CASE 67
An 18-year-old male college student was brought to the emergency department of a hospital with the complaints of fever, chills, and pain while walking.
PHYSICAL EXAMINATION
LABORATORY STUDIES
Diagnostic Work-Up
Table 67-1 lists the likely causes of illness (differential diagnosis). A clinical diagnosis of acute osteomyelitis was considered. Microbiologic diagnosis of acute osteomyelitis is often made by CT-guided aspiration. Investigational approach to delineating the etiology may include
TABLE 67-1 Differential Diagnosis and Rationale for Inclusion (consideration)
Rationale: Skin infections may be deep seated with an abscess (which exhibits fluctuance of the area), or mainly cellulitis (superficial redness and warmth). Gas gangrene would have crepitance on palpation due to the presence of gas. Skin cancers may manifest with similar lesions, but usually in older individuals. Sarcomas may manifest with skin or soft-tissue lesions. TB classically causes osteomyelitis of the vertebrae, called Pott disease, although other areas may be seen; overlying cellulitis is uncommon in such cases. S. aureus is the most common cause of skin and soft-tissue infections. Other causes are much less common and cannot be distinguished clinically, although the history of a traumatic wound makes some of the above organisms (e.g., Salmonella) less likely. Pseudomonas is often associated with IV drug users, and Salmonella with patients with sickle cell disease.
MICROBIOLOGIC PROPERTIES
Species belonging to the genus Staphylococcus are Gram-positive cocci that occur individually, in pairs, and in irregular grapelike clusters (Fig. 67-2A). They are nonmotile, nonspore forming, and catalase positive. The cell wall contains peptidoglycan and teichoic acid. These bacteria are resistant to temperatures as high as 50°C, to high salt concentrations, and to drying. Colonies on sheep blood agar are usually large (6 to 8 mm in diameter), smooth, and translucent; colonies of most strains are β-hemolytic and pigmented, ranging in color from cream-yellow to orange (see Fig. 67-2B). The ability to clot plasma (coagulase activity) is generally an accepted criterion for the identification of S. aureus. One such factor, bound coagulase, also known as clumping factor, reacts with fibrinogen to cause organisms to aggregate (a widely used key diagnostic test in the hospital laboratory). Another factor, extracellular coagulase, reacts with prothrombin to form thrombin, which can convert fibrinogen to fibrin (the tube or slide coagulase test is also used in the diagnostic laboratory).
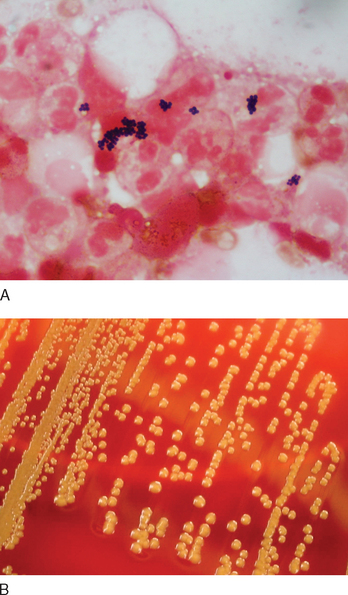
FIGURE 67-2 A, Gram stain of Staphylococcus aureus from a skin abscess. B, Culture of Staphylococcus aureus.
(A, Courtesy of Dr. Dominick Cavuoti, Department of Pathology, University of Texas Southwestern Medical School, Dallas, TX; B, Courtesy of Lisa Forrest, Department of Microbiology, University of Texas Southwestern Medical Center, Dallas, TX.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree