35 CASE 35
A 68-year-old man comes to the clinic complaining of difficulty in breathing.
PATHOPHYSIOLOGY OF KEY SYMPTOMS
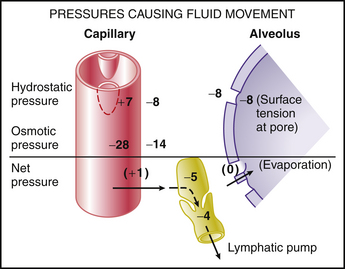
Fluid exchange across the pulmonary capillaries is governed by the same balance of hydrostatic pressures and protein-mediated oncotic pressure as occurs in other capillary beds. The relatively low pulmonary capillary pressure (normally 10 to 15 mm Hg) results in the net balance for fluid exchange across the pulmonary capillaries favoring reabsorption. Consequently, there is normally very little free fluid in the pulmonary interstitial space (Fig. 35-1).
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree