Antihypertensives

ACTIONS
Antihypertensive drugs act on the vascular, cardiac, renal, and sympathetic nervous systems. They also act to lower blood pressure (BP), cardiac output, and peripheral vascular resistance.
USES
• Control mild-to-severe hypertension
CONTRAINDICATIONS
• Cerebrovascular insufficiency
PRECAUTIONS
• Uncontrolled congestive heart failure, thyrotoxicosis
• Beta blockers can mask symptoms of hypoglycemia in patients with diabetes
• Hepatic and renal dysfunctions
SIDE EFFECTS
• **Hypotension, sedation, sexual dysfunction**
• Calcium channel blockers—bradycardia, peripheral edema, constipation
• Beta blockers—bradycardia, decreased atrioventricular (AV) conduction, reduced cardiac contractility, †bronchoconstriction†
NURSING IMPLICATIONS
1. *Monitor vital signs.*
2. ‡Teach patients about orthostatic hypotension for initial dosing (e.g., get up slowly) and other lifestyle changes—weight reduction, sodium restriction, and daily exercise.‡
3. *Monitor electrolyte, hepatic, and renal serum blood studies.*
4. *Avoid abrupt withdrawal of drug; may cause rebound phenomenon of excessive rise in BP.*
5. *Methyldopa (Aldomet) is the drug of choice for hypertension in pregnancy.*
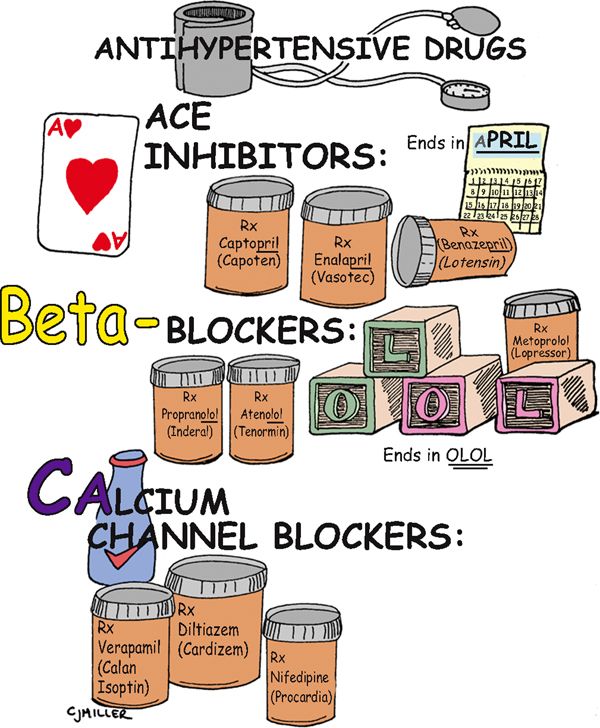
Antihypertensive Drugs

CLASSIFICATION
Blood pressure is regulated by cardiac output (CO) and peripheral vascular resistance (PVR). Medications that influence either one of these systems lead to blood pressure control. Antihypertensive drugs that influence these systems to lower the blood pressure are angiotensin-converting enzyme (ACE) inhibitors, beta-adrenergic blockers, and calcium channel blockers (CCBs).
ACTIONS
• A—ACE inhibitors block the conversion of angiotensin I to angiotensin II, a vasoconstrictor. This block causes vasodilation and therefore decreases PVR, resulting in a decrease in blood pressure. Aldosterone is also blocked, causing a decrease in sodium and water retention.
• B—Beta-adrenergic blockers block the beta1-receptors in the heart, which results in decreased heart rate and decreased force of contraction.
• C—CCBs block calcium influx into the beta-receptors, decrease the force of the myocardial contraction, reduce heart rate, and decrease PVR.
USES
• Mild-to-moderate essential hypertension
• Either as separate drugs or frequently in combination with another drug
NURSING IMPLICATIONS
1. *Initial drug selection starts with a thiazide diuretic, typically followed by a beta-adrenergic blocker or an ACE inhibitor or CCB.*
2. ‡Take medication as prescribed; do not stop abruptly.‡
3. ‡Teach patient never to double-up on doses if a dose is missed.‡
4. ‡Change positions slowly; watch for postural hypertension.‡
5. ‡Avoid over-the-counter medications.‡
6. ‡Take caution in hot weather, hot showers, hot tub baths, or prolonged sitting or standing because these may aggravate low blood pressure.‡
7. ‡Teach patients about multidrug therapy; instruct them not to discontinue a previous antihypertensive medication when another medication is started.‡
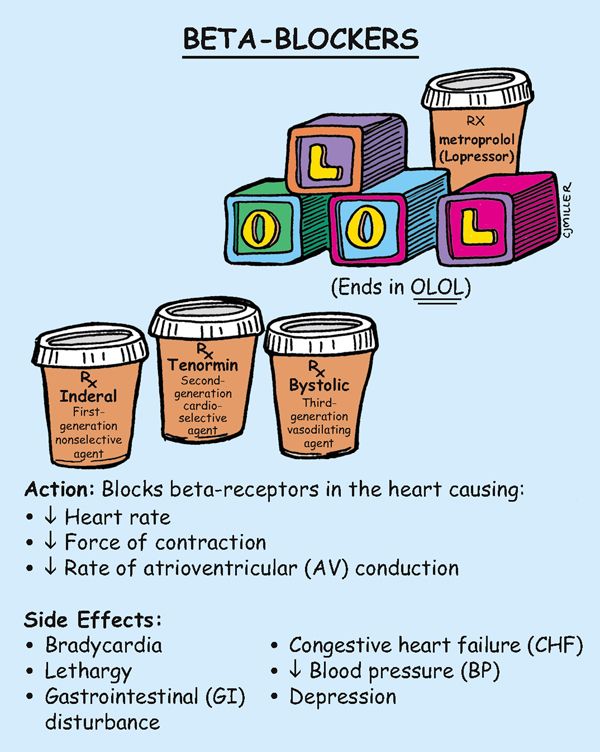
Beta-Blockers

ACTIONS
Beta1 action is primarily on the heart—decreases rate, decreases force of contraction, and delays impulse conduction. Beta2 action is primarily on the heart, but it also blocks receptors in the lungs and can cause bronchoconstriction.
USES
• Uncomplicated hypertension, dysrhythmias; angina
CONTRAINDICATIONS
• Bradydysrhythmias, atrioventricular (AV) block
• Beta2 in chronic respiratory problems
PRECAUTIONS
• Hepatic and renal dysfunction, diabetes
• History of depression, heart failure
SIDE EFFECTS
• Headache, flushing, dizziness, **fatigue, weakness,** bradycardia
• Postural hypotension, †bronchospasm, bronchoconstriction†
• Decreased cardiac output, †congestive heart failure (CHF)†
NURSING IMPLICATIONS
1. Assess for symptoms of heart failure.
2. ‡Instruct the patient to report any weakness, dizziness, or fainting.‡
3. *Before giving, evaluate the patient’s blood pressure and pulse for significant changes. Hold if systolic blood pressure is below 90 mm Hg.*
4. *Monitor patients with diabetes, because tachycardia (a symptom of hypoglycemia) is often masked as a result of the beta1 blockade.*
5. Propranolol (Inderal) has both beta1– and beta2-receptor blocking actions and is considered nonselective; metopropol (Lopressor) is cardioselective, which means it blocks only beta1. Atenolol (Tenorim) is considered a cardioselective beta1 blocker, but it blocks beta2 at high doses. Nebivolol (Bystolic) vasodilates and other third-generation drugs block beta1, beta2, and alpha1 (carvedilol [Coreg]).
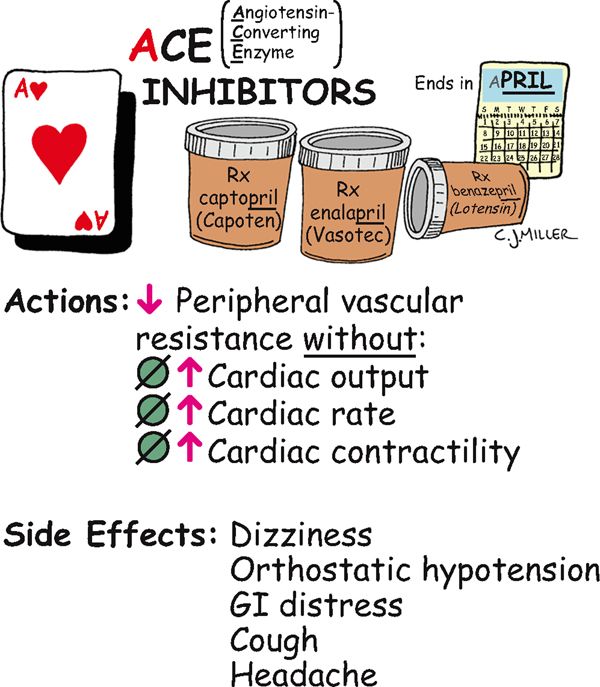
Angiotensin-Converting Enzyme (ACE) Inhibitors

ACTION
Suppress formation of angiotensin II from the renin-angiotensin-aldosterone system, reduce peripheral resistance, and improve cardiac output.
USES
CONTRAINDICATIONS
• Second- and third-trimester pregnancies
PRECAUTIONS
• Renal impairment, collagen vascular disease
SIDE EFFECTS
• Headache, dizziness, **postural hypotension (especially the first dose)**
• Rash, †angioedema†
• **Altered sense of taste, hyperkalemia**
• **Nagging, nonproductive cough**
NURSING IMPLICATIONS
1. Regularly *monitor blood pressure,* especially for 2 hours after the first dose, because severe first-dose hypotension often develops.
2. ‡Teach patient to rise slowly from a lying to a sitting position to reduce postural hypotensive effects.‡
3. *Before administering, assess the patient for history or presence of renal impairment.*
4. *Administer on an empty stomach for best absorption.*
5. ‡Teach patient to notify health care provider if cough develops.‡
6. ‡Teach patient to avoid potassium supplements or potassium-containing salt substitutes.‡
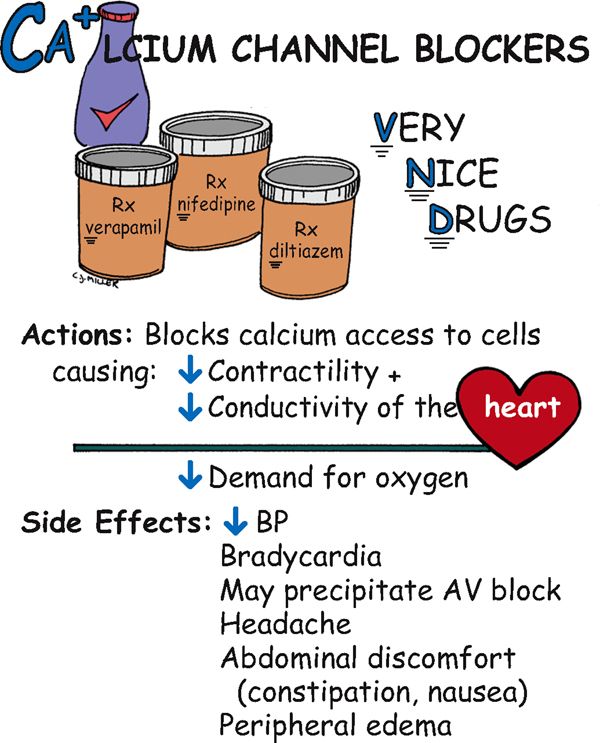
Calcium Channel Blockers

ACTION
Block calcium access to the cells, causing decreased heart contractility and conductivity and leading to a decreased demand for oxygen.
USES
• Angina, hypertension, and dysrhythmias (verapamil and diltiazem)
CONTRAINDICATIONS
• nifedipine: hypersensitivity
• verapamil: severe left ventricular dysfunction, decreased blood pressure, cardiogenic shock, or heart block
• diltiazem: sick sinus syndrome, heart block, decreased blood pressure, acute myocardial infarction, or pulmonary congestion
PRECAUTIONS
• Renal or hepatic insufficiency may develop.
• Avoid giving verapamil or diltiazem with beta blockers and digoxin.
SIDE EFFECTS
• Decreased blood pressure, **edema of the extremities,** headache
• Constipation (verapamil), nausea, skin flushing, †dysrhythmias†
NURSING IMPLICATIONS
1. Administer before meals; may be taken with food if needed; *do not crush or allow patient to chew sustained-release medication preparations.*
2. *Monitor vital signs and watch for low blood pressure.*
3. ‡Teach about postural hypotension.‡
4. Check liver and renal function studies.
5. *Weigh patient; report any peripheral edema or weight gain.*
6. ‡Teach patient to avoid grapefruit.‡
7. ‡Teach patient that constipation can be minimized by increasing dietary fiber and fluid.‡
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree