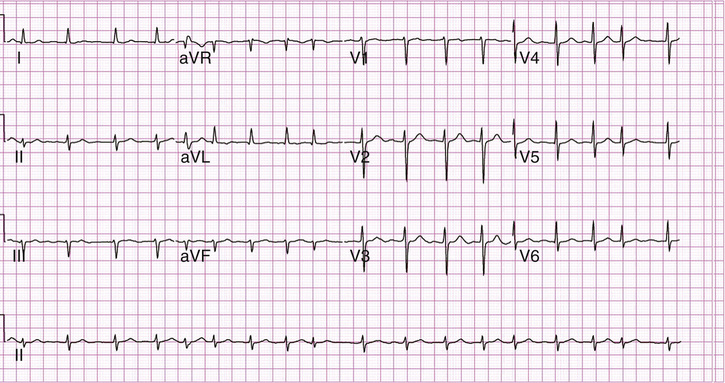
Gina Rossetti, Nida Hamiduzzaman, Eric Hsieh This ECG shows atrial fibrillation with a rapid ventricular response. This is characterized by an irregularly irregular ventricular rhythm, the absence of discrete P waves, and a narrow QRS complex. Atrial fibrillation can present with a rapid ventricular response characterized by a ventricular rate greater than 100 beats/minute. The ventricular rate generally ranges from 120 to 160 but can sometimes be greater than 200 beats/minute. Approximately 5% of all adults older than 70 years old will experience atrial fibrillation. Many patients are asymptomatic and the arrhythmia is found incidentally during medical evaluation. Patients can present with palpitations, dizziness, fatigue, and poor exercise tolerance. They can also have chest pain due to cardiac demand ischemia caused by the increased ventricular rate. This usually occurs in patients who have underlying coronary artery disease (CAD). Patients may present with signs of fluid overload such as an elevated jugular venous pulsation, crackles on lung exam, and peripheral pitting edema. Fluid overload can be due to decreased cardiac output caused by poor contraction of the ventricle or underlying structural heart disease. Hypotension due to reduced cardiac output can occur and may progress to cardiogenic shock. Atrial fibrillation is classified into three types. Lone atrial fibrillation occurs in patients with no structural heart disease and no identifiable precipitants. Despite no identifiable cause, the arrhythmia tends to recur and then becomes permanent. Paroxysmal atrial fibrillation occurs when the episodes of the arrhythmia are intermittent. The patient will often have episodes of atrial fibrillation that can last minutes to days and then will convert back to normal sinus rhythm spontaneously. Persistent atrial fibrillation indicates that the arrhythmia will not convert to normal sinus rhythm and thus will need medical therapy. Permanent atrial fibrillation indicates that the arrhythmia will not respond to therapy and normal sinus rhythm cannot be achieved. In a normal heart, the sinoatrial node in the right atrium will send an electric impulse to the atrioventricular (AV) node, which will generate a ventricular heartbeat at a rate of 50 to 80 beats/minute. This coordinated electrical impulse allows for effective contraction of the myocardium and thus normal cardiac output. In atrial fibrillation, electric impulses are produced by multiple ectopic foci, usually next to the origin of the pulmonary veins. This causes the atria to fibrillate, or contract in a disordered manner. The resulting disordered conduction through the AV node to the ventricles causes rapid, inefficient ventricular contraction and decreased cardiac output. The most common etiology is underlying structural heart disease in patients older than 65. Common causes of heart disease include long-standing hypertension, CAD, congestive heart failure (CHF), and valvular disease. If there is underlying heart pathology, atrial fibrillation is more likely to become persistent or permanent. In addition, there are identifiable triggers that are reversible. The most common are alcohol, hyperthyroidism, electrolyte abnormalities, stimulants, and pulmonary disease. Atrial fibrillation also occurs in the postoperative setting, specifically after cardiopulmonary operations in elderly patients and often abates on its own over 1 to 2 days. A portion of atrial fibrillation cases will have no identifiable cause and be deemed idiopathic. Patients are admitted if they show evidence of hypotension or fluid overload or if they have an associated medical condition that justifies admission. Examples include hypertensive emergency, cardiac ischemia, infection, or hyperthyroidism.
A 78-Year-Old Male With Palpitations and Lightheadedness
How would you interpret this ECG?
What are the common presenting signs and symptoms of atrial fibrillation?
How do you classify the types of atrial fibrillation?
What is the pathophysiology of atrial fibrillation?
What are some underlying etiologies of atrial fibrillation?
What are the criteria for hospitalization for atrial fibrillation?
What medications could you use to control the pulse rate?
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


19 A 78-Year-Old Male With Palpitations and Lightheadedness
Case 19