Problem 6 A 42-year-old woman with hypertension
You are a medical resident in a major teaching hospital. A 42-year-old woman is referred to your outpatient clinic for assessment and management of hypertension. The referral letter states that she was diagnosed with hypertension 8 years ago. She remains hypertensive (blood pressure 150/90 mmHg to 180/100 mmHg when checked by her general practitioner) despite treatment with three agents (irbesartan, indapamide and amlodipine). She was diagnosed with ‘anxiety’ several years ago, for which she has been taking diazepam. She has had no other major illnesses. There is no family history of hypertension.
The following results are available.
Investigation 6.1 Summary of results
| Fasting glucose (3.8–5.5 mmol/L) | 10 |
| Urea (2.7–8.0 mmol/L) | 7.3 |
| Creatinine (50–120 µmol/L) | 68 |
| eGFR (mL/min/1.73 m2) | >60 |
| Ionized calcium (1.1–1.25 mmol/L) | 1.31 |
| Total calcium (2.10–2.55 mmol/L) | 2.75 |
| Phosphate (0.65–1.45 mmol/L) | 1.27 |
| Plasma metanephrine | 18 100 pmol/L (<500 pmol/L) |
| Plasma normetanephrine | 9260 pmol/L (<900 pmol/L) |
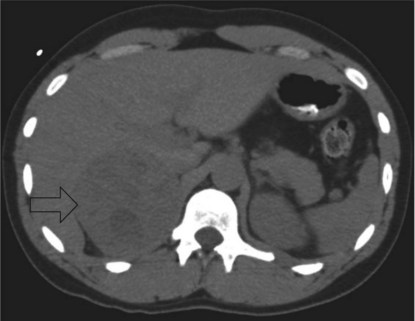
Some imaging studies are arranged and a CT scan of the abdomen performed. A representative slice is shown (Figure 6.1).
She undergoes a laparoscopic adrenalectomy and the large adrenal tumour is removed intact. As soon as the adrenal vein is ligated the blood pressure falls and the anaesthetist is able to reduce the alpha blockade. The opened surgical specimen is shown (Figure 6.2).
All medications are stopped immediately postoperatively.
Answers
She must be investigated for a secondary cause of hypertension.
A.2 The following components of the history should be clarified:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree