INTRODUCTION
Arterial disease can be broadly classified into two categories: occlusive and aneurysmal. The major sequelae of arterial obstruction are tissue ischemia and necrosis, while those of aneurysmal disease are rupture and hemorrhage in the aortic position and thrombosis and embolization in the peripheral arteries.
ARTERIAL OCCLUSIVE DISEASE
Although atherosclerosis is the dominant cause of arterial occlusive disease in Western countries, other etiologies such as congenital and anatomical anomalies, auto immune diseases, and remote thromboembolism can also result in arterial obstruction. Symptoms of occlusive vascular disease primarily are end-organ dysfunction and, in the muscle beds, pain with exercise and tissue necrosis.
Atherosclerosis can occur in any artery, with plaques most commonly developing in areas of low shear stress, such as at arterial branch points. Lesions are usually symmetrically distributed, although the rate of progression may vary. Early lesions are confined to the intima. In advanced lesions, both intima and media are involved, but the adventitia is spared. Preservation of the adventitia is essential for the vessel’s structural integrity and is the basis for all cardiovascular interventions.
When the hemodynamically significant disease affects a major artery, a parallel system of collateral vessels may preserve flow to the peripheral runoff bed. Collateral vessels are smaller, more circuitous, and always have a higher resistance than the original unobstructed artery. The stimuli for collateral development include abnormal pressure gradients across the collateral system and increased flow velocity through intramuscular channels that connect to reentry vessels. Adequate collateral vessels take time to develop but often maintain tissue viability in patients with chronic major arterial occlusions.
Generally, arterial insufficiency occurs in medium-sized and large arteries with at least a 50% reduction in arterial diameter. This correlates with a 75% narrowing of cross-sectional area and enough resistance to decrease downstream flow and pressure. Early in the process, compensatory dilation of the vessel wall may preserve lumen diameter as the atherosclerotic lesion develops, but with continued growth, lesions overcome this adaptation and result in flow limiting stenoses. If there is adequate collateral flow, single stenoses or even occlusions are reasonably well-tolerated. Severe ischemia occurs when there are inadequate collaterals or there are multiple levels of disease.
CHRONIC LOWER EXTREMITY OCCLUSIVE DISEASE
Peripheral arterial insufficiency is predominantly a disease of the lower extremities. Upper extremity arterial lesions are uncommon and confined mostly to the subclavian arteries. Even when present, upper extremity atherosclerosis rarely produces symptoms due to abundant collateral pathways. In the lower extremities, however, obstructive lesions are distributed widely, with lesions of the superficial femoral and iliac arteries the most common (Figure 34–1). Symptoms are related to the location and number of obstructions.
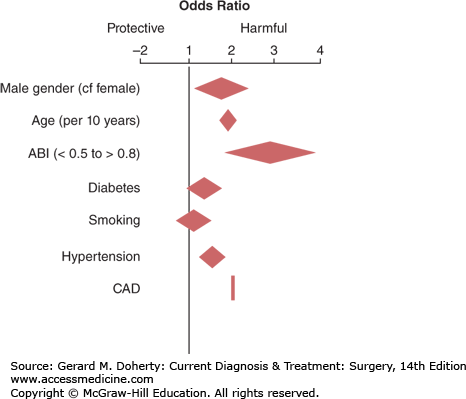
Peripheral arterial disease affects at least 20% of individuals older than 70 years with the incidence increasing with the increasing incidence of diabetes. Although most patients with this disorder do not develop gangrene or require amputations, adverse outcomes of systemic atherosclerosis, including myocardial infarction and/or stroke, are common. Even after adjustment for known risk factors, individuals with peripheral arterial disease exhibit a several-fold higher risk of mortality than the nonaffected population. A low ankle-brachial index (ABI) is one of the strongest risk factors for all-cause mortality. Peripheral arterial disease is more a marker of a more virulent form of atherosclerosis and early death from cardiovascular or cerebrovascular disease than an indicator of imminent limb loss; thus, identifying and treating associated atherosclerotic risk factors is essential (Figure 34–2).
Figure 34–2.
Odds ratios for risk factors for all-cause mortality. ABI, ankle-brachial index; CAD, coronary artery disease. (Reproduced, with permission, from TASC Working Group: Dormandy JA et al. Management of peripheral arterial disease: epidemiology, natural history, risk factors. J Vasc Surg. 2000 Jan;31[1 Pt 2]:S1-S296.)
Intermittent claudication refers to pain in muscles of the lower extremity associated with walking and relieved by rest. Because tissue perfusion is adequate at rest, tissue loss is not present and the risk of amputation is low unless there is progression of disease. Claudication is derived from the Latin word meaning “to limp”; therefore, the term should be used only for symptoms in the lower extremities. The pain is a deep-seated ache usually in the calf muscle, which gradually progresses until the patient is compelled to stop walking. Patients occasionally describe “cramping” or “tiredness” in the muscle. Typically, symptoms are completely relieved after 2–5 minutes of inactivity. Claudication is distinguished from other types of pain in the extremities in that it does not occur at rest and some period of exertion is always required before it appears, it generally occurs after a relatively consistent distance traveled, and it is relieved by cessation of walking. Relief of symptoms is not dependent upon sitting or other positional change. The severity of claudication is traditionally expressed in terms of city blocks.
Regardless of which arterial segment is involved, claudication most commonly involves the calf muscles because of their high workload with the mechanics of normal walking. Occlusions proximal to the origin of the profunda femoris can extend the pain to involve the thigh. Gluteal pain indicates lesions in or proximal to the hypogastric arteries and is often accompanied by impotence. Leriche syndrome occurs in men with aortoiliac disease and includes claudication of calf, thigh, and buttock muscles; erectile dysfunction; and diminished or absent femoral pulses. Occasionally, patients describe transient numbness of the extremity accompanying the pain and fatigue of claudication as nerves as well as muscles become ischemic.
The two conditions that most often mimic claudication are osteoarthritis of the hip or knee and neurospinal compression due to congenital or osteophytic narrowing of the lumbar neurospinal canal (spinal stenosis). Osteoarthritis can be differentiated from claudication because pain occurs predominantly in joints, the amount of exercise required to elicit symptoms varies, symptoms are characteristically worse in the morning and upon initiating exercise, rest does not relieve symptoms promptly, the severity of symptoms changes from day to day, and anti-inflammatory agents may relieve the pain. Impingement on the spinal canal or nerve root produces neurospinal compression symptoms; therefore, the pain is typically burning in nature and symptoms may occur with sitting or standing. Neurospinal pain often follows a dermatomal distribution, a key factor in differentiating this from claudication.
Uncommon conditions such as coarctation of the aorta, chronic compartment syndrome, popliteal artery entrapment, and vasculitis can mimic symptoms of atherosclerotic arterial insufficiency. Age at presentation and associated findings may aid in diagnosing these conditions.
The correct diagnosis of vascular claudication should be easily established by determining the location of pain with exercise (calf), the quality of the pain (aching or cramping), the length of time required for relief of symptoms after stopping exercise (immediate), the reproducibility of the distance walked before symptoms begin (initial claudication distance), and most importantly, the reduction or loss of pulses with exercise.
With extensive disease, patients develop ischemic rest pain and/or ulceration. Ischemic rest pain, a grave symptom caused by ischemic neuritis, indicates advanced arterial insufficiency that carries a risk of gangrene and amputation if arterial reconstruction cannot be performed. The pain is severe and burning, usually confined to the forefoot distal to the metatarsals. It may be localized to the vicinity of an ischemic ulcer or pregangrenous toe. It is aggravated by elevation of the extremity or by bringing the leg to the horizontal position. Thus, it appears at bed rest (hence the name) and may prevent sleep. Because gravity aids the delivery of arterial blood, classically, the patient with rest pain can obtain relief by simply hanging the leg over the side of the bed. This simple maneuver will differentiate ischemic rest pain from peripheral neuropathy, which is associated with diabetes and is the most common cause of foot pain at rest. In patients who must keep the foot constantly dependent to relieve pain, the leg and foot may be swollen, causing some confusion in diagnosis. The ischemic neuritis of rest pain is severe and resistant to opioids for relief.
Patients with rest pain may give a history of claudication, but rest pain also may occur de novo in diabetics with distal tibial disease, embolic occlusion of the distal tibial arteries, and patients whose walking is limited by other conditions. Differentiating ischemic rest pain from neuropathy in diabetics is critical and may require vascular testing to clarify the diagnosis.
Patients with severe lower extremity arterial insufficiency often develop ulcers or wounds on the feet even from seemingly trivial trauma. These lesions are most commonly located on the distal foot and toes, but on occasion they can be in the upper foot or ankle. Typically, the wounds are excruciatingly painful, deep, and devoid of any evidence of healing such as contraction or formation of granulation tissue.
Inability to attain or maintain an erection may be produced by lesions that obstruct blood flow through both hypogastric arteries and is commonly found in association with narrowing of the terminal aorta, common iliac, or hypogastric arteries. Vasculogenic erectile dysfunction is less common than that due to other causes.
Although the patient may report numbness in the extremity, sensory abnormalities are generally absent on examination. If decreased sensation is found in the foot, peripheral neuropathy should be suspected.
Physical examination is of paramount importance in assessing the presence and severity of vascular disease. The physical findings of peripheral atherosclerosis are related to changes in the peripheral arteries and to tissue ischemia.
Decreased amplitude of the pulse denotes proximal obstructions to flow. The pulse examination can help localize disease. For example, an absent femoral pulse usually signifies aortoiliac disease. It is unusual for collateral flow to be sufficient to produce a pulse distal to an occluded artery.
A bruit is the sound produced by dissipation of energy as blood flows through a stenotic arterial segment. With extremely high flows, the energy may vibrate the artery, creating a “thrill.” The bruit or thrill is transmitted distally along the course of the artery. Thus, when a bruit is heard through a stethoscope placed over a peripheral artery, stenosis is present at or proximal to that level. The pitch of the bruit rises as the stenosis becomes more marked, until a critical stenosis is reached or the vessel becomes occluded, when the bruit may disappear. Thus, absence of a bruit does not indicate insignificant disease.
Exercise in a normal individual increases the pulse rate without producing arterial bruits or reduction in pulse amplitude. In an individual who complains of claudication, there may be minimal findings at rest, but exercise will produce decreased pulse strength, decreased distal arterial pressure, and possibly an audible bruit unmasking a significant stenosis. Exercise is best used in conjunction with noninvasive vascular testing.
Chronic ischemia commonly produces loss of hair over the dorsum of the toes and foot and may be associated with thickening of the toenails (onychomycosis) due to slowed keratin turnover. With more advanced ischemia, there is atrophy of the skin and subcutaneous tissue so that the foot becomes shiny, scaly, and skeletonized.
Pallor of the foot on elevation of the extremity to approximately 40 cm with a complete absence of capillary refill indicates advanced ischemia. Pallor on elevation does not occur unless advanced ischemia is present. It is always present with ischemic rest pain.
When pallor is produced with elevation, the ischemia results in maximum cutaneous vasodilation. When the extremity is returned to a dependent position, blood returning to the dilated vascular bed produces an intense red or possibly ruborous color in the foot, called reactive hyperemia, and denotes advanced disease. The delay in the appearance of color when the extremities return to a dependent position is proportionate to the impairment in circulation.
In advanced atherosclerotic disease, the skin of the foot displays a characteristic dark red/cyanotic color on dependency. Because of low inflow, the blood in the capillary network of the foot is relatively stagnant, oxygen extraction is high, and the capillary blood becomes the color of the venous blood. The concurrent vasodilation due to ischemia causes blood to suffuse the cutaneous plexus, imparting a purple color to the skin. The purple discoloration due to severe chronic venous insufficiency does not give way to pallor on elevation.
With chronic ischemia, the temperature of the skin of the foot decreases. Coolness can best be detected by palpation with the back of the examiner’s hand with comparison to the contralateral foot.
Ischemic ulcers are usually very painful and accompanied by rest pain in the foot. They occur in toes or at a site where minor trauma can initiate the injury. The margin of the ulcer is sharply demarcated or punched-out, and the base is devoid of healthy granulation tissue. The surrounding skin is pale and mottled, and signs of chronic ischemia are invariably present.
Moderate to severe degrees of chronic ischemia produce gradual soft tissue and muscle atrophy and loss of strength. Joint mobility and gait may be altered due to muscle atrophy. Subsequent changes in foot structure and gait increase the possibility of developing foot ulceration.
Severe tissue ischemia may progress to necrosis with minor injuries, infection, or swelling. Necrosis halts proximally at a line where the blood supply is sufficient to maintain viability and results in dry gangrene. If the necrotic portion is infected (wet gangrene), necrosis may extend into tissues that would normally remain viable.
Noninvasive assessment is helpful to determine the severity of hypoperfusion and the sites of hemodynamically significant stenoses or occlusions.
The ankle-brachial index is a quick screening test and the cornerstone of the diagnosis of peripheral vascular disease. The ABI is determined by dividing the systolic pressure obtained by Doppler insonation at the ankle by the brachial arterial pressure. Normally, the ABI is 1.0 or greater; a value below 1.0 indicates occlusive disease proximal to the point of measurement. The ABI correlates roughly with the degree of ischemia (eg, claudication occurs with a value less than 0.7 and rest pain usually appears when the ratio is 0.3 or lower). Elderly patients or patients with diabetic vascular disease may have artificially elevated ABI values due to calcified, noncompressible arteries, and toe-to-brachial pressure ratios should be substituted.
Blood pressures can be measured at rest and after exercise in the ankle, and the effect of exercise can be monitored. Exercise testing confirms and quantitates the diagnosis of claudication. To perform exercise testing, the patient walks on a treadmill at a standard speed and grade until claudication pain is experienced or a time limit is reached. With significant arterial occlusive disease, there will be a decrease in the ABI with exercise, usually measured 1 minute after cessation of walking. If the pain is not due to arterial stenosis, no fall in pressure will occur. This test is particularly useful in differentiating neurogenic pain with walking from claudication.
Color duplex ultrasound imaging is a mainstay of vascular imaging. It is a painless, relatively inexpensive, and (in experienced hands) accurate method for acquiring anatomic and functional information (eg, velocity gradients across stenoses). Although the accuracy of this study is operator dependent, it can supply sufficient information to permit intervention in selected cases.
CT angiography (CTA) is useful for imaging the arterial tree and has the advantage of visualizing cross-sections of the vessel lumen. In many instances, this allows for more accurate determination of vessel diameter and stenosis severity than conventional angiography. It does require the administration of nephrotoxic contrast dye, it is less useful for tibial disease, and its images may be obscured by the presence of calcification or metallic implants. MR angiography (MRA) also can be used to obtain images similar in quality to angiography in most cases. MRA does not show calcifications and gives better visualization of tibial vessels than CTA. MRA also can reveal details of composition of atherosclerotic plaque. Gadolinium-associated nephrogenic fibrosing dermopathy limits its use in patients with renal insufficiency. The integrated use of computer workstations with CT and MR image data can provide three-dimensional (3D) images that can be useful in visualizing patient anatomy and planning interventional procedures.
Conventional arteriography provides detailed anatomic information about peripheral arterial disease. It is reserved for patients warranting invasive intervention such as percutaneous transluminal angioplasty (often shortened to PTA) or vascular surgery. Complications of angiography are related to technique and contrast media. Technical complications such as puncture site hematomas, arteriovenous fistulas, and false aneurysms are rare (1%). Contrast agents may precipitate allergic reactions (0.1%). Patients with renal failure, proteinuria, diabetes, and dehydration are at increased risk for contrast-induced renal failure. Adequate hydration of patients before and after angiography, acetylcysteine, and periprocedural infusions of sodium bicarbonate infusions may reduce the incidence of this complication.
The objectives of treatment for lower extremity occlusive disease are relief of symptoms, prevention of limb loss, and maintenance of bipedal gait.
In general, patients with peripheral vascular disease have shortened life expectancies because of their severe atherosclerotic disease. Nondiabetic patients with ischemic disease of the lower extremity have a 5-year survival rate of 70%. The survival rate is 60% in patients with associated ischemic heart disease or cerebrovascular insufficiency. Patients with peripheral vascular disease and renal failure have a 2-year survival rate of less than 50%. Most deaths are due to myocardial infarctions and strokes. Only 20% of deaths are due to nonatherosclerotic causes.
Nonoperative treatment consists of (1) medical management of cardiovascular risk factors, (2) exercise rehabilitation, (3) foot care, and (4) pharmacotherapy.
See Table 34–1. Cigarette smoking is the single most important risk factor for peripheral vascular disease, and all patients should stop smoking. At high levels of consumption, 2-3 packs per day, claudicants will experience immediate improvement in walking distance.
In the past, elevated lipids were not usually associated with peripheral vascular disease. Hyperlipidemia, however, is often present, especially in patients with early onset of disease. Elevated triglyceride levels and low high-density lipoprotein (HDL) cholesterol levels are more prevalent than elevated levels of low-density lipoprotein (LDL) cholesterol. Reduction of elevated lipid levels is associated with stabilization or regression of arterial plaques. Statins are extremely effective in reducing LDL cholesterol, and goals of therapy for patients with peripheral vascular disease are to maintain cholesterol levels at less than 100 mg/dL (2.6 mmol/L). Statins have other pleiotropic effects that may reduce inflammation, stabilize plaques, and independently increase walking distance in claudicants. Other antihyperlipidemic medications, including niacin and fibrates (gemfibrozil), may be used to lower hypertriglyceridemia, which can increase HDL cholesterol.
Both type 1 and type 2 diabetes increase the prevalence and severity of cardiovascular disease. Intensive glycemic control reduces the incidence of nephropathy, neuropathy, and retinopathy in diabetes, but it does not correlate with the severity or progression of peripheral arterial disease. In order to reduce all-cause mortality, however, it is recommended that fasting blood sugars should be controlled with hemoglobin A1c levels less than 7%.
For claudicants, exercise ranging from unsupervised walking to formal supervised exercise on a treadmill significantly improves walking ability. A 21-study meta-analysis of exercise programs showed an average 180% increase in initial claudication distance and a 120% increase in maximal walking distance achieved through exercise. The precise mechanism behind this improvement is not firmly established. Collateral development seems unlikely because ankle pressures and limb flow do not increase substantially. Possible explanations include improved metabolic capacity and conditioning of the muscles.
Since patients with claudication are at a twofold to fourfold greater risk of dying from complications of generalized atherosclerosis than people without claudication, an additional benefit of exercise in these patients is that an improvement in walking distance as part of an aggressive risk factor modification regimen results in an overall decrease in cardiovascular risk.
The feet of patients with neuropathy or with critical limb ischemia should be inspected and washed daily and kept dry. Mechanical and thermal trauma to the feet should be avoided. Toenails should be trimmed carefully, and corns and calluses should be attended to promptly. Even minor foot infections or injuries should be treated aggressively. Educating the patient to understand neuropathy, peripheral vascular insufficiency, and the importance of foot care is a central aspect of treatment.
The Antiplatelet Trialists Collaboration found an overall 25% decrease in fatal and nonfatal myocardial infarctions, strokes, and vascular deaths in those treated with antiplatelet agents. Aspirin at dosages ranging from 75 to 350 mg/d is the first-line antiplatelet agent recommended, though clopidogrel, which blocks the activation of platelets by adenosine diphosphate (ADP), may be useful in aspirin-intolerant patients. Clopidogrel is also an important adjunctive therapy in reducing thrombogenicity at locations of endovascular arterial treatment. All patients with cardiovascular disease, whether symptomatic or asymptomatic, should be considered for antiplatelet therapy to reduce the risk of cardiovascular morbidity and mortality.
Two drugs have been approved by the FDA for treatment of intermittent claudication. Pentoxifylline produces a small improvement in both initial claudication distance (about 20%) and absolute claudication distance (about 10%). Cilostazol is a phosphodiesterase III inhibitor with vasodilator, antiplatelet, and antilipid activity. Randomized, placebo-controlled, blinded trials have shown an increase of about 50% in absolute claudication distance in patients treated with cilostazol. Quality-of-life assessments also improved significantly. Gene therapy for cardiovascular disease is being investigated, but conclusions regarding safety and efficacy are premature.
| Risk Factor | Therapy | Clinical Effect |
|---|---|---|
| Tobacco use | Counseling Pharmacotherapy Nicotine replacement Bupropion, varenicline | Reduced overall mortality Reduced cardiovascular events |
| Antiplatelet | Aspirin Clopidogrel (Plavix) | Antiplatelet therapy gives > 20% reduction in Ml, stroke, or vascular death |
| Hyperlipidemia | Statin Lipid goals in PAD patients: LDL < 100 mg/dL | 20-30% reduction in cardiovascular and all-cause mortality in CAD patients |
| Hypertension | Target BP < 140/90 in PAD patients Beta-blocker ACE inhibitor | Beta-blocker and ACE inhibitors each associated with > 20% reduction in cardiovascular mortality |
| Diabetes | Goal hemoglobin Alc < 7% | Benefits in vascular disease unproven |
| Lifestyle | Daily aerobic exercise Weight loss Healthy, low-fat diet | Reduced lipid levels Reduced cardiovascular events |
Interventional procedures, open or endovascular, are performed both for limb salvage and for incapacitating claudication. The choice of operative procedure depends on the location and distribution of arterial lesions and the patient’s comorbidities. Recognition of coexistent cardiopulmonary disease is particularly relevant, because many patients with peripheral vascular disease also have ischemic heart disease and/or chronic lung disease associated with tobacco use. Preoperative cardiac functional assessment is sometimes necessary, but preoperative myocardial revascularization is not beneficial in patients with reasonable cardiac reserve. All patients undergoing vascular surgery should have preoperative risk assessment. Randomized trials have shown that perioperative β-blocker, angiotensin-converting enzyme (ACE) inhibitor, and statins may reduce cardiac morbidity in patients undergoing vascular surgery. Evidence is also emerging demonstrating the importance of maintaining statin therapy throughout the perioperative period.
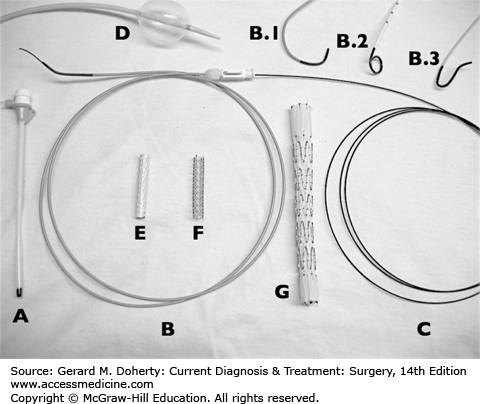
Endovascular therapy consists of image-guided techniques to treat diseased arterial segments from within the lumen of the vessel. Access to the arterial system is established by the insertion of valved sheaths, usually percutaneously, into the access vessel, often the common femoral artery. Steerable wires and catheters are then passed through the vasculature under fluoroscopic guidance to the target lesion (Figure 34–3). Once the target lesion is accessed, therapeutic maneuvers, such as angioplasty, or devices, such as stents, can be delivered. In many arterial beds, endovascular therapy is more commonly utilized than open surgical therapy because of its minimally invasive nature and reduction of short-term morbidity and mortality. However, many questions remain concerning the long-term durability of endovascular repairs, and open surgery still plays a major role in the treatment of patients with arterial disease.
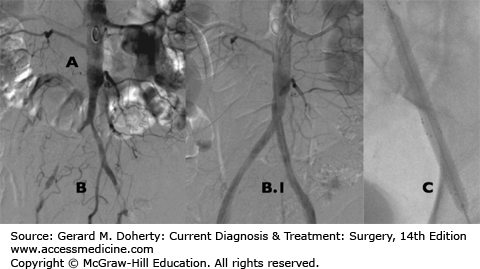
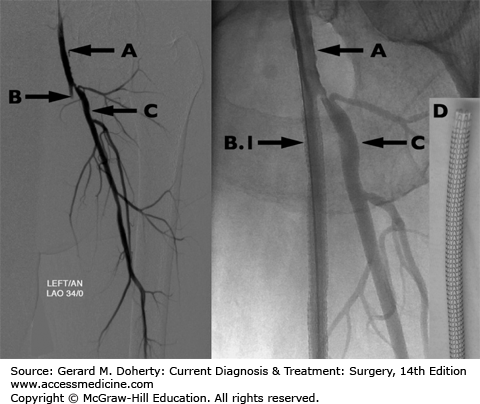
with or without placement of an intravascular stent, is often the treatment of choice when stenoses or even occlusions are relatively short and localized. As the angioplasty balloon expands, it stretches the adventitia, fracturing and compressing plaque, expanding the artery to widen the lumen. Energy losses associated with a stenosis are inversely proportionate to the fourth power of the radius; therefore, even small increases in radius can result in substantial increases in blood flow, although durability of the procedure is improved with the reestablishment of a normal lumen. Concomitant stenting is frequently performed to improve luminal expansion and the arteriographic appearance of the lesion. Stent grafts (stents with fabric covering) may also be used in selected cases or to repair the inadvertent rupture of an artery during angioplasty (Figure 34–4).
Both stents and stent grafts are commonly used from the aortic bifurcation to the distal popliteal artery. Stenting is performed less commonly below the knee, but angioplasty of tibial disease is now common with the use of small catheters and wires. As in the coronaries, drug eluting stents may significantly improve patency rates. Percutaneous mechanical and laser atherectomy are other options in removing obstructing lesions in lower extremity atherosclerotic occlusive disease.
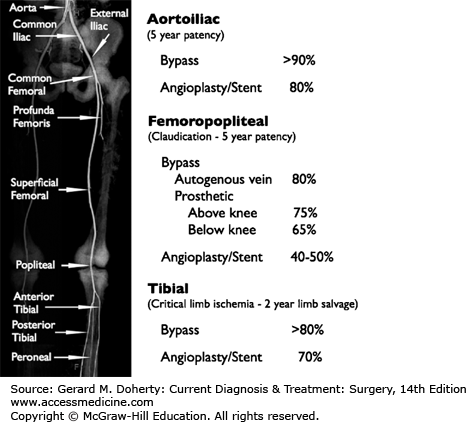
For short, stenotic segments in larger, more proximal vessels, the results of endovascular therapies are good with 1-year success rates of 85% in common iliac disease and 70% in external iliac disease. The results with superficial femoral and popliteal lesions are lower (Figure 34–5). The success of endovascular therapy for lower extremity occlusive disease is inversely related to the complexity of the lesion, defined by the number and length of stenoses treated.
Close follow-up of patients post endovascular therapy is required since disease may recur more frequently after angioplasty than after bypass surgery. The patient should be closely followed using noninvasive tests. Repeat angioplasty or stenting may be indicated for recurrent disease, but the improvement in morbidity and mortality of endovascular interventions may be offset by the need for multiple repeat procedures. In general, minimally invasive percutaneous treatment of lower extremity occlusive disease is best used in patients of high operative risk and severe, limb-threatening ischemia (Figure 34–6).
Figure 34–3.
Endovascular gear. A: Sheath. Inserted using Seldinger technique into access vessel. Wires, catheters, and devices pass through the sheath. Sheaths provide stable working access points and protect artery. B: Catheter. Variable length, stiffness, coating, and shape (examples: B.1, cobra; B.2, pigtail; B.3, mesenteric selective). Catheters help steer wires through vasculature and also maintain access in vessel. C: Guidewire. Variable diameter, length, stiffness, and shape. Used to gain access into vasculature, cross lesions, and deliver devices. D: Balloon catheter. E: Peripheral stent graft. F: Peripheral nitinol self-expanding stent. G: Aortoiliac stainless steel/Dacron stent-graft.
Open operations are indicated for aortoiliac occlusive disease in younger patients with low operative risk or patients with severe disease not amenable to endovascular therapy. To completely bypass the aortoiliac segment, an inverted Y-shaped prosthesis is interposed between the infrarenal abdominal aorta and the femoral arteries, creating an aortofemoral bypass. The goal of operation is restoration of blood flow to the common femoral artery or, when occlusive disease of the superficial femoral artery is present, to the profunda femoris artery. The clinical results of aortofemoral reconstruction are excellent, although the mortality and morbidity clearly are higher than for endovascular therapy. The operative death rate is 5%; early patency rate, 95%; and late patency rate (5-10 years postoperatively), about 80%. Late complications may be as high as 10% and include graft-intestinal fistula formation, anastomotic aneurysm formation, renal failure, and erectile dysfunction.
Lower risk procedures may be preferable in high-risk patients. If the clinically important lesions are confined to one side, a femoral-femoral or iliofemoral bypass graft can be used. A graft from the axillary to the femoral artery (ie, axillofemoral graft) can be used for bilateral disease. Unfortunately, these “extra-anatomic” methods of arterial reconstruction are more prone to late occlusion than are direct reconstructions.
When disease is confined to the femoropopliteal segment of the SFA, femoropopliteal bypass is used. The principal indication for these operations is limb salvage. In patients with claudication alone, the indications for femoropopliteal bypass are more difficult to define but must include substantial disability from claudication. For limited lesions of the superficial femoral artery, endovascular therapy is often attempted first, with surgery reserved for extensive disease or angioplasty failure.
The best conduit for femoropopliteal bypass is an autologous greater saphenous vein. The saphenous vein may be left in situ or removed and reversed. Expanded polytetrafluoroethylene (PTFE) may also be used as a conduit, particularly for bypass to the suprageniculate popliteal artery. Below the knee, PTFE conduits produce much lower patency rates than saphenous veins. Operative death rates are low (2%), and 5-year patency rates range from 60% to 80%. Limb salvage rates are higher than graft patency rates.
The profunda femoris artery perfuses the thigh and acts as an important source of collateral flow when the superficial femoral artery is diseased. When there is a stenosis of the profunda, profundoplasty alone can be performed for limb salvages with success rates of 80% when the suprageniculate popliteal artery is patent and 40%–50% when the popliteal artery is occluded. Isolated profundoplasty is rarely helpful for treating claudication.
Reconstruction of tibial arteries (ie, distal bypass to the tibial, peroneal, or pedal vessels) is performed only for limb salvage. Advancing technology allows better endovascular therapy in the tibial vessels, with decreased short-term morbidity and mortality, and similar gains in limb salvage when compared to bypass surgery. However, bypass still remains an important mode of therapy for these patients. Autogenous saphenous veins are preferred because prosthetic conduits have high failure rates. Due to smaller vessel size, extensive disease, and probably the length of the bypass conduit, these grafts are not as durable as femoropopliteal bypass, so the limb salvage rate is substantially higher than graft patency. The operative death rate for these procedures is about 5 due to extensive comorbidities.
Amputation of the limb is necessary within 5-10 years in only 5% of patients presenting with claudication. Amputation is more common if patients continue to smoke cigarettes. Patients with multiple risk factors for atherosclerosis and short-distance claudication are also at increased risk for eventual limb loss. Of patients who present with ischemic rest pain or ulceration, 5%–10% require amputation as initial therapy, and most eventually will require amputation if not revascularized. Successful revascularization results in lower costs than primary amputation and an infinite improvement in quality of life. Occasionally, primary amputation may be preferable to revascularization if the likelihood of successful bypass is low, extensive foot infection is present, or the patient is nonambulatory. Amputation levels, options, and the special needs of amputees are covered in the section on Lower Extremity Amputation.
ACUTE LOWER EXTREMITY OCCLUSIVE DISEASE
Sudden occlusion of a previously patent artery is a dramatic event characterized by the abrupt onset of severe pain and absent pulses in the involved extremity. Tissue viability depends on the extent to which flow is maintained by collateral circuits. When ischemia persists, motor and sensory paralysis and muscle infarction become irreversible in a matter of hours.
Acute major arterial occlusion may be caused by an embolus, primary arterial thrombosis, trauma, or dissection. The heart is the source of embolus in 80%–90% of episodes, with the remainder from proximal arterial lesions. Aortic aneurysms often contain thrombus, but this material rarely causes symptomatic emboli. In contrast, femoral and particularly popliteal aneurysms embolize frequently. Ulceration in atherosclerotic plaques also can lead to formation of thrombus, which may fragment. Miscellaneous infrequent sources of emboli include cardiac tumors (including cardiac myxoma) and paradoxical emboli (venous thrombi migrating through a patent foramen ovale). Up to 5%–10% of spontaneous emboli originate from a source that remains unidentified despite thorough diagnostic interrogation.
It may be difficult to differentiate between sudden thrombosis of an atherosclerotic peripheral artery and embolic occlusion. The former patients usually have preexisting atherosclerotic stenosis and low blood flow, which predisposes to stagnation and thrombosis. One should also keep in mind the clinical setting and a history of preexisting symptoms such as atrial fibrillation (embolus) or claudication (primary thrombosis).
The Five Ps
Pain
Pallor
Pulselessness
Paresthesias
Paralysis
Acute arterial occlusion is characterized by the five Ps: pain, pallor, pulselessness, paresthesias, and paralysis. Severe sudden pain is present in 80% of patients, and its onset usually indicates the time of vessel occlusion. Pain is absent in some patients because of prompt onset of anesthesia and paralysis and portends a poor prognosis.
On examination, the key finding is a lack of palpable pulses in a diffusely painful extremity. It is important to determine if sensitivity to light touch is maintained. These fibers are highly susceptible to ischemia, and their dysfunction heralds the beginning of irreversible ischemic changes. The onset of motor paralysis implies impending gangrene. Early intervention is critical. Swelling with acute tenderness of a muscle belly—usually in the calf following acute femoral artery occlusion—generally denotes irreversible muscle infarction. Skin and subcutaneous tissues have greater resistance to hypoxia than nerves and muscles, which may demonstrate irreversible histological changes after 3 hours or less of ischemia.
Immediate anticoagulation by intravenous heparin slows the propagation of thrombus and allows time for assessment of adequacy of collateral flow and preparation for operation. If light touch is intact, arteriography may be performed to define the anatomy and assist in planning the operation. Diagnosis of acute embolic occlusion is based on an abrupt block of the artery with little accompanying arterial disease; conversely, acute in situ thrombosis is associated with extensive atherosclerosis and a well-established collateral network. The operative treatment for an embolus, embolectomy, differs from that of preexisting atherosclerosis, which may require bypass. Nonoperative management is rarely indicated except in debilitated patients and patients with emboli to major arteries in the upper extremities, which generally have good collateral circulation.
Therapeutic options include catheter-directed thrombolysis, percutaneous mechanical thrombectomy, and surgical embolectomy. For patients with severe acute ischemia, operative therapy is preferable because it is usually associated with the least delay in reestablishing perfusion. Surgical embolectomy may be performed through an arteriotomy at the site of the embolic occlusion or, most commonly, by clot extraction with a balloon (Fogarty) catheter inserted through a remote arteriotomy. Successful embolectomy requires removal of the embolus and the “tail” of thrombus that extends distally or proximally from it. If operation is not performed within the first few hours, the clot may become adherent, and subsequent revascularization is less successful. Intraoperative infusion of thrombolytic agents is often a useful adjunct to embolectomy.
In patients who will tolerate a delay in revascularization (ie, those who do not have neural changes on examination), intra-arterial thrombolysis should be considered. The usual regimen involves selective intra-arterial infusion of low doses of thrombolytic agent (eg, tissue plasminogen activator) directly into the clot. This activates thrombus plasminogen more efficiently, allows high concentrations in the clot while limiting systemic effect, and has acceptable complication rates. In cases of thrombosis on preexisting atherosclerotic lesions, thrombolysis reveals the underlying lesions that will require treatment to prevent recurrent thrombosis.
If revascularization is successful, a reperfusion injury may develop with significant swelling requiring fasciotomy to treat the compartment syndrome that may accompany the reperfusion injury. Renal insufficiency from myoglobin release should be anticipated after reperfusion of ischemic muscle. Treatment consists of vigorous hydration and alkalinization of the urine. Administration of free radical scavengers such as Mannitol may be helpful in this disorder.
Patients with clearly irreversible limb ischemia should undergo amputation without an attempt at revascularization, as revascularization may expose the patient to the serious hazards of reperfusion caused by release of acidic and hyperkalemic venous blood from the dying extremity.
Traumatic arterial occlusion must be corrected within a few hours to avoid development of gangrene. Repair of arterial injury is usually performed in conjunction with repair of other injuries. Occasionally, temporary shunts are used to restore flow to the injured extremity while other injuries are addressed and repaired.
PERIPHERAL MICROEMBOLI
Microemboli are most dramatic when they occlude a digital artery perfusing a toe or finger. This causes sudden pain, cyanosis, and coldness or numbness in the affected digit. These changes characteristically improve over several days. If there are multiple emboli, these symptoms may reappear in a different area of the hand or foot. In the lower extremity, this clinical entity has been called blue toe syndrome or trash foot. The sudden onset of pain and purple discoloration of a toe in the presence of palpable pulses is recognized as a potentially limb-threatening arterial problem. With each succeeding episode, recovery is slower and less complete.
The most common source of microembolization is cardiac valvular disease. However, if no cardiac valvular lesions are found, a careful examination of the proximal arterial tree must be done to identify an arterial source shedding atheroemboli.
Sudden onset may differentiate peripheral microembolism from other causes of blue toes, such as vasculitis, thromboangiitis obliterans, trauma, or chronic ischemia. If a single toe is affected, it is more likely to be the result of emboli, while multiple cyanotic toes are more likely to be vasculitis or chronic ischemia. It is important to remember that a patent proximal artery is required to serve as a conduit for the embolus, so pulses are intact. Furthermore, a normal blood supply is present in adjacent tissue segments. The appearance of a normally perfused foot with a cyanotic toe is characteristic. However, the waxing and waning symptoms of repeated emboli can make the diagnosis difficult. Unless the syndrome is recognized, alternative diagnoses investigated, and the lesion of origin corrected, survival of the foot or hand may be in peril.
DIABETIC VASCULAR DISEASE
Atherosclerotic arterial disease in patients with diabetes mellitus is more diffuse and more severe than in nondiabetics. In diabetic patients, the tibioperoneal vessels frequently contain atherosclerotic changes, and the vessels are often heavily calcified. The degree of ischemia may be severe and extensive, and noninvasive tests (ABIs) may be falsely elevated. Fortunately, in many diabetics, the small arteries in the foot are relatively spared, making distal bypass to these arteries possible and allowing foot salvage in cases of threatened limb loss.
Diabetic patients also have a high incidence of neuropathy and are more apt to ignore minor foot injuries, which can develop into ulcerations. Daily foot inspections are essential to avoid progression of minor injuries into limb threatening lesions. Neuropathy is also responsible for loss of tone of intrinsic foot muscles that leads to subluxation of the metatarsal phalangeal joints, resulting in a “rocker-bottom” foot and ultimately producing complete joint destruction termed a Charcot foot. These architectural changes also make skin breakdown more likely to occur and require referral to a foot and ankle clinic.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree