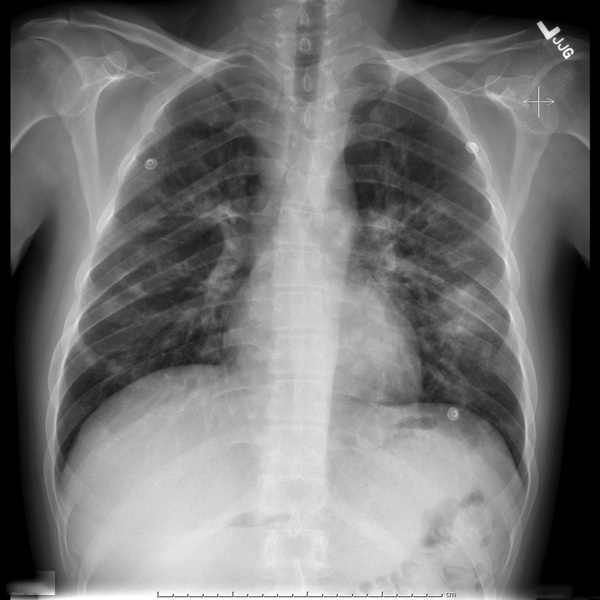
Mark Sims, Raj Dasgupta Cough is broadly characterized on the basis of duration. Acute cough lasts for less than 3 weeks, subacute cough lasts for 3 to 8 weeks, and chronic cough lasts more than 8 weeks. These designations are helpful, especially in an outpatient setting, as they can focus our differential diagnosis. Acute cough is typically infectious, with upper and lower respiratory tract infections being the most common causes. Subacute and chronic cough have a broader differential. The most common causes of chronic cough are actually benign. These are gastroesophageal reflux disease, cough variant asthma, and upper airway cough syndrome (previously known as postnasal drip). A thorough history and physical exam should elucidate these causes and rule out other more serious underlying disease. The presence of fever, constitutional symptoms, dyspnea on exertion, or hemoptysis should trigger expanded evaluation as these indicate potentially serious pathology. Finally, the age and underlying comorbidities that may alter the differential should be considered. As a clinician it is important to be familiar with the indications and uses of prophylactic regimens in HIV patients. Bactrim is used as primary prophylaxis for Pneumocystis jirovecii pneumonia (PCP) when the CD4 count is less than 200 and for Toxoplasmosis gondii when the CD4 count is less than 100. Azithromycin is used as primary prophylaxis for mycobacterium avium complex when the CD4 count is less than 50. Therefore, one can assume the patient’s CD4 count was less than 50 at the time of diagnosis and that he is profoundly immunosuppressed. It is important to note that in certain endemic or resource-limited regions, screening for tuberculosis, histoplasmosis, coccidiomycosis, and cryptococcosis may be necessary. Kaposi sarcoma (KS) is found in advanced HIV. It is a neoplastic, vascular lesion. Initial treatment for this disease is highly active antiretroviral therapy (HAART). However, progression on HAART may necessitate the use of cytotoxic chemotherapy. Bacillary angiomatosis is characterized by similar smaller, red to violet, pedunculated papules. It is caused by Bartonella spp. and treated with antibiotic therapy. Definitive diagnosis is by skin biopsy with Warthin–Starry stain showing clumps of tangled, dark bacilli. The skin lesions tend to be faster growing, more numerous, less erythematous, and smaller. Especially if cytotoxic chemotherapy is being considered, this diagnosis should be excluded with skin biopsy. The CXR reveals bilateral, scattered, patchy pulmonary infiltrates. There is a predominant mass located in the left lower lobe or lingula of the upper lobe. A lobar infiltrate can be more accurately located. An upper lobe infiltrate will obscure the left heart border and a lower lobe infiltrate will obscure the diaphragm. The same concept is true for the right middle lobe and lower lobe obscuring the right heart border and diaphragm, respectively. This patient should be placed in airborne respiratory isolation given the high risk of active pulmonary tuberculosis. The risk of tuberculosis doubles within the first year of diagnosis of HIV. The risk of activation increases with declining immunity such that 1 out of 10 new diagnoses of tuberculosis occur in those with HIV. Respiratory isolation is defined as a single patient, negative pressure room with a double door. All contacts should be trained in the use of an N-95 mask respirator. The “95” refers to the percentage of filtration capacity and is only effective when both the mouth and nose are covered. Whenever the patient is outside of the room for procedures or tests, he or she should wear a surgical mask, and exposure to other patients should be minimized.
A 31-Year-Old Male With Human Immunodeficiency Virus, Cough, and Shortness of Breath
How is a cough characterized?
Based on this drug regimen, what can one presume about the patient’s HIV status?
What is the skin lesion pictured in Figure 5.1?
What other skin lesion mimics KS?
Describe the findings on the CXR (shown in Fig. 5.2).
What is the next appropriate step in management?
How do you evaluate for and manage a potential case of active tuberculosis?
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


5 A 31-Year-Old Male With Human Immunodeficiency Virus, Cough, and Shortness of Breath
Case 5

