Dawn Piarulli, R. Michelle Koolaee Table 9.1 summarizes the etiologies of inflammatory arthritis based on symptom duration. The duration of joint symptoms can implicate certain diagnoses over others. When the arthritis is acute (lasting a few days or less), one must immediately consider septic arthritis or crystal-induced arthritis (i.e., gout, pseudogout). Septic arthritis can occur secondary to organisms of bacterial, viral, or fungal origin. An arthrocentesis should be immediately performed to rule out this possibility as well as to evaluate for crystal-induced arthritis. See Case 47 for more information about septic and crystal-induced arthritis. TABLE 9.1 Differential Diagnosis for Inflammatory Arthritis Based on Duration of Symptoms When symptoms have been present for more than a few days but less than 6 to 8 weeks, one should consider subacute types of infectious or parainfectious arthritides such as poststreptococcal arthritis or viral arthritis such as parvovirus B19 arthritis. Another differential diagnosis to consider is reactive arthritis. Reactive arthritis (formally known as Reiter’s syndrome) is an acute inflammatory arthritis that can occur after genitourinary infections (i.e., Chlamydia) or after gastrointestinal infections like Yersinia, Salmonella, Shigella, Campylobacter, or Clostridium difficile. In a patient who presents with chronic arthritis (more than 6 to 8 weeks), it is reasonable to consider autoimmune illnesses, which include systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), or the seronegative spondyloarthropathies (SpAs), to name a few. Be mindful that arthritis due to tuberculous or fungal infections may fall into the chronic category if not detected early on. Arthritis is usually categorized into monoarthritis, oligoarthritis, or polyarthritis. These terms refer to the number of joints involved in arthritis. Oligoarthritis refers to ≤4 affected joints, whereas polyarthritis refers to five or more affected joints. The number of joints involved is important because the differential diagnosis for each class of arthritis is a bit different (although there can be overlap). Table 9.2 highlights the differential diagnosis according to the number of joints involved. TABLE 9.2 Differential Diagnosis for Inflammatory Arthritis According to the Number of Joints Involved When trying to determine what is causing chronic arthritis, it is important to determine whether a patient is suffering from an inflammatory arthritis or a noninflammatory arthritis. Inflammatory arthritis is associated with at least 30 minutes and often greater than 1 hour of morning stiffness. Patients with osteoarthritis can also have morning stiffness, but it usually lasts less than 20 minutes. Synovitis is the physical exam term used to indicate the finding of active inflammatory arthritis. A joint with synovitis may have bogginess, swelling, tenderness, and may or may not have a palpable effusion. Synovitis is not specific to any particular type of inflammatory arthritis; any type may have this finding. When an effusion is present with synovitis and no diagnosis has been made, arthrocentesis is critical to perform to help establish a diagnosis. See Case 47 for discussion on synovial fluid analysis. Table 9.3 summarizes ways in which inflammatory and noninflammatory arthritis differ. TABLE 9.3 Distinguishing Inflammatory Versus Noninflammatory Arthritis DIPs, first CMC, hips, knees, spine Asymmetric involvement of joints PIPs, MCPs, wrists, radiohumeral joint, glenohumeral joint, MTPs Symmetric involvement of joints Subchondral sclerosis and cysts Osteophytes Asymmetric narrowing (within one joint) Periarticular osteopenia Erosions Symmetric narrowing (within one joint) Bony enlargement Heberden’s/Bouchard’s nodes Synovitis Rheumatoid nodules in advanced disease In summary, this is a young female who presents with a chronic, polyarticular, symmetric arthritis affecting both small and large joints. RA is a likely diagnosis, given the involvement of bilateral small joints in conjunction with symptom duration of greater than 6 to 8 weeks. Other possibilities include SpA with peripheral joint involvement such as ankylosing spondylitis (AS), psoriatic arthritis (PsA), or reactive arthritis. Peripheral joint involvement refers to joints of the extremities (such as shoulders, elbows, wrists, MCPs, PIPs, distal interphalangeal joints [DIPs], knees, ankles, or metatarsal interphalangeal joints [MTPs]). Axial joint involvement refers to spinal or sacroiliac joint involvement, which the patient does not have. She has no rash, so PsA is less likely (although 10% of the time the arthritic symptoms may precede the rash). With no history of recent infections, reactive arthritis is less likely. Patients with Sjögren’s syndrome may also present with polyarticular inflammatory arthritis; however, she does not have any symptoms of keratoconjunctivitis sicca (dry eye) or xerostomia (dry mouth). Given the chronicity of her symptoms, an infectious cause of her arthritis would be very unlikely.
A 22-Year-Old Female With Joint Pain
Why is the duration of this patient’s joint pain important?
Duration
Differential Diagnoses to Consider
A few days or less
Septic arthritis (bacterial, fungal, or tuberculous), crystal-induced arthritis (gout/pseudogout)
More than a few days but less than 6 to 8 weeks
Viral arthritis (especially parvovirus B19), poststreptococcal arthritis, bacterial arthritis (bacterial, fungal, or tuberculous), reactive arthritis (which follows gastrointestinal or genitourinary infections)
Chronic/more than 8 weeks
Rheumatoid arthritis, systemic lupus erythematosus, scleroderma, sarcoidosis, Sjögren’s syndrome, chronic infections (tuberculous arthritis, fungal arthritis, Lyme disease)
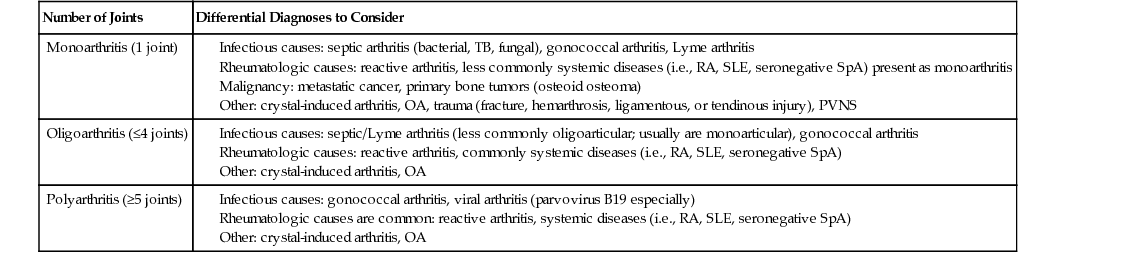
What is meant by the term oligoarthritis, and why is the number of joints involved in arthritis important?
Number of Joints
Differential Diagnoses to Consider
Monoarthritis (1 joint)
Oligoarthritis (≤4 joints)
Polyarthritis (≥5 joints)
Why is it important to ask about the duration of morning stiffness?
What is the definition of synovitis and what does it indicate?
Feature
Noninflammatory (Osteoarthritis)
Inflammatory (Rheumatoid)
Age of onset
Typically older patients (usually >50)
Any age
Morning stiffness
Morning stiffness <30 minutes
Morning stiffness >1 hour
Joint involvement
Radiographic findings
Effusions on exam
Occasionally
Frequently
Physical exam findings
How would you summarize the findings and the most likely differential diagnoses?
What are other physical exam findings in RA?
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


9 A 22-Year-Old Female With Joint Pain
Case 9
