nerve to the obturator artery. Considerable uncertainty persists regarding the exact path of the sympathetic nerve supply to the lower limb (Pick 1970). Sympathetic denervation of vessels in the lower limb can be effected by removing or ablating the upper three lumbar ganglia and the intervening parts of the sympathetic trunk; very rarely, this procedure is useful in treating vascular insufficiency of the lower limb.
Parasympathetic innervation
Pelvic splanchnic nerves
The pelvic splanchnic nerves are motor to the smooth muscle of the rectum, anus and bladder wall but inhibitory to the vesical sphincter. They supply vasodilator fibres to the erectile tissue of the penis and clitoris and are probably also vasodilator to the testes, ovaries, uterine tubes and uterus. They are visceromotor to the sigmoid and descending colon as far as the splenic flexure and distal transverse colon.
Abdominopelvic autonomic plexuses and ganglia
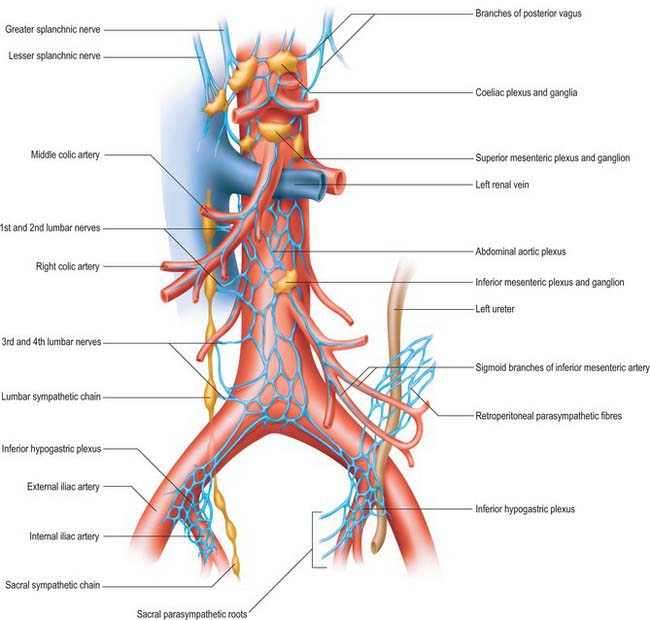
The abdominopelvic autonomic plexuses are somewhat variable and often fuse or are closely inter-related. The following descriptions recognize their main features (Figs 60.3, 60.4).
Coeliac plexus
The coeliac plexus is the largest major autonomic plexus, sited at the level of the twelfth thoracic and first lumbar vertebrae. It is a dense network uniting two large coeliac ganglia and surrounds the coeliac artery and the root of the superior mesenteric artery. It is posterior to the stomach and lesser sac, anterior to the crura of the diaphragm and the beginning of the abdominal aorta, and lies between the suprarenal glands. The plexus and ganglia are joined by the greater and lesser splanchnic nerves and branches from the vagus and phrenic nerves. The plexus extends as numerous secondary plexuses along adjacent arteries. The coeliac plexus is connected to, or gives rise to, the phrenic, splenic, hepatic, superior mesenteric, suprarenal, renal and gonadal plexuses (Fig. 60.5).
Abdominal aortic plexus (intermesenteric plexus)
The abdominal aortic plexus lies on the sides and front of the aorta, between the origins of the superior and inferior mesenteric arteries. It consists of 4–12 intermesenteric nerves, connected by oblique branches. It is continuous above with the superior mesenteric plexus and below with the superior hypogastric plexus, and is formed by parasympathetic and sympathetic branches from the coeliac plexus. It receives rami from the first and second lumbar splanchnic nerves (which contain sympathetic fibres). The abdominal aortic plexus is connected to the gonadal, inferior mesenteric, iliac and superior hypogastric plexuses.