Atropine Overdose

CLASSIFICATION
Anticholinergic, antispasmodic, antidysrhythmic
ACTION
Inhibits action of acetylcholine. Primary affects are on the heart, exocrine glands, smooth muscles, and eye.
USES
• Antidysrhythmic—increases heart rate in symptomatic bradycardia, atrioventricular (AV) block.
• Preoperative—decreases secretions.
• Promotes mydriasis for retinal examination.
• Decreases intestinal hypermotility (diarrhea).
PRECAUTIONS AND CONTRAINDICATIONS
• Gastrointestinal (GI) problems—obstruction, ulcers, colitis, gastroesophageal reflux disease (GERD)
• Glaucoma, tachycardia, bladder obstruction (benign prostatic hyperplasia [BPH])
• Hyperthyroid, liver or renal disease, asthma, hypertension
ADVERSE EFFECTS
• Decreased sweating, which can lead to hyperthermia and flushing
• Central nervous system—toxic doses may cause delirium and hallucinations
• **Dry mouth, tachycardia**
• **Blurred vision,** urinary retention, **urinary hesitancy,** constipation
NURSING IMPLICATIONS
2. *Evaluate frequently for urinary retention, especially in older adult men with prostate problems.*
3. *Do not administer if patient has a tachycardia.*
4. *If used preoperatively, explain that warm, dry, flushed feeling may occur.*
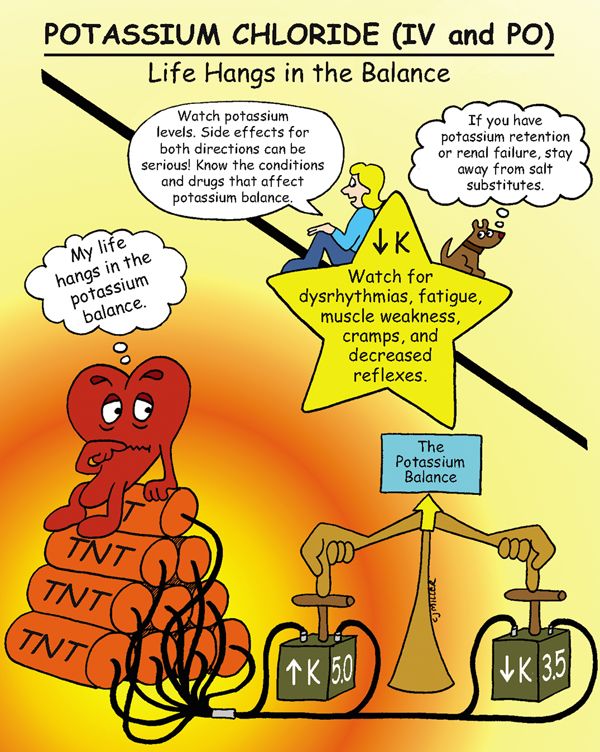
Potassium Chloride (Intravenous and Orally)

CLASSIFICATION
Electrolyte replacement
ACTIONS
Is necessary for nerve impulse conduction; maintains electrical excitability of the heart, and assists to regulate acid-base balance.
USES
• Prevent or correct (or both) potassium deficiency
CONTRAINDICATIONS
PRECAUTIONS
• Acute acidosis resulting in potassium shifts
SIDE EFFECTS
• **Gastrointestinal discomfort—nausea, vomiting, diarrhea**
• Hyperkalemia—(primarily from intravenous [IV] infusion of potassium) †ventricular tachycardia,† confusion, anxiety, dyspnea, weakness, and tingling
NURSING IMPLICATIONS
1. Give oral medication with a full glass of water with or after meals.
2. *Monitor serum potassium (3.5 to 5.0 mEq/L normal value).*
3. *Watch for signs of renal insufficiency—increased creatinine, increased blood urea nitrogen; stop potassium, and notify health care provider if symptoms of renal failure develop.*
4. †IV potassium must always be diluted before administering. Never administer potassium via IV push.†
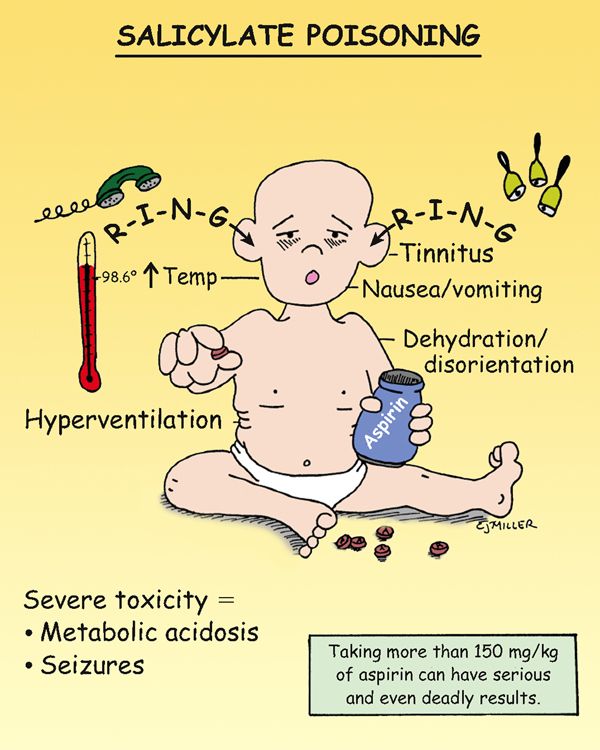
Salicylate Poisoning

PATHOPHYSIOLOGY
Initially, respiratory excitation occurs, producing a respiratory alkalosis. As toxicity occurs, a respiratory depression occurs, resulting in an increase in carbon dioxide levels, which produces respiratory acidosis. The respiratory acidosis is uncompensated because the bicarbonate stores are depleted during the early stages of poisoning. Metabolic acidosis results from the acidity of aspirin, along with an increased production of lactic and pyruvic acids.
SIGNS AND SYMPTOMS
• **Initial symptoms: tinnitus, sweating, headache, and dizziness**
• †Toxicity: hyperthermia, sweating, and dehydration; respiratory depression, resulting in respiratory acidosis, stupor, and coma†
TREATMENT
• Decrease gastrointestinal (GI) absorption—gastric lavage and activated charcoal.
• Provide oxygen or ventilation assistance as necessary.
• Treat for hyperthermia (external cool down, tepid water sponge bath), dehydration (intravenous hydration, balance pH, and electrolytes), and reverse acidosis (slow infusion of bicarbonate).
• Provide dialysis, if necessary. Hemodialysis may be necessary.
NURSING IMPLICATIONS
1. ‡Teach parents safe medication storage.‡
2. ‡Teach parents not to administer aspirin to children who are suspected of having a viral infection, especially chicken pox or influenza.‡
3. *Monitor respiratory status, blood gases, and the progression of symptoms.*
4. *Assist older patients to evaluate the combination of over-the-counter (OTC) medications for the presence of aspirin.*
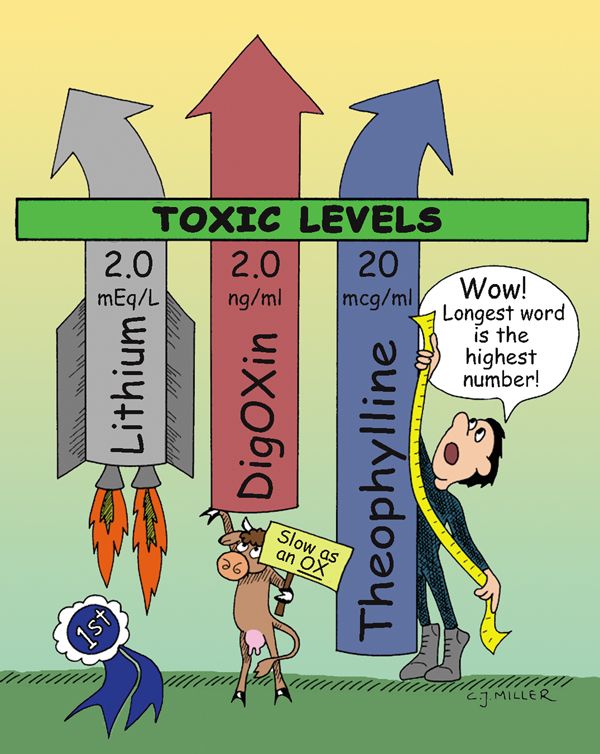
Toxic Levels of Lithium, Digoxin, and Theophylline

LITHIUM
• Therapeutic level: 0.8 to 1.4 mEq/L
• Toxic level: >2.0 mEq/L (levels should be kept below 1.5 mEq/L)
• ‡Levels are routinely monitored every 2 to 3 days initially, then every 1 to 3 months during therapy.‡
• *Sodium depletion is the most common cause of lithium accumulation.*
Signs and Symptoms
• **Side effects (at therapeutic levels) include fine hand tremors, polyuria, thirst, transient fatigue, muscle weakness, headache, and memory impairment.**
• Gastrointestinal (GI) effects are nausea, diarrhea, and anorexia.
• Toxic effects (1.5 to 2.0 mEq/L) include persistent gastrointestinal (GI) problems (vomiting, diarrhea), course hand tremors, hyperirritability, and poor coordination.
• Effects of †acute toxicity† (above 2.0 mEq/L) include ataxia, high output of dilute urine, electrocardiographic (ECG) changes, tinnitus, blurred vision, †severe hypotension,† and †seizures.† Symptoms may progress to †coma† and †death.†
DIGOXIN
• Optimal level: 0.5 to 0.8 ng/ml
• *Hypokalemia is the most common predisposing factor to toxicity.*
• ‡Patients should not interchange various brands because of variations in absorption.‡
Signs and Symptoms
• **GI signs include anorexia and nausea and vomiting.**
• Central nervous system signs are **fatigue** and visual disturbances.
• †Dysrhythmias—digoxin can mimic most dysrhythmias; if cardiac rate or rhythm changes during therapy, the health care provider should be notified.†
THEOPHYLLINE
• Optimal level: 5 to 15 mcg/ml
Signs and Symptoms
• *Aminophylline is the preferred form for intravenous (IV) administration. It must infuse slowly (25 mg/min or slower); too rapid IV infusion may cause hypotension, tachycardia, hyperventilation, and seizures.*
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree