Problem 29 A 25-year-old woman with chest pain and breathlessness
You are currently working in the emergency department on an evening shift. A 25-year-old woman has come to you for urgent assessment tonight with difficulty breathing and right-sided chest pain. The pain began suddenly 1 week ago. She describes it as sharp and worse on breathing in. It is now constant and has increased in severity. She has also become progressively more breathless on exertion over the last few days and is now unable to perform activities such as showering without feeling ‘out of puff’.
You ask her more history – she has not had a fever, cough or wheeze and she has never previously suffered any respiratory complaints. The woman has polycystic ovarian syndrome and has been using the oral contraceptive pill to help regulate her menses in the last couple of years. Her health has otherwise been good. She is an active smoker, averaging 10 cigarettes per day for the last 7 years.
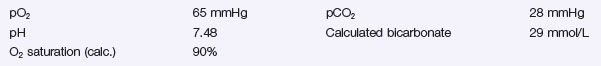
You examine her – she is obese with a weight of 110 kg. She is sweaty and looking unwell. She is taking short shallow breaths and her respiratory rate is 30 breaths/minute. Her temperature is 37.5°C, her pulse is 120 beats/minute and feels regular. Her blood pressure is 125/60 mmHg with oximetry showing oxygen saturation on room air of 88%. Her jugular venous pressure is visualised at 5 cm. Both heart sounds are present with no murmurs or pericardial rub audible. There are reduced breath sounds at both lung bases. No crackles, wheeze or pleural rub are heard. You note that there is tenderness behind her left calf but no associated leg swelling. Her admission CXR is reported as having mild basal atelectasis, but as being otherwise normal.
Complete blood picture and baseline electrolytes are normal.
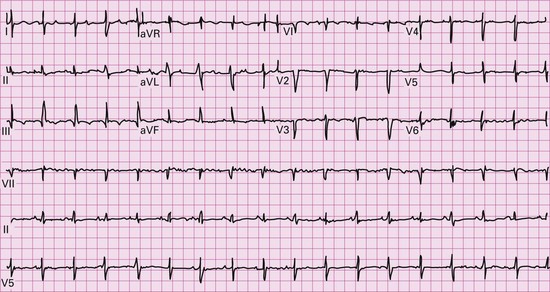
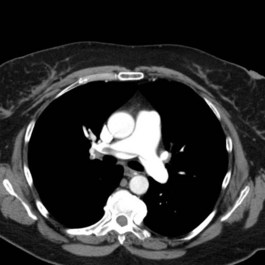
An imaging study is undertaken and two images from the sequence are shown (Figure 29.2). Her left Doppler showed an extensive clot into proximal femoral veins.
Q.4
What do these images show? What clinical signs may reflect the underlying severity of the condition?
Answers
• Pulmonary embolism (PE) is the most likely and important diagnosis to consider as it carries a significant mortality risk when untreated:
• Inflammatory pleurisy from pneumonia is less likely because more infective symptoms would be expected a week after onset (sputum production and constitutional symptoms) along with definite features of consolidation on chest X-ray and/or on clinical examination (bronchial breath sounds).
• Pericarditis is another condition that sometimes mimics pleurisy but does not usually cause hypoxia, unless associated with acutely decompensated heart failure.
Further specific questions should be asked to determine her pre-test probability of DVT/PE:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree