CASE 33
LABORATORY STUDIES
Diagnostic Work-Up
Table 33-1 lists the likely causes of the man’s illness (differential diagnosis). A clinical diagnosis of acute human immunodeficiency virus (HIV)-1 infection was considered based on the risk and symptoms. Laboratory-based studies are necessary for confirmation of HIV-1 infection and may include
TABLE 33-1 Differential Diagnosis and Rationale for Inclusion (consideration)
Rationale: Several primary viral infections have similar presentations. Fever, malaise, and lymphadenopathy are common symptoms. CMV is frequently associated with liver involvement. A maculopapular truncal rash can often be seen in primary HIV infection. Oral ulcers are commonly seen with primary HSV infection. Infectious mononucleosis may have associated splenomegaly and, in particular, a severe sore throat. Secondary syphilis is often characterized by a rash that also involves the palms and soles. As seen above, symptoms, signs, and epidemiology (e.g., host risk factors) are helpful in suggesting an infectious etiology, but laboratory investigation is needed for confirmation of the clinical diagnosis.
MICROBIOLOGIC PROPERTIES
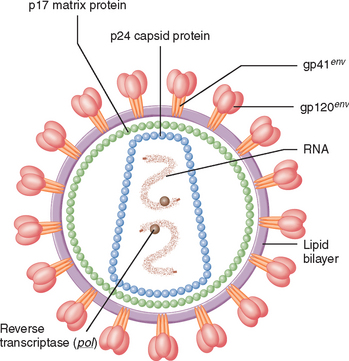
HIV belongs to a subgroup of retroviruses known as lentiviruses (“slow” viruses). The four recognized human retroviruses belong to two distinct groups: the human T lymphotropic viruses, HTLV-1 and HTLV-2, which are transforming retroviruses; and the human immunodeficiency viruses, HIV-1 and HIV-2, which are cytopathic viruses. The course of infection with retroviruses is characterized by a long interval between initial infection and the onset of clinical symptoms. The most common cause of HIV disease in the United States as well as worldwide is HIV-1. The virion structure of HIV-1 consists of a capsid and a surrounding matrix and envelope studded with virus-specific proteins (Fig. 33-1). Embedded in the viral envelope is a transmembrane protein (Env), consisting of a cap made of three molecules called glycoprotein (gp) 120, and a stem of three gp41 molecules that anchor the structure in the viral envelope. The envelope also incorporates a variety of host proteins, including major histocompatibility complex (MHC) class I and II antigens.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree