Problem 26 A 41-year-old man involved in a car crash
A 41-year-old man is brought in by ambulance to the emergency department of a tertiary hospital with trauma facilities from the scene of a car crash. The paramedic crew provides a history. The patient was a restrained driver in a sedan vehicle that had a head-on collision with another car whose occupant was pronounced dead at the scene. The car was not fitted with either driver or curtain airbags. There was significant intrusion of the engine block into the driver’s compartment and the patient was trapped for about 30 minutes before extraction, with full cervical spine immobilization, by the emergency services. The patient is uncertain about whether he lost consciousness or not, but ambulance officers report he seems a little confused with poor recollection of events and has an obvious contusion to his right temple. Ambulance officers also report the smell of alcohol on the patient’s breath.
During the ambulance journey from the scene of the crash the patient complained of shortness of breath and pain in the left side of his chest. He has been cardiovascularly stable throughout. The patient has been given oxygen by mask, one large-bore intravenous access has been obtained and 500 mL of crystalloid has been infused.
Your examination reveals the following:
A second wide-bore intravenous cannula is inserted into a peripheral vein and 1 L of a crystalloid solution administered rapidly. Blood samples are collected for cross-matching, complete blood picture and biochemistry. In addition forensic blood alcohol samples are obtained. The chest X-ray is shown in Figure 26.1.
The initial laboratory results are also unremarkable and his haemoglobin is 131 g/L.
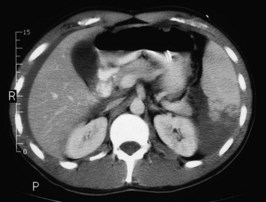
A CT scan of his head, cervical spine, chest, abdomen and pelvis is performed. A slice from the upper abdomen is shown in Figure 26.2.