Problem 31 A 68-year-old woman with breathlessness and yellow sputum
You are working in the emergency department one winter evening. A 68-year-old woman is brought in by ambulance, acutely short of breath. The history is obtained mainly from the patient’s daughter, because the patient is too breathless to talk, very tired and also a little drowsy. She says she has had difficulty with her breathing for many years and can now only walk at a slow pace for 100 metres and then has to stop due to breathlessness. She has had a smoker’s cough for as long as she can remember and has produced phlegm on most days for many years. She has had a number of chest infections this winter despite repeated courses of antibiotics and as a result the local doctor started her on a purple inhaler.
On this occasion the woman has been unwell for 1 week. During this time she has been producing thick yellow-green sputum which she has found difficult to cough up. She has been sitting up at night in a chair and has been unable to do anything due to her breathlessness and extreme fatigue. She has become nauseated and is eating very little. She has not had a temperature or shivers or chest pain. She has not noticed any blood in her sputum and she has not had ankle swelling. The patient has been on antibiotic tablets for 5 days but there has been no improvement.
The woman suffered a myocardial infarction at the age of 60 and underwent coronary bypass surgery. She has not had recurrent angina since then and is not on any cardiac medication. She does not have hypertension or diabetes mellitus. She had experienced pain in the left calf on walking up until the last 6 months when she has been more troubled by breathlessness.
She is on a salbutamol puffer, 2 puffs 4-hourly, fluticasone/salmeterol 250 mg/25 mg 2 puffs bd and amoxicillin 500 mg three times a day for the past 3 days. She currently smokes 5 cigarettes a day, but until 3 months ago smoked 30–60 a day and had done so since the age of 17. She claims she finds benefit from the smoking as it seems to aid the clearing of her sputum.
You ponder the differentials, and move on to examining the patient.
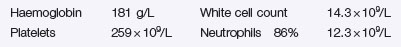
The following result is obtained:
Investigation 31.1 Arterial blood gas analysis on air
| pO2 | 41 mmHg |
| pCO2 | 75 mmHg |
| pH | 7.25 |
| HCO3 | 32 mmol/L |
Investigation 31.2 Arterial blood gas analysis on 3 L/min O2
| pO2 | 58 mmHg |
| pCO2 | 89 mmHg |
| pH | 7.21 |
| HCO3 | 32 mmol/L |
The electrolytes are normal other than bicarbonate.
The chest X-ray is shown in Figure 31.1.
An ECG shows a sinus tachycardia with a right axis deviation and a prominent R wave in lead V1.
Investigation 31.5 Arterial blood gases on air
| pO2 | 50 mmHg |
| pCO2 | 61 mmHg |
| pH | 7.40 |
| HCO3 | 34 mmol/L |
The patient is told firmly that she must stop smoking immediately.
Q.9
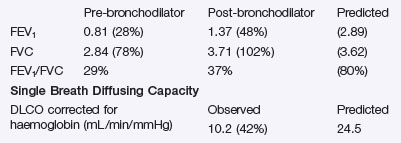
What do these results tell you? How will you manage the patient before discharge and in the future?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree