8 CASE 8
LABORATORY STUDIES
Chest radiography: Enlarged left atrium and ventricle, interstitial pulmonary edema, and consolidation of the lower lung fields
PATHOPHYSIOLOGY OF KEY SYMPTOMS
Myocardial infarction causes damage to the ventricular tissue and impairs the pumping ability. Because the infarct was in the left ventricle in this patient, left ventricular pumping is impaired. This results in a decreased arterial blood pressure and an elevated pressure in the left atrium and pulmonary circulation. The elevated volume in the left atria causes the appearance of a third heart sound owing to the turbulent flow of blood during atrial filling (Fig. 8-1).
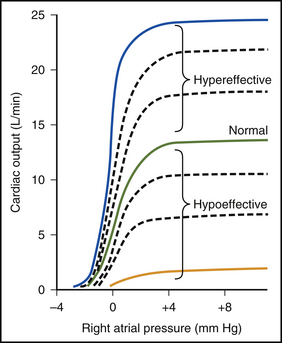
FIGURE 8–1 Cardiac output curves for the normal heart and for hypoeffective and hypereffective hearts.
(Redrawn from Guyton AC, Jones CD, Coleman TB: Circulatory Physiology: Cardiac Output and Its Regulation, 2nd ed. Philadelphia, WB Saunders, 1973.)
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


