CASE 37
A 71-year-old male returned home after a 2-week stay in Mexico. The day after his return, he experienced an acute onset of fever, crampy abdominal pain, and watery diarrhea. By the next day, he had tenesmus and noticed mucus and a bloody tinge of the stool. The stools became grossly bloody and increased in number. Worried about his condition, his daughter took him to a hospital emergency department.
LABORATORY STUDIES
Diagnostic Work-Up
Table 37-1 lists the likely causes of illness (differential diagnosis). Leukocytes were present on fecal examination (Fig. 37-1). A diagnosis of dysentery was considered. Investigational approach may include
TABLE 37-1 Differential Diagnosis and Rationale for Inclusion (consideration)
Rationale: Multiple enteric pathogens can cause the dysentery syndrome. Classically, a rapid, descending course of infection, with fever and abdominal pain progressing to mucoid diarrhea with bloody stools (colitis), is seen with shigellosis, but similar symptoms may also be seen with the other agents listed under dysentery. E. coli O157:H7 is usually not associated with fever. Amebic colitis has a gradual onset, manifesting with a 1- to 2-week history of abdominal pain, diarrhea, and tenesmus (fever is uncommon). C. difficile with earlier antibiotic exposure is also important to consider. Noninfectious causes should be ruled out by laboratory investigation, although it is uncommon for inflammatory bowel disease to occur at the age of the case patient.
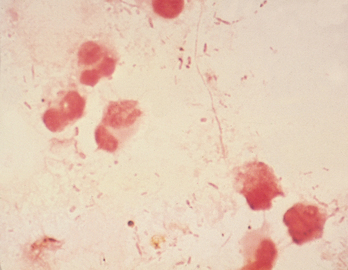
FIGURE 37-1 Leukocytes were seen on examination of fecal specimen from this patient. Gram stain.
(Courtesy of Dr. Paul Southern, Departments of Pathology and Medicine, University of Texas Southwestern Medical Center, Dallas, TX.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


