Cephalosporins

ACTION
Each generation has increasing bactericidal activity to break down gram-negative bacteria and anaerobes, as well as reach the cerebrospinal fluid. Cephalosporins interfere with bacterial cell wall synthesis and are considered broad-spectrum. The cell weakens, swells, bursts, and dies as a result of increased osmotic pressure inside the cell.
USES
• Is used widely in a variety of infections.
CONTRAINDICATIONS
• Because of cross-sensitivity, patients with allergies to penicillins
SIDE EFFECTS
• †Hypersensitivity reactions:† **rash, pruritus, fever**
• Anorexia, **nausea,** flatulence, **vomiting, diarrhea**
• Third-generation medications: †possible suprainfection†
• Cefmetazole, cefoperazone, and cefotetan may cause bleeding tendencies. Taking cefotetan and drinking alcohol may cause a serious disulfiram-like reaction.
NURSING IMPLICATIONS
1. Evaluate intramuscular (IM) and intravenous (IV) sites for reaction, such as abscess and thrombophlebitis. Minimize complication of thrombophlebitis by rotating injection sites and slowly injecting in a dilute solution.
2. *Monitor rate of infusion; check labeling for rate of IV infusion.*
3. *Monitor renal and hepatic studies throughout therapy.*
4. ‡Advise patient to hydrate; notify health care provider if patient is experiencing diarrhea.‡
5. With medications that cause bleeding tendencies, monitor for bleeding.
6. *If gastrointestinal (GI) upset occurs, patient can take medication with food.*
7. ‡Teach patient to refrigerate oral suspensions.‡
8. IM injections are frequently painful; forewarn patient.
9. Instruct patient to report any signs of allergy (e.g., skin rash, itching, hives).
Tetracyclines

CLASSIFICATION
Antibiotic
ACTION
Tetracyclines are bacteriostatic, broad-spectrum antibiotics that suppress bacterial growth and replication but do not kill the bacterial cells outright. These antibiotics are considered second-line drug agents used for infections resistant to first-line drugs by passive diffusion and active transport, competing for binding at subunit sites of RNA ribosome interfering with the bacteria’s ability to function and reproduce. This antibiotic is a bactericidal in large doses.
USES
• Rickettsial diseases (Rocky Mountain spotted fever, typhus)
• Chlamydia infections, peptic ulcer disease (Helicobacter pylori infection)
• Acne, Mycoplasma pneumoniae, Lyme disease, periodontal disease
PRECAUTIONS
• May result in renal and hepatic dysfunction.
• *Do not give to children (<8 yr) or pregnant women.*
• *May cause staining of developing teeth.*
SIDE EFFECTS
• **Nausea,** abdominal cramping, vomiting, diarrhea, †suprainfection,† **photosensitivity**
NURSING IMPLICATIONS
1. ‡Take on an empty stomach; antacids, milk products, and iron supplements should not be consumed until at least 2 hours after dose was taken.‡
2. *Do not administer to pregnant women or children under age 8 years to avoid tooth discoloration.*
3. †Monitor carefully for diarrhea because diarrhea may indicate a suprainfection of bowel (Clostridium difficile).†
4. Check dose and rate when delivering intravenously.
5. ‡Wear sunscreen and protective clothing.‡
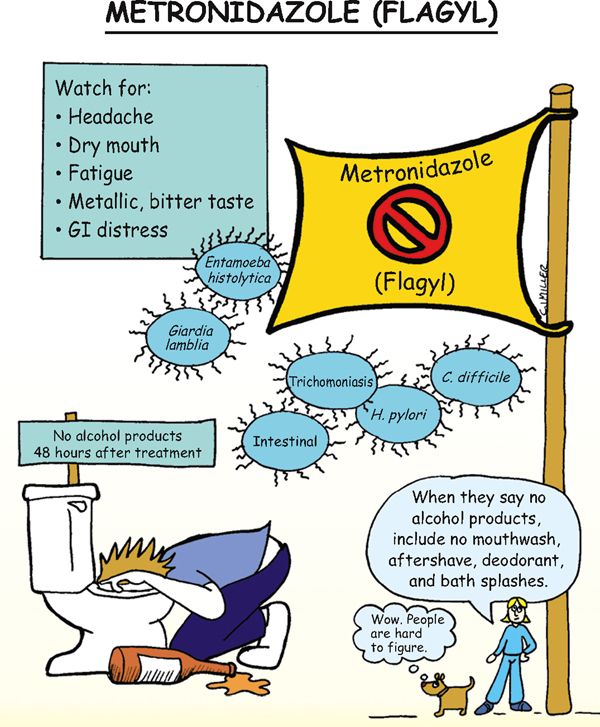
Metronidazole (Flagyl)

CLASSIFICATION
Antibacterial
ACTION
Direct trichomonacidal and amebicidal activity against Trichomonas vaginalis, Entamoeba histolytica, Clostridium difficile, and Giardia lamblia. Antibacterial activity against anaerobic bacteria, gram-negative anaerobic bacilli, and clostridia.
USES
• Asymptomatic and symptomatic trichomoniasis in female and male patients
• Acute intestinal amebiasis, giardiasis, and antibiotic-associated colitis
• Used in combination with tetracycline and bismuth subsalicylate (Pepto-Bismol) for treatment of Heliobacter pylori
CONTRAINDICATIONS
• Active central nervous system (CNS) disease, blood dyscrasias
• First-trimester pregnancy, breast-feeding mothers
PRECAUTIONS
• Second- and third-trimester pregnancies
SIDE EFFECTS
• **Nausea, headache, dry mouth,** vomiting, anorexia, epigastric distress
• **Metallic taste,** darkening of the urine, seizures
NURSING IMPLICATIONS
1. Take on an empty stomach if possible; may take with food if nauseated.
2. ‡Teach not to apply cologne, aftershave lotion, or bath splashes or ingest alcohol products to avoid a disulfiram-type reaction (e.g., flushing, nausea and vomiting, palpitations, tachycardia, psychosis).‡
3. ‡Mothers should wait until 3 days after last dose of drug to resume breast-feeding.‡
4. ‡Teach patient that harmless darkening of the urine may occur.‡
Isoniazid (INH)

CLASSIFICATION
Antituberculosis agent
ACTIONS
Bacteriostatic to “resting organisms” and bactericidal to actively dividing organisms. Interferes with biosynthesis of bacterial protein, nucleic acid, and lipids.
USES
• Treatment of all forms of active tuberculosis
• Preventive in high-risk persons (e.g., those with a positive tuberculosis [TB] skin test or exposure)
CONTRAINDICATIONS AND PRECAUTIONS
• History of isoniazid-associated hypersensitivity reaction
• Convulsive disorders or alcoholism
SIDE EFFECTS
• **Peripheral neuropathy,** clumsiness, unsteadiness, muscle ache
• Epigastric distress, jaundice, †drug-induced hepatitis†
NURSING IMPLICATIONS
1. ‡Teach patient to take orally on an empty stomach 1 hour before or 2 hours after meals.‡
2. *Depletes vitamin B6 (pyridoxine) and will need supplementation during treatment.*
3. *Peripheral neuritis, the most common adverse effect, is preceded by paresthesias (e.g., numbness, tingling, burning, pain) of the feet and hands.*
4. ‡Teach patients to reduce or eliminate consumption of alcohol to reduce risk of hepatotoxicity.‡
5. *Antituberculosis treatment always involves two or more medications;* INH is often combined with rifampin.
Remember this mnemonic for antibiotics used in TB: STRIPE
ST—streptomycin R—rifampin I—isoniazid P—pyrazinamide E—ethambutol
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree