Gastrointestinal Surgery
LEARNING OBJECTIVES
After studying this chapter the reader will be able to:
• Identify relevant anatomy of the gastrointestinal tract
• Correlate physiology to conditions requiring surgical intervention
• Discuss procedural considerations
• Identify tissue layers involved in opening and closing the gastrointestinal tract
• Compare diagnostic methods for determining surgical interventions and/or approaches
• Identify surgical incisions used in gastrointestinal surgery
• Identify instruments and equipment used in open and laparoscopic gastrointestinal procedures
• List the pharmacologic/hemostatic agents utilized during gastrointestinal surgery
• Review specific procedural steps as a guide for clinical procedure consideration
Overview
Surgery of the gastrointestinal (GI) system may be indicated to establish a diagnosis, to prevent or cure disease, to relieve symptoms or restore function, or to afford palliative measures that provide comfort or nutrition and promote quality of life. Advances in scientific knowledge, research, pharmacology, and technologic developments in the interventional disciplines as well as successful outcomes based on clinical evidence continue to broaden the spectrum of modalities and approaches to managing patients with GI disorders.
GI surgery, a subspecialty within the domain of general surgery, traditionally concerns itself with surgical management of the esophagus, stomach, small intestine, large intestine, and rectum. Gastroenterology is a medical specialty that diagnoses and manages GI disorders and conditions through endoscopic and pharmacologic approaches. Many surgical procedures that once entailed laparotomy and extensive postoperative recovery have been replaced or duplicated by endoscopic access and intervention. Endoscopic examination, enhanced with fluoroscopy, ultrasound, and video magnification in conjunction with interventional radiology, is a critical component of surgical diagnosis and postoperative evaluation. Laparoscopy, a minimally invasive approach to the intraabdominal compartment, has revolutionized GI surgery. Medical and surgical specialties have evolved to embrace and facilitate these advancements. Although clinicians may specialize in the disciplines of laparoscopy, gastroenterology, general surgery, bariatrics, GI surgical oncology, or colorectal surgery, the perioperative nurse and surgical technologist must know the fundamentals of GI surgery, interventional options available to patients, and care requirements common to all GI patients.
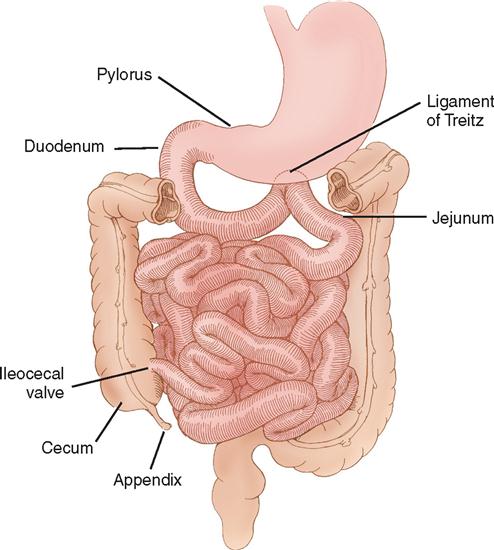
Surgical Anatomy
The GI tract, or alimentary canal, is a continuous tubelike structure that extends the entire length of the trunk (Figure 2-1). The tract includes the mouth; pharynx; esophagus; stomach; small intestine, consisting of the duodenum, jejunum, and ileum; and large intestine, which comprises the cecum, ascending colon, transverse colon, descending colon, sigmoid colon, rectum, and anus. The length of the GI tract in a cadaver is about 9 meters, or 30 feet. In a living person it is shorter because of sustained muscle contraction and tone. The six basic functions of the GI tract are ingestion, secretion, mixing and propulsion, digestion, absorption, and defecation.
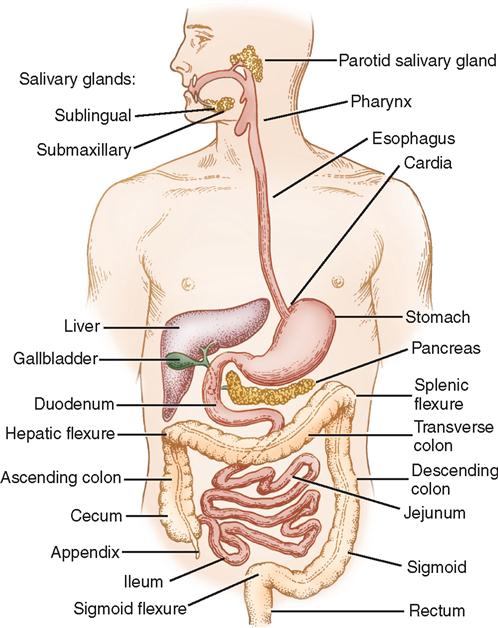
The esophagus extends from the pharynx, at the level of the sixth cervical vertebra, and passes through the neck, posterior to the trachea and heart, and anterior to the vertebral column. The lower portion of the esophagus passes in front of the aorta and through the diaphragm, slightly to the left of the midline, to join the cardia of the stomach. Blood is supplied to the esophagus from branches of the inferior thyroid arteries, bronchial arteries, thoracic aorta, and branches of the left gastric and inferior phrenic arteries. The nerve supply comes from branches of the vagus and sympathetic nervous system. The length of the esophagus in an adult is about 25 cm, or 10 inches. The esophagus is a collapsible musculomembranous tube that functions primarily to transport ingested material, by peristalsis, from the pharynx to the stomach.
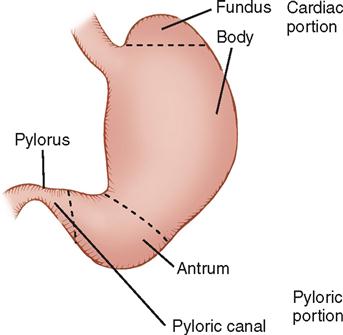
The stomach is an expanded J-shaped organ situated between the esophagus and the duodenum. It lies in the upper left abdominal cavity, slightly to the left of the midline and beneath the diaphragm. The stomach is divided into three parts: the fundus, the body, and the antrum (Figure 2-2). The fundus lies below the left dome of the diaphragm, behind the apex of the heart. The body and antrum lie in an oblique direction within the abdominal cavity. The stomach is stabilized indirectly by the lower portion of the esophagus and directly by its attachment to the duodenum, which is anchored to the posterior parietal peritoneum. The omentum, the peritoneal ligaments, and branches of the celiac vessel provide additional support to the stomach.
The convex, or lower, margin of the stomach is known as the greater curvature; the concave, or upper, margin is the lesser curvature. Attached to the greater curvature is the greater omentum, which is a double fold of peritoneum containing fat. It covers the intestines loosely and is not to be confused with the mesentery, which connects the intestines with the posterior abdominal wall. The left gastroepiploic branch of the splenic artery and the right gastroepiploic branch of the hepatic artery run through the greater omentum. The lesser omentum, attached to the lesser curvature of the stomach, contains the left gastric artery, a branch of the celiac axis, and the right gastric branch of the hepatic artery.
Stomach functions include acceptance and storage of ingested material; chemical and mechanical digestion through the production of gastric lipase, pepsinogen, hydrochloric acid, gastrin, and intrinsic factor, responsibility for the absorption of vitamin B12; and peristaltic waves, which both mix and propel stomach contents, or chyme, into the duodenum.
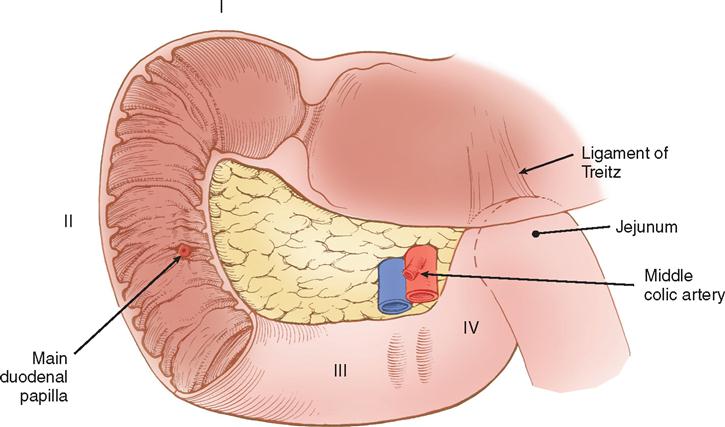
The small intestine, the longest part of the digestive tract, begins at the pylorus and ends at the ileocecal valve (Figure 2-3). The small intestine varies in size with the degree of contraction but is usually about 3 meters in length and 2.5 cm in diameter in the adult. It is divided into three parts: the duodenum, about 25 cm long; the jejunum, which is about two fifths of the length of the entire small intestine; and the ileum, which makes up the remaining length in an adult. The duodenum, which is the proximal portion of the small intestine, begins at the pylorus, is contiguous with the jejunum, and is stabilized by a fusion between the pancreas and the posterior parietal peritoneum. The duodenum is divided into four portions: superior (I), descending (II), transverse (III), and ascending (IV) (Figure 2-4). Nearly all of the superior portion mucosa is characterized by the lack of folds; it appears slightly dilated and is referred to as the duodenal bulb. The characteristic circular folds of the small intestinal mucosa begin proximal to the end of the superior portion of the duodenum and extend through the jejunum. They become less prominent in the ileum. The purpose of the circular mucosal folds, called plicae circulares of Kerckring or valvulae conniventes, is to provide greater mucosal surface area.
The common bile duct and the main pancreatic duct enter the medial wall of the middle of the second portion of the duodenum at the ampulla of Vater. The first, second, and third portions of the duodenum curve in a C-loop concavity in which the head of the pancreas is located. The fourth portion of the duodenum ascends to the duodenojejunal flexure. The duodenojejunal flexure is stabilized by the ligament of Treitz, which suspends the duodenum from the posterior body wall. The ligament of Treitz serves as a landmark during any abdominal exploration because it provides the surgeon with a reliable orientation of the patient’s anatomy.
The blood supply of the duodenum comes from the arterial branches of the celiac axis (Figure 2-5). The gastroduodenal artery branches off the hepatic artery and is located behind the duodenal bulb. At the inferior margin of the bulb, the gastroduodenal artery divides into the right gastroepiploic artery and a superior pancreaticoduodenal branch. The superior pancreaticoduodenal artery supplies blood to the proximal duodenum and head of the pancreas. The inferior pancreaticoduodenal artery branch of the superior mesenteric artery supplies blood to the third and fourth portions of the duodenum as well as to the head and body of the pancreas.

The jejunum, situated in the upper portion of the abdomen, joins with the ileum, situated in the lower portion of the abdominal cavity. The ileum empties into the large intestine through the ileocecal valve. The jejunum and ileum are suspended by the mesentery, which is attached to the posterior abdominal wall. The free border of the mesentery, which is about 5.5 meters (18 feet) long, contains branches of the superior mesenteric artery, many veins, lymph nodes, and nerve fibers. The blood supply to the jejunum and ileum comes entirely from the superior mesenteric artery. The small bowel contains major deposits of lymphatic tissue, known as Peyer’s patches, in the ileum. The rich lymphatic drainage of the small bowel plays a major role in fat absorption. Lymphatic drainage from the mucosa proceeds through the wall of the small intestine to lymph nodes adjacent to the mesentery. Lymphatic drainage then proceeds to larger lymphatics that communicate with the retroperitoneal cisterna chyli and from there to the thoracic duct. The lymphatics of the intestine play a major role in the body’s immune defense as well as in the distribution of cells arising from intestinal neoplasms.
Compared to the ileum, the jejunum has a larger circumference and thickness. The mesenteric vessels usually form only one or two arcades, a series of anastomosing arterial arches, compared with the multiple vascular arcades of the ileum. The jejunal mucosa is thick and has prominent plicae circulares. The ileum mucosa is thinner with few plicae.
The small intestine serves two important, but opposite, functions simultaneously. It absorbs essential nutrients at 95% efficiency while it provides an effective barrier from harmful ingested environmental elements. The remarkably large surface area of the combined small and large intestinal mucosa is estimated to be 200 square meters, about the size of a doubles’ tennis court.
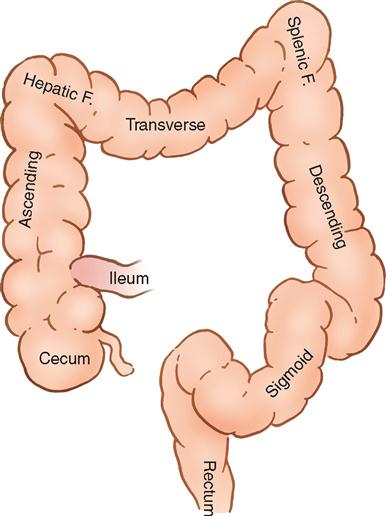
The large intestine begins at the ileocecal valve and ends at the anus. It is divided into the cecum, colon, and rectum. The cecum attaches to the ileum and extends about 7 cm below it. The cecum in an adult usually adheres to the posterior wall of the peritoneal cavity and has a serosal covering on its anterior wall only. The cecum forms a blind pouch from which the appendix projects.
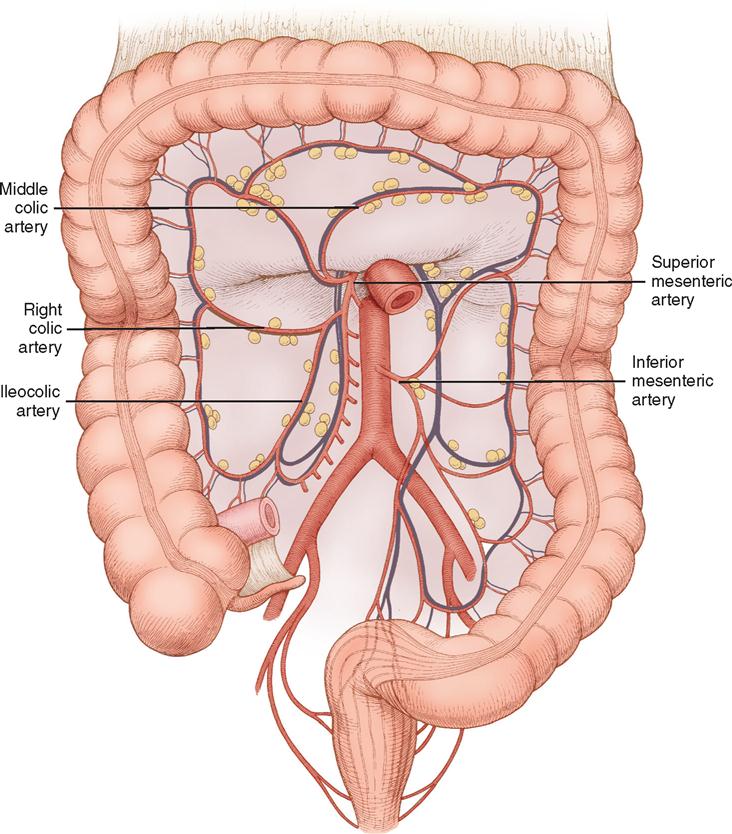
The colon, about 1.5 meters long, is divided into four parts: the ascending colon, the transverse colon, the descending colon, and the sigmoid colon (Figure 2-6). The ascending colon extends upward from the ileocecal valve to the hepatic flexure. The upper portion of the ascending colon lies behind the right lobe of the liver and in front of the anterior surface of the right kidney. The transverse colon begins at the hepatic flexure and ends at the splenic flexure. It lies below the stomach and is attached to the transverse mesocolon. The descending colon extends downward from the splenic flexure to just below the iliac crest. The iliac portion of the sigmoid colon lies on the inner surface of the left iliac muscle. The remaining portion of the colon passes over the pelvic rim into the pelvic cavity and lies partly in the abdomen and partly in the pelvis. It then forms an S-shaped curve in the pelvis and terminates in the rectum at the level of the third segment of the sacral vertebrae. The blood supply to the ascending colon, hepatic flexure, and transverse colon comes from the superior mesenteric artery, whereas the blood supply to the descending colon and rectum comes from the inferior mesenteric artery (Figure 2-7).
The wall of the colon consists of taeniae coli, epiploic appendices, and haustra. The taeniae coli are three longitudinal, or axial, strips of muscles distributed around the circumference of the colon. They represent the longitudinal muscle layer, which is not complete in the colon (the small intestine and rectum have both circular and complete longitudinal muscle layers). The epiploic appendices are fatty appendages along the bowel that have no particular function. The haustra are sacculations that outpouch from the bowel wall among the taeniae coli. The diameter of the colon varies in size from about 9 cm (3½inches) in the cecum to an average of about 1.25 cm (½inch) in the sigmoid colon.
The rectum begins at the sigmoid colon and ends in the anus. This slightly curved passage is surrounded by the pelvic fascia as it lies on the anterior surface of the sacrum and coccyx. In the male, the rectum lies behind the prostate gland, seminal vesicles, and bladder. In the female, the rectum lies behind the uterus and the vagina. A septum rectovesical, also called Denonvilliers’ fascia, separates the rectum from the urogenital structures. The rectum is suspended in the pelvis by fascia extending from the right and left pelvic sidewalls. Rectosacral fascia extends from the sacrum to the anorectal junction and suspends the rectum posteriorly. The rectum dilates just before it becomes the anal canal. This dilation, or ampulla, presents folds called Houston’s valves. The wall of the rectum consists of four layers, similar to those of the small intestine.
The anal canal is a narrow passage that passes downward and slightly posteriorly. It is surrounded and controlled by two circular muscle groups, which form the external and internal anal sphincters. The internal sphincter is a continuation of the longitudinal muscle layer.
The primary function of the large intestine is to reabsorb water and electrolytes, to form solid waste into feces, to synthesize vitamin K and B-complex vitamins, and to propel and eliminate solid food residue and waste through defecation.
The GI tract constitutes a complex microbiologic ecosystem that supports and maintains essential digestive and protective functions vital to life, yet it presents significant risks and challenges during diagnostic and surgical interventions. Substantial populations of microorganisms, both obligate anaerobes and facultative bacterial spores, exist in the intestinal lumen. The organisms of the upper tract differ from those of the lower tract, with the highest concentration in the distal bowel. These organisms can contribute to contamination and disease processes within the intestinal tract and throughout the body. Gastric and intestinal pH, while necessary for digestive benefit and protection from selected organisms, can compromise peritoneal tissues and structures when unplanned spillage or leakage occurs. The pH of the stomach ranges from 1.5 to 3, whereas the pH of the intestines can range from 7 to 8.5.
Surgical Technologist Considerations
GI surgery and endoscopic procedures present special considerations related to the planned procedure, instrumentation, approach, anatomic structures involved, health status of the patient, surgeon and patient preferences, and availability of special institutional resources. Special institutional resources may include a bariatric program, an oncology program with research protocols, a transplant program, a trauma center, or a technologically advanced OR with computer-integrated imaging display and robotics.
Optimum care of the patient undergoing GI surgery and other invasive GI procedures relies on sound knowledge and experience, along with a good understanding of the complex setups in the operating room. The experienced surgical technologist will be able to anticipate the need for specialized equipment based on the surgical procedure scheduled. An expert and attentive surgical technologist will hand the surgeon the appropriate instrumentation without being asked, based on an understanding of the procedural steps and anatomy involved. GI surgery can require a sterile and a nonsterile setup for the same patient. The surgical technologist should have a good understanding of bowel technique and the flexibility to move swiftly from the laparoscopic approach to an open approach should the need arise. The risks for injury or failure to achieve the intended outcome are equally present in GI surgery as in any surgical or invasive procedure. No procedure is routine, and unexpected outcomes can occur even when planning and preventive measures have been employed under the most optimal circumstances.
Laboratory studies might include a complete blood count (CBC) with differential, serum electrolytes, platelet count, cholesterol level, vitamin and mineral levels, liver function, serum proteins, coagulation profile, pancreatic function, and indices of nutritional status (Table 2-1).
TABLE 2-1
Common Serum Studies with Relevance to GI Surgery
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree