51 CASE 51
PATHOPHYSIOLOGY OF KEY SYMPTOMS
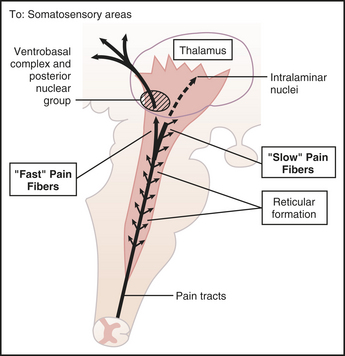
Fast pain is carried along myelinated Aδ fibers that synapse in the dorsal horn and ascend through the neospinothalamic tract to the thalamus and then on to the somatosensory cortex (Fig. 51-1). Within the spinal cord, glutamate is a neurotransmitter secreted at Aδ synapses. Slow pain is carried along the unmyelinated C fibers, which make polysynaptic connections in the spinal cord and ascend through the paleospinothalamic tract to the brain stem and thalamus. Within the spinal cord, substance P is the neurotransmitter released at C fiber synapses. The multiple synaptic connections transmitting slow pain mean that slow pain is very poorly localized on a somatotopic map.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree