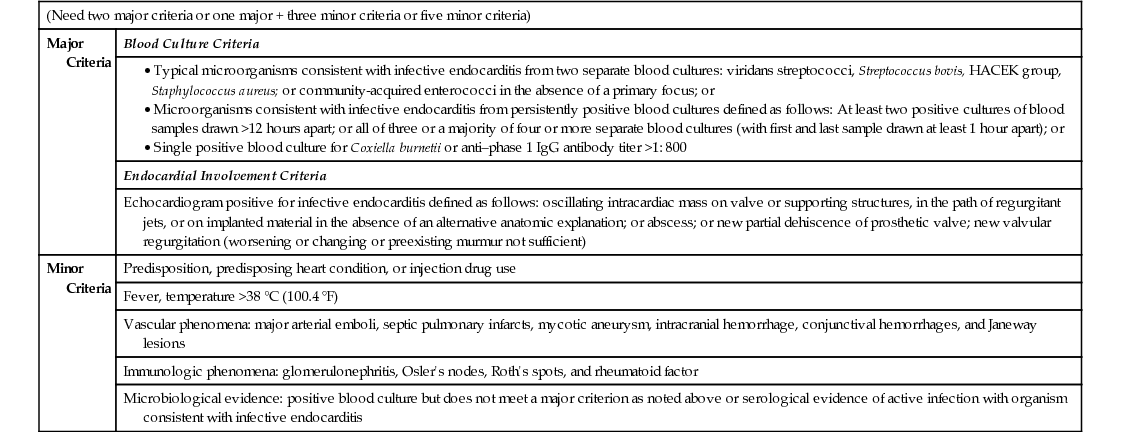
Arthur Jeng, Arzhang Cyrus Javan This patient has fevers but a paucity of other symptoms. Although pyelonephritis can cause fevers, he does not have any symptoms of either pyelonephritis (flank pain, nausea) or lower urinary tract infection (UTI) (dysuria, urinary frequency/urgency). Additionally, the UA does not demonstrate significant pyuria. Therefore, despite being labeled with the diagnosis of pyelonephritis, it is unlikely the reason for his fevers, and additional investigation needs to be performed. The differential diagnoses should include causes of subacute chronic fevers with a paucity of symptoms. This would include subacute bacterial endocarditis, indolent infections such as extrapulmonary tuberculosis, brucellosis (undulant fever), Q fever, typhoid fever, typhus (from Rickettsia), certain cancers (especially lymphoma, leukemia, and renal cell carcinoma), and autoimmune diseases. Human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS) can allow opportunistic organisms, such as Cryptococcus, cytomegalovirus (CMV), and Mycobacterium avium complex to cause fever with no localizing symptoms. It may also predispose patients to febrile noninfectious processes such as multicentric Castleman’s disease and lymphoma. To diagnose a UTI, three factors need to be satisfied: Because S. viridans does not cause UTIs and the patient does not have UTI symptoms, this is not the diagnosis. The bacteriuria is either a contaminant, or it is reflecting bacteremia (the nephrons filter the blood, often leading to pathogens leaking from blood into the urine). The microbiology data show significant bacteremia within S. viridans group, making subacute bacterial endocarditis the most likely diagnosis. As such, the patient needs an echocardiogram to evaluate for cardiac vegetations and any complications, including valvular dehiscence and/or myocardial/perivalvular abscess. In most hospitals, the initial echocardiogram to obtain is the transthoracic echocardiogram (TTE), as this is a noninvasive study that can be obtained very quickly. The modified Duke criteria can be used to assist in the evaluation and diagnosis of infective endocarditis (Table 7.2). A list of typical organisms that cause infective endocarditis is shown in Table 7.3. When a patient has infective endocarditis but the blood cultures do not grow any organisms, it is called culture-negative infective endocarditis. These pathogens are uncommon causes of infective endocarditis (Table 7.4) and require further evaluation through serology or PCR to establish a microbiological diagnosis. Detailed history-taking may uncover epidemiologic risk factors for acquiring one of these pathogens. TABLE 7.2 Modified Duke Criteria TABLE 7.3 Bacteria That Cause Infective Endocarditis and Prevalence From International Collaboration on Endocarditis (ICE) Prospective Cohort Study
A 56-Year-Old Male With 3 Weeks of Fever
What do you think about his admission diagnosis?
What is the differential diagnosis?
What do you think about this diagnosis?
What is the likely diagnosis now, and what other tests should you order?
(Need two major criteria or one major + three minor criteria or five minor criteria)
Major Criteria
Blood Culture Criteria
Endocardial Involvement Criteria
Echocardiogram positive for infective endocarditis defined as follows: oscillating intracardiac mass on valve or supporting structures, in the path of regurgitant jets, or on implanted material in the absence of an alternative anatomic explanation; or abscess; or new partial dehiscence of prosthetic valve; new valvular regurgitation (worsening or changing or preexisting murmur not sufficient)
Minor Criteria
Predisposition, predisposing heart condition, or injection drug use
Fever, temperature >38 °C (100.4 °F)
Vascular phenomena: major arterial emboli, septic pulmonary infarcts, mycotic aneurysm, intracranial hemorrhage, conjunctival hemorrhages, and Janeway lesions
Immunologic phenomena: glomerulonephritis, Osler’s nodes, Roth’s spots, and rheumatoid factor
Microbiological evidence: positive blood culture but does not meet a major criterion as noted above or serological evidence of active infection with organism consistent with infective endocarditis
Staphylococci
Cases (%) from ICE Cohort
Staphylococcus aureus
31.6
Coagulase-negative staphylococci
10.5
Streptococci
Viridans group streptococci
18
Streptococcus gallolyticus (bovis)
6.5
Other streptococci (β-hemolytic streptococci, nutritionally variant streptococci)
5.1
Enterococcus
10.6
HACEK Group
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

7 A 56-Year-Old Male With 3 Weeks of Fever
Case 7