CASE 3
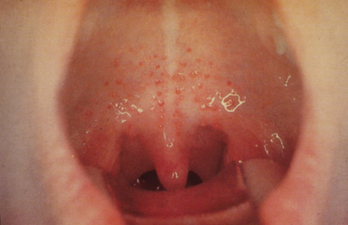
A 6-year-old girl came home from school feeling miserable on a cold day in January. She had a high fever and complained of an itchy throat. She had difficulty swallowing any food, refused to eat, and cried almost all evening. The next day her grandpa took her to their family physician’s clinic. It was noted that several children from her school had reported sore throats recently.
The patient had received all standard childhood immunizations at the appropriate times.
PHYSICAL EXAMINATION
LABORATORY STUDIES
Diagnostic Work-Up
Table 3-1 lists the likely causes of illness (differential diagnosis). A monospot test can be useful to rule out Epstein-Barr virus (EBV) infection. Additional tests for delineating the etiology may include
TABLE 3-1 Differential Diagnosis and Rationale for Inclusion (consideration)
Rationale: All of the above may cause pharyngitis. The patient had pharyngitis. Because it affects therapeutic decision making, it is important to attempt clinical differentiation between viral and bacterial pharyngitis. The clinical presentations for viral and bacterial pharyngitis overlap broadly. Viruses cause more than 70% of cases of pharyngitis. Mild pharyngeal symptoms with rhinorrhea suggest a viral etiology. High fever, tonsillar exudates, anterior cervical lymphadenopathy, and the absence of cough are the best predictive clinical features for bacterial pharyngitis or EBV infection. EBV is less likely to be symptomatic in this age group.
MICROBIOLOGIC PROPERTIES
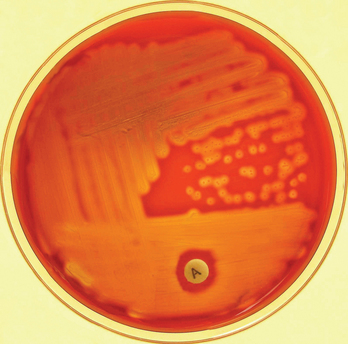
Streptococci are Gram-positive cocci in chains. S. pyogenes yield small colonies with clear, sharp β-hemolysis on blood agar culture (colonies are surrounded by a clear zone indicating complete lysis of red blood cells; Fig. 3-2). Throat culture is the standard for diagnosing streptococcal pharyngitis, and sheep blood agar incubated up to 48 hours is the culture medium of choice. The bacteria are catalase negative and bacitracin sensitive in a diagnostic disc susceptibility test. S. pyogenes is commonly known as group A β-hemolytic streptococcus (GABHS) for the presence of the cell surface group A carbohydrate antigen. RADT, a rapid (dipstick-based) test, which detects the presence of the cell-wall carbohydrate antigen in the throat swab, can be completed at the bedside in minutes. A positive RADT confirms the diagnosis, whereas a negative RADT requires confirmation with culture results.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree