CHAPTER 5 Integrative Neuromuscular Acupoint System
INTRODUCTION
The INMAS protocol resonates with the Western practitioner, thus facilitating its incorporation into pain management. Mechanisms of acupuncture are clarified in terms of their peripheral and central effects (see Chapters 3 and 4) and are explained using basic neuroscientific terminology and concepts that are based on the scientific and clinical discoveries of the last 40 years.
THREE TYPES OF ACUPOINTS
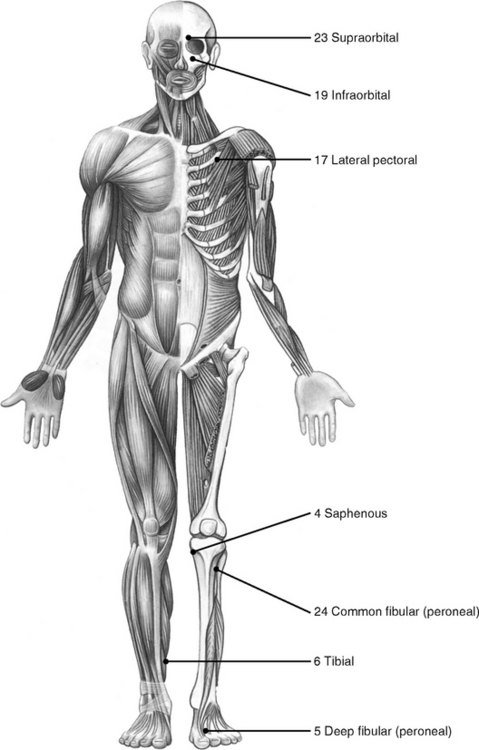
A chronic pathological condition can gradually result in more than 100 tender HAs in the body. Usually other tender HAs develop around what are known as the 24 primary HAs that appear first in the body. For instance, the H1 deep radial acupoint (Figure 5-1) is tender in almost everyone. If homeostasis declines or if an elbow or arm is injured, more tender acupoints appear along the deep radial nerve from H1 distally toward the wrist. Thus, the practitioner need only remember the 24 primary HAs to know all other potential HAs.
The combination of the three types of acupoints forms a universally standardized protocol for all pain symptoms; at the same time this protocol ensures an individualized approach, as is practiced in TCM, by identifying and treating the specific SAs of each patient. In other words, when treating patients, primary HAs are the same for every patient, whereas SAs are individualized symptomatic points. Different SAs require different PAs according to their neurosegmental connection. Thus this protocol contains both standardization and individualization.
The following example explains how we can use one principal protocol to treat two different pain symptoms, elbow pain and knee pain. More detailed instruction is provided in Chapter 6.
| Patient A (with elbow pain) | Patient B (with knee pain) | |
|---|---|---|
| HAs | Primary HAs | Primary HAs (same as patient A) |
| SAs | Locate SAs in elbow and arm | Locate SAs in the knee, thigh, and leg |
| PAs | Use PAs along C4-T1 | Use PAs along L2-5 |
THE RANDOM AND PREDICTABLE PATTERNS OF TENDER ACUPOINT FORMATION
All acupoints consist of peripheral nerve fibers, including the sensory and postganglionic nerve fibers and other soft tissues (see Chapter 1). Acupoints become tender in two distinguishing patterns: the random pattern of SAs and the predictable pattern of HAs.
As previously explained, when homeostasis declines, homeostatic acupoints are gradually transformed from a latent phase (nonsensitive) to passive or active phases. In general, HAs appear symmetrically in predictable locations and predictable sequential order in the human body, and this is referred to as the predictable pattern of tender HA formation. There can be more than 100 HAs in some patients; the first 24 HAs are shown in Figure 5-1. All other HAs appear around these 24 primary HAs, as discussed previously.
The three pathophysiologic phases of acupoints reveal the quantitative and qualitative dynamics of an acupoint: when pathologic factors persist, the number, size, and sensitivity of tender HAs and SAs increase. With proper treatment, the number of tender acupoints decreases and the sensitivity of each acupoint subsides (see Chapters 2 and 3). In the absence of proper treatment or when the self-healing potential is impaired, the size of an acupoint will increase and it will finally become a permanent pathologic structure such as a palpable nodule in the muscle.
There are no “sham” acupoints (see Chapter 4). Stimulated by acupuncture needling, any sensory nerve fiber, sensitized or not sensitized, will produce and send electrical signals to the spinal cord and the brain. Important acupoints, such as the 24 primary acupoints, provide stronger signals, and “sham” acupoints provide weaker signals.
NEUROANATOMY OF 24 PRIMARY HOMEOSTATIC ACUPOINTS
For 30 years Dr. H.C. Dung studied the pathophysiology of HAs in both clinical practice and laboratory research. He found that as many as 110 HAs may develop when homeostasis declines. Of these, 24 acupoints are the most important, as discussed previously.1
This discovery of HAs and their quantitative relation to homeostasis makes it possible to evaluate the pathophysiological condition (the self-healing potential) of a patient and predict the duration and prognosis of the acupuncture treatment (Chapter 6).
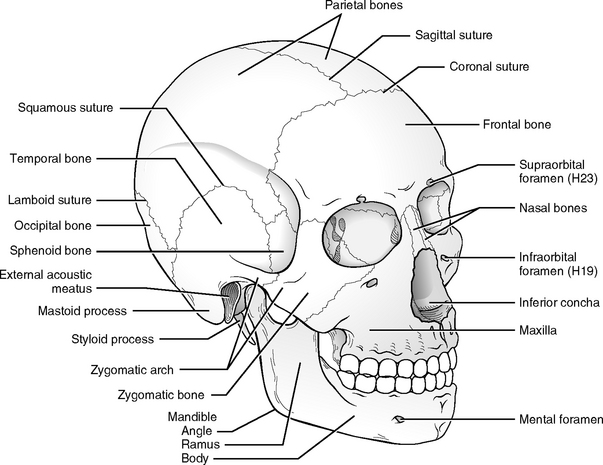
The 24 primary acupoints are named with their homeostatic sequence number, followed by the name of the related peripheral nerves or anatomic landmarks (see Figure 5-1). Consider, for example, the H1 deep radial acupoint. H1 means that this acupoint is the first of all the HAs to become tender on the body, and deep radial indicates that this acupoint is located on the deep radial nerve. Acupoint H19 infraorbital is located on the infraorbital foramen where the infraorbital nerve emerges and usually becomes tender after the H18 iliotibial point.
All the acupuncture needling methods described in the following section apply to prone or supine positions. The actual location of an acupoint varies in different patients. To achieve the best results, a practitioner should always palpate the body to locate the actual acupoints before needling them. The 24 primary homeostatic acupoints (see Figure 5-1) are described below according to body region.
Homeostatic Acupoints on the Head and Neck
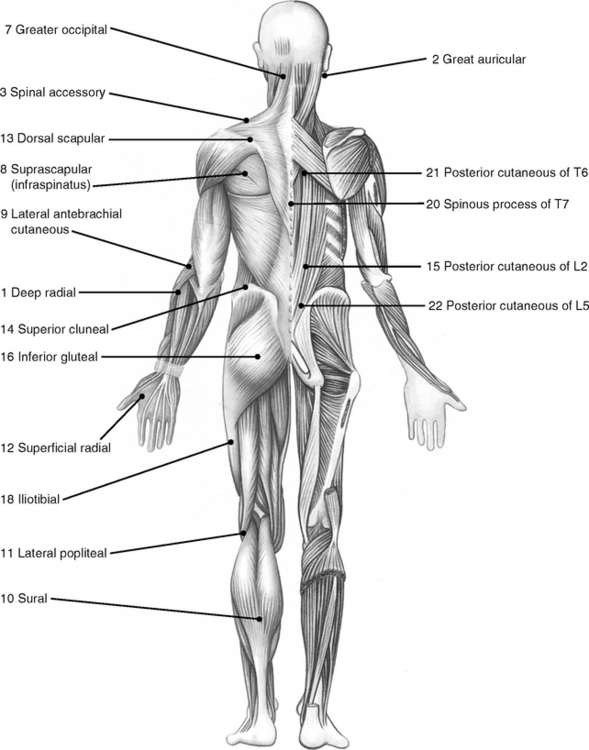
H19 Infraorbital
This acupoint is located exactly on the infraorbital foramen (Figure 5-2). The infraorbital nerve, a cutaneous nerve from the maxillary branch (V2) of the trigeminal nerve, passes the foramen and innervates the facial skin. To avoid hematoma use 38- or 36-gauge needles (diameter, 0.18 or 0.20 mm, respectively). The depth for needling ranges from 2 to 5 mm.
H23 Supraorbital
This acupoint is formed right on the supraorbital notch, which is the passage for the supraorbital nerve (see Figure 5-2). This cutaneous nerve from the ophthalmic branch (V1) of the trigeminal nerve extends to the top of the head. The method of needling this point is similar to the H19 infraorbital.
Clinical Notes
Because the supraorbital nerve is smaller than the infraorbital nerve, the H23 supraorbital becomes tender after the H19 infraorbital does (see Chapter 1). For example, the H19 infraorbital is always tender in a patient with a slight headache. If the headache lingers for some time, the H23 supraorbital becomes tender, too. If the headache continues to deteriorate, other points in the face, such as the mental nerve (V3), the zygomaticofacial nerve (V2), and the zygomaticotemporal nerve, also appear tender. More tender points indicate that the symptom is more chronic and more severe and requires more treatments.
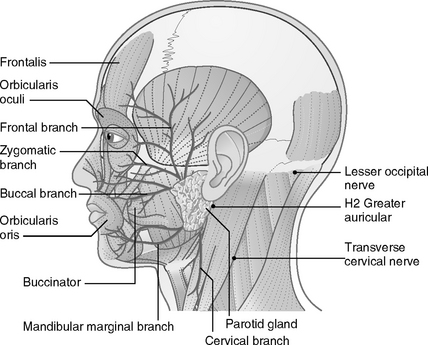
When treating patients with facial problems such as temporomandibular pain, chronic sinus pain, or facial paralysis, other points innervated by the facial nerve (VII) (Figure 5-3) should be carefully palpated and selectively needled according to the individual symptom.
H2 Greater Auricular
This acupoint is located just behind the earlobe and on the anterior border of the sternocleidomastoid muscle (see Figure 5-3). The greater auricular nerve is one of the four branches from the cervical nerve plexus (CNP, C2-4). The anterior rami of C2 to C4 interconnect to form the cervical nerve plexus. The CNP lies deep below the internal jugular vein and the sternocleidomastoid muscle. Four cutaneous branches from the CNP emerge around the middle of the posterior border of the sternocleidomastoid muscle.
The greater auricular nerve curves over and ascends obliquely toward the earlobe and the angle of the mandible. This nerve bundle surfaces through the investing fascia just below the earlobe and divides into branches to supply the skin on the inferior part of the ear and the area extending from the mandible to the mastoid process. The three acupoints formed by the CNP are shown in Figure 5-3.
Clinical Notes
Several acupoints on the neck are formed by three other nerves derived from the CNP. These nerves are the (1) lesser occipital nerve, which forms an acupoint located on the insertions between the sternocleidomastoid and the trapezius muscles on the occipital bone; (2) the transverse cervical nerve, which curves around the middle of the posterior border of the sternocleidomastoid and then passes transversely to the anterior border of the same muscle (several acupoints are formed over the anterior triangle of the neck); and (3) the supraclavicular nerve, which divides into medial, intermedial, and lateral branches. These nerves send small branches to the skin of the neck and then emerge from deep fascia just superior to the clavicle to supply the skin over the anterior aspect of the chest and shoulder. When needling tender acupoints in this area, a practitioner always should pay attention to the direction and depth of the needling so as not to puncture the lung. A safe needling method is suggested later in this chapter.
H7 Greater Occipital
This acupoint is located at the base of the occipital region, 2 or 3 cm from the midline (see Figure 5-1). This acupoint can be palpated easily because it is tender in more than 95% of patients. The dorsal rami of the C2 spinal nerve form the greater occipital nerve. This nerve emerges between the posterior arch of the atlas (C1) and the lamina of the axis (C2), below the small muscle obliquus capitis inferior. It then surfaces to supply the skin of the occipital region.
Clinical Notes
The H7 great occipital is frequently used because many symptoms can be traced to the problems of the neck. Neck-related problems are discussed in detail in Chapter 9. For effective treatment, we usually use needles of gauge 34 (diameter: 0.22 mm). The depth varies from 2 to 4 cm, depending on the thickness of the patient’s neck tissues.
H3 Spinal Accessory
The spinal accessory nerve (XI) originates from both cranial roots (nucleus ambiguus in medulla) and spinal roots (C1 to C6), and it contains both afferent (sensory) and efferent (motor) fibers. The branch of the spinal accessory nerve enters the trapezius muscle at the point over the shoulder bridge in the middle of the front edge of the upper trapezius muscle (see Figure 5-1). This acupoint is a neuromuscular attachment point.
Clinical Notes
The H3 spinal accessory appears tender in more than 98% of the population. We use a needle no more than 2.5 cm long and insert the needle perpendicularly to the skin. Practitioners should be extremely careful when needling this point because the apex of the lung is just below this point. We suggest four needling methods in Chapter 9. A practitioner can choose the method he or she is most comfortable with or explore other safe methods. Another branch of the spinal accessory nerve also innervates the sternocleidomastoid muscle, but the acupoints formed in that muscle are less important.
Other Facial Acupoints
Two cranial nerves, the trigeminal nerve (V) and the facial nerve (VII; see Figure 5-3), are involved in the formation of facial acupoints. The trigeminal nerve contains both sensory (afferent) and motor (efferent) nerves and is responsible for general sensations in the skin of the face and front of the head as well as controlling the chewing muscles. The two types of facial muscles are the muscles of mastication (chewing) and the muscles of facial expression. Two important muscles of mastication, the temporalis and masseter muscles, are innervated by the motor nerves of the trigeminal nerve. The acupoints formed in those two muscles are essential in treating some headaches and facial symptoms such as temporomandibular joint syndrome (TMJ) and facial paralysis.
Homeostatic Acupoints on the Upper Extremity
The large nerve network of the brachial plexus supplies the upper extremities. The brachial plexus is formed by the union of the ventral rami of nerves C5 to C8 and most of the ventral ramus of T1 (Figure 5-4). To supply the upper extremities, these five rami interconnect to form three nerve trunks: upper (C5-6), middle (C7), and lower (C8 and T1). Each trunk splits into anterior and posterior divisions. All the posterior divisions unite to become the posterior cord, which has two major nerves, the axillary and radial nerves. The anterior divisions form the lateral cord and the medial cord. The lateral cord becomes the musculocutaneous nerve, and the medial cord the ulnar nerve. The union of fibers from both the lateral and the medial cords forms the median nerve. The small branches from the upper trunk and the three cords supply the shoulder (back and front); the five major terminal nerves are made up of the three cords innervating the free arm. Six primary homeostatic acupoints are located in the upper extremities: one on the chest, two on the shoulder, two on the forearm, and one on the hand. Here we discuss only the major nerves that give rise to the primary homeostatic acupoints.
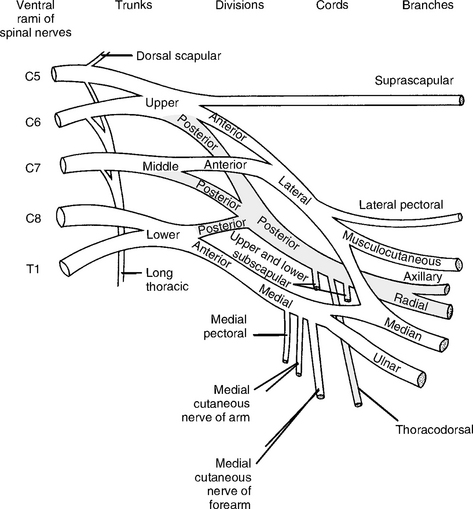
Figure 5-4 Diagram of the brachial plexus. The small nerve to the subclavius, from the upper trunk, is omitted.
(Modified from Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders.)