Trauma Surgery
LEARNING OBJECTIVES
After studying this chapter the reader will be able to:
• Identify common surgical procedures and interventions in trauma surgery
• Understand positioning, prepping, and draping of the surgical trauma patient
Overview
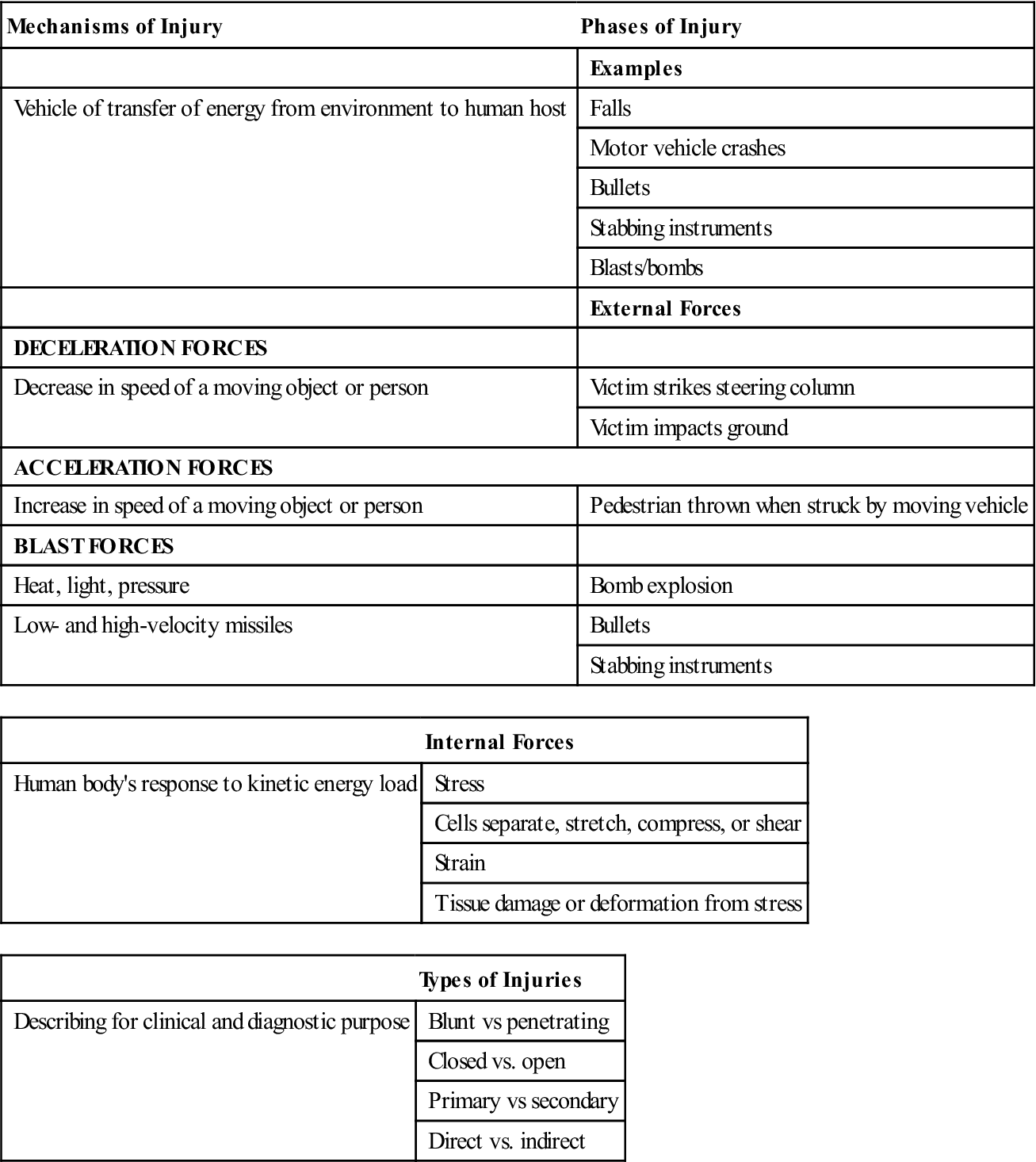
Trauma is ranked as one of the foremost public health issues in the United States today. Unintentional injury related to trauma is the fifth leading cause of death today and the leading cause of death for persons aged 1 to 44 years (Barclay, 2009). Trauma is the leading nonobstetric cause of maternal mortality and is associated with fetal mortality directly related to the severity of maternal injury (Cusick and Tibbles, 2007). Whether the injury is a result of a motor vehicle collision, violence, crime, or work-related injury, trauma occurs unplanned and without warning. The unpredictable nature of trauma poses a major challenge to the surgical technologist and the patient care team.
The potential for injury has existed since the beginning of humanity. Most of the major advances in care of critically injured patients have been accomplished through experience in the military. Clearly, the shorter the response time, the greater the survival rate for casualties. This was demonstrated by the success of the mobile army surgical hospitals (MASH) during the Korean conflict and again during the Vietnam conflict; MASH brought the necessary supplies, equipment, and personnel closer to the battlefields and, consequently, improved patient outcomes.
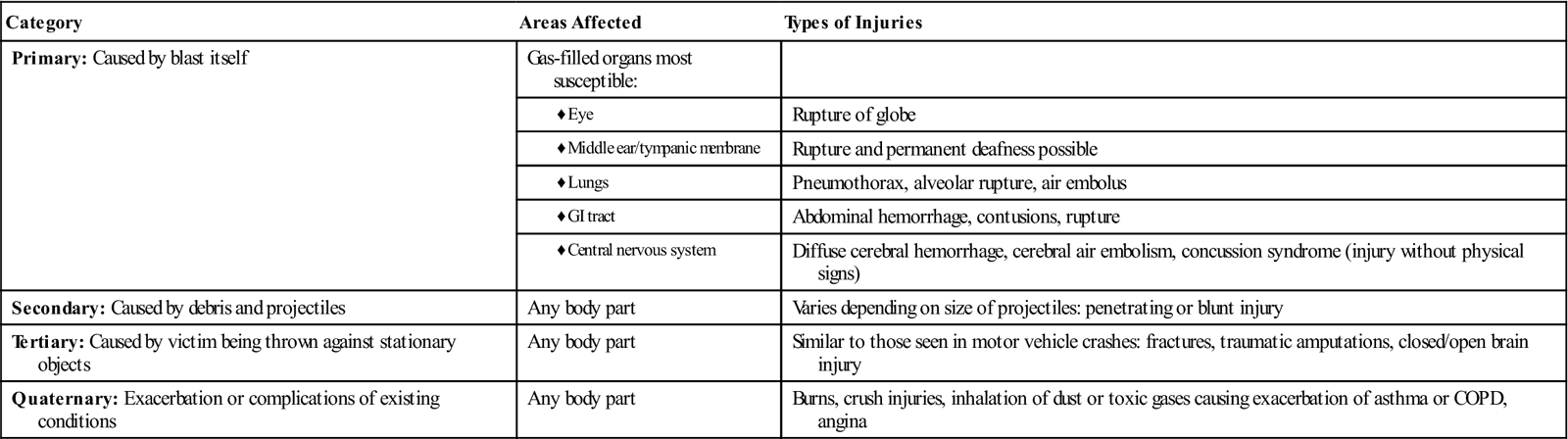
Eventually this concept was applied to the civilian population and is now commonly referred to as the “golden hour” of trauma care. More specifically, the golden hour refers to the time immediately after the injury when rapid and definitive interventions can be most effective in the reduction of morbidity and mortality. The golden hour starts at the scene, where prehospital personnel determine the severity of injury, initiate medical treatment, and identify the most appropriate facility to which to transport the patient. Traumatic deaths may occur in three phases, or time frames. The first occurs immediately after the injury. This accounts for approximately 50% of the deaths from trauma and is usually a result of lacerations to the heart or aorta or brainstem injury. These patients rarely survive transport to the hospital and die at the scene. The second phase occurs within the first 1 to 2 hours after the injury, representing approximately 30% of total fatalities. These patients have injuries to the spleen, liver, lung, or other organs that result in significant blood loss. This is the group in which definitive trauma care (i.e., appropriate and aggressive resuscitation with adequate volume replacement) may have the most significant effect (the golden hour). The third phase occurs days to weeks after the injury, often during the intensive care phase, and is usually caused by complications or a failure of multiple organ systems.
The wars in Iraq and Afghanistan have resulted in some changes in the way traumatic injuries are managed; the military has not set up convalescence centers as in Vietnam and Desert Storm. Rather, the doctrine of “essential care in theater” is followed. Physicians and nurses have been trained to provide immediate care, keeping in mind the treatment resources that will be available at the next level of care. Soldiers with upper body injuries are surviving because of body armor. However, there is no protection for upper extremities; therefore there are many amputations being performed, including above-elbow and shoulder disarticulations. The new philosophy is to stress continuity of care with the goal of returning the soldier to the highest possible level of function.
Time is of the essence in providing definitive care to the critically injured person. A significant number of patient deaths can be prevented if rapid transport is provided from the scene to a facility equipped to provide resuscitation and treatment in an efficient and timely manner. This concept is reflected in the national development of the Emergency Medical Services (EMS) system. Facilities and resources are allocated and coordinated to provide specific interventions for a group of patients. For example, facilities that meet certain criteria to accommodate the specialized needs of the critically injured patient are designated as trauma centers. Communities establish transfer and triage protocols that allow for a trauma patient to reach the appropriate facility with the least out-of-hospital time possible. This may be accomplished by a helicopter with a specially trained flight crew or by the use of ground transport with an Advanced Life Support (ALS) ambulance team (Figure 18-1).
Trauma centers (TC) are classified based on the scope of services and resources that are available. A level I TC is capable of providing total care for every type of injury. Accepting this designation commits the TC to providing qualified personnel and equipment necessary for rapid diagnosis and treatment on a 24-hour basis. A level II TC provides comprehensive care for all injuries but lacks some of the specialized clinicians and resources required for the level I designation. A level II facility may provide surgical intervention if the critical nature of the injury dictates immediate intervention before transfer to a level I facility. A level III facility provides prompt evaluation, resuscitation, emergency surgery, and stabilization, as needed, before transfer to a higher-level facility. The American College of Surgeons (ACS) recommends that in level II and III centers, an OR team is readily available at all times. Depending on the population served and the volume of urgent cases, this requirement may be met with on-call staff. A level IV trauma center has the ability to provide advanced trauma life support before patient transfer. These facilities may be located in rural areas with limited access and may be a clinic or a hospital.
Although the risk for death is 25% lower for a severe injury treated in a level I TC (Barclay, 2009), not all patients require the services of a level I TC and so may be transported to the closest emergency department for care. New guidelines and recommendations for triage, first developed as a position statement by the ACS in 1986, have been published (Barclay, 2009). Known as the “Decision Scheme,” this algorithm guides EMS personnel through the following four decision points: physiologic parameters, anatomic parameters, mechanism of injury (MOI), and other special considerations. Personnel review physiologic parameters. Patients with a Glasgow Coma Scale score less than 14, systolic blood pressure less than 90 mm Hg, or respiratory rate less than 10 breaths per minute or greater than 29 breaths per minute should be transported to the highest level facility available. The anatomic parameters include specific types of injuries, such as penetrating injuries of the neck or torso, flail chest, or proximal long bone fracture; these patients are also transported to the highest level facility available. The MOI and other special considerations, such as age or prior medical history, are also reviewed to determine to what level facility the patient is transported (History box).
Trauma patients require immediate access to the OR 24 hours per day, 365 days per year. A sudden influx of a large number of trauma patients to a trauma center may necessitate triage or classification of those less seriously injured as less urgent, allowing immediate access for the critically injured patients. The elective surgery schedule may need to be interrupted to expedite care for the trauma patient or patients. Scheduling policies and procedures are established collaboratively by the departments of surgery, trauma, anesthesia, and perioperative nursing services. Consequently, the perioperative nurse and surgical technologist need to be familiar with supplies and equipment located in the OR designated for trauma or in the ORs that are used most frequently for these patients.
Surgical Technologist Considerations
When dealing with the unpredictable timing, it is often the on-call perioperative team who cares for the injured patient requiring surgery. In contrast to an elective surgical procedure, the team may know very little about the trauma patient. The surgical team may be working with reduced preparation before the patient enters the operating room. Speed and efficiency will be the key to the successful outcome of the trauma patient.
An experienced surgical technologist will have the clinical knowledge to prepare for unexpected complications, such as increased hemorrhage, multiple surgical teams, and a large number of equipment and supplies. The ability to prioritize and work calmly and collaboratively with the team enhances the level of patient care.
After the type of traumatic injury has been identified, the surgical technologist will select the appropriate equipment and supplies. Blunt trauma can present a greater risk to the patient than penetrating trauma. Because it is more difficult to identify and treat blunt trauma, the surgical technologist will need to have specific instruments to gain quick access to the site of the injury.
If it is blunt trauma to the abdomen, a laparotomy set of instruments and supplies is appropriate. Understanding that there will be a need for multiple sponges, suture, and ties, as well as having the appropriate electrosurgical equipment available, is key. Blunt trauma to the head will require the surgical technologist to be prepared for either burr holes or a craniotomy. The surgeon will need to quickly relieve the pressure on the brain; the ability to set up the specialized power equipment is paramount for the surgical technologist.
In penetrating trauma, there may be injuries to surrounding anatomic structures, which most often include the liver, spleen, intestines, and vascular system. The surgical technologist may need to secure lasers, anastomotic stapling devices, specialty instruments, and suture or vascular grafts to be prepared to effectively assist the surgeon.
The skin prep for traumatic injuries will vary depending on the location of the injury and the preference of the surgeon. Assisting to open and set up the sterile prep will facilitate a more expeditious start time. If there is debris present in the wound, the prep may need to include a sterile scrub brush or powerized irrigation equipment. While removing the debris, it is crucial to use caution to prevent further injury.
Results of diagnostic studies including x-ray films, CT scans, and MRIs, as well as lab values, are beneficial to the perioperative team, because these results can help guide the correct selection of instruments, supplies, and equipment.
With the knowledge that there may be several healthcare providers or multiple teams working on the patient simultaneously, room setup and traffic flow become extremely important to ensuring sterility in the room.
Understanding it will be difficult to regulate body temperature in the trauma patient, appropriate warming devices and fluids need to be readily available. Complicating this will be dealing with hypothermia and thermal injuries; these present the perioperative team with additional steps to ensure optimal patient outcomes.
Stress debriefing is very important to the entire perioperative team. Most surgical interventions are of the curative nature, while trauma can result in less than optimal outcomes for the patient, including death. Learning to openly discuss the feelings and emotions this particular type of surgery evokes is an important part of becoming a successful trauma team member. It is imperative for healthcare providers to care for themselves as well as their patients.
Assessment
The resuscitative process begins with arrival of emergency personnel on the scene and ends when the patient has been stabilized, received definitive care, and undergone a complete and thorough physical examination to determine all injuries sustained. When the patient arrives in the ED, the trauma team initiates a primary assessment. This is a logical, orderly process of patient assessment for potential life threats. These assessment activities are based on established protocols for advanced trauma life support (ATLS). The mnemonic “ABCDE” is used, representing assessment of the following:
Airway interventions may include manual maneuvers (chin-lift, jaw-thrust), insertion of oral or nasopharyngeal airways, or intubation. The trauma team may also perform emergent procedures, such as tracheotomy or needle cricothyrotomy, to secure the patient’s airway. Pulse oximetry and capnography monitoring are used. If cervical spine precautions were not implemented before arrival at the hospital, the team initiates them before performing any other procedures on the patient. A trauma team member can stabilize the head and neck, if necessary, until a cervical collar is placed. Once placed, the team does not remove it until a cervical radiograph clears the neck of injury.
During this time, the surgeon or ED physician and trauma team identify and correct life threats that are present before progressing to the next part of the examination. A patient requiring immediate surgery is transported to the OR, undergoes surgical intervention, and then is transferred to the postanesthesia care unit (PACU) or intensive care unit (ICU), depending on his or her condition. On the other hand, a patient may have a penetrating wound with evisceration of abdominal contents. However, correcting the obvious defect, which is currently not life-threatening, is postponed until the trauma team is assured that the patient has a patent airway and an effective breathing pattern and cervical spine precautions have been implemented. An evisceration needs to be corrected, but an inadequate airway is an immediate life threat and assumes priority.
Depending on the patient’s injury, the surgeon may order an arterial blood gas (ABG) measurement. This test provides an accurate assessment of the ventilatory status of the patient and also evaluates resuscitative airway and breathing interventions (Table 18-1). Metabolic acidosis or a large base deficit (pH <7.35 or >7.45), with all other causes ruled out, may indicate internal bleeding.
TABLE 18-1
Laboratory Values: Arterial Blood Gases (ABGs)
| NORMAL VALUES | ||
| PaO2 | Pressure of oxygen in arterial blood | 80-100 mm Hg |
| PaCO2 | Pressure of carbon dioxide in arterial blood; measurement of how well lungs are discarding carbon dioxide (CO2 level is controlled by lungs) | 34-45 mm Hg |
| pH | Acidity or alkalinity of arterial blood; measurement of hydrogen ion concentration | 7.35-7.45 |
| HCO3− | Amount of bicarbonate in arterial blood; controlled by kidneys | 21-28 mEq/L |
| O2 saturation | Percentage of hemoglobin that is carrying oxygen | 95-100% |
| ABNORMAL VALUES | POSSIBLE CAUSE | |
| PaO2 | <50 mm Hg | Hypoxia |
| PaCO2 | >45 mm Hg | Hypoventilation/CO2 retention by lungs |
| pH | <7.35 | Acidosis |
| >7.45 | Alkalosis | |
| HCO3− | <22 mEq/L | Renal excretion of too much bicarbonate |
| >26 mEq/L | Renal retention of too much bicarbonate |
Modified from Pagana KD, Pagana TJ: Mosby’s diagnostic and laboratory test references, ed 9, St Louis, 2009, Mosby.
After the trauma team completes the primary assessment and corrects any immediate life threats, they perform a secondary assessment. The purpose of the secondary assessment is to identify all injuries present. Sometimes the secondary assessment may be completed by the perioperative team, the PACU nurse, or the critical care nurse. This assessment is a more in-depth, head-to-toe evaluation of the patient. Inspection, palpation, percussion, and auscultation are used in the complete head-to-toe assessment to reveal any deformities, open injuries, tenderness, or swelling. The assessment begins at the head and face and then moves to the neck (including the spine), the chest, the abdomen, and the pelvis. The four extremities are next; distal pulses, motor function, and sensation are assessed. The final check is the back; the patient is carefully log-rolled to the side for a full visual and tactile assessment (Evidence for Practice).
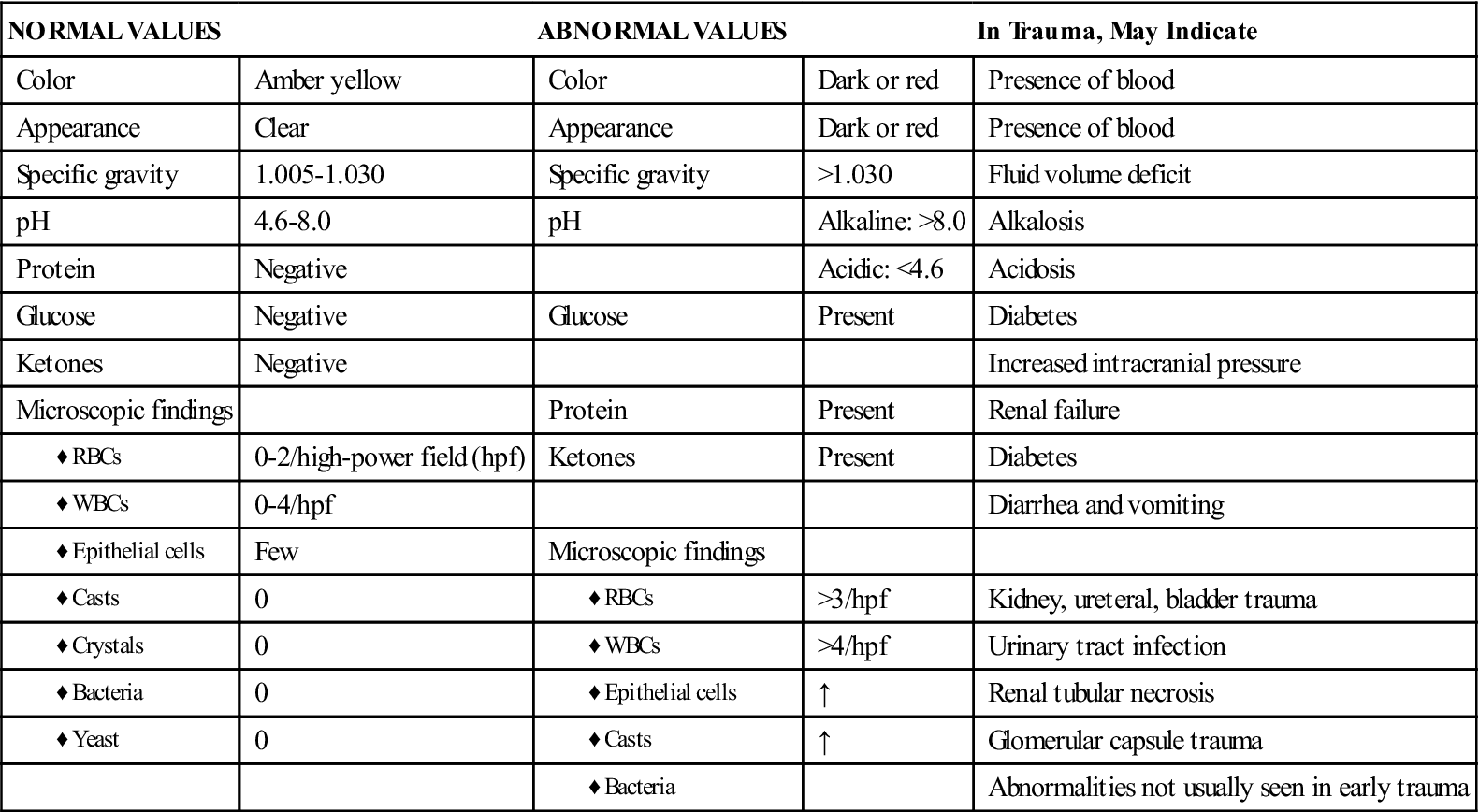
The patient’s vital signs, including a rectal or tympanic temperature, unless contraindicated, are obtained. Often during resuscitation, a Foley catheter is inserted to monitor urine output and fluid resuscitation efforts. The circulator should inspect the urinary meatus for the presence of blood before inserting the catheter. If blood is noted, the circulator notifies the surgeon and does not insert the catheter. The patient may have a ruptured bladder or a urethral injury, either of which is commonly associated with a fracture of the pelvis. The surgeon may wish to perform a retrograde urethrogram to examine the bladder and urethra for the presence of tears or disruption. After catheter insertion, urine is obtained for a urinalysis and urine drug screen. The identification of specific drugs in the urine may assist in further diagnosis and treatment. The urine will also be tested to determine the presence of red blood cells (RBCs) (Box 18-1). Depending on the amount of hematuria present, a renal contusion or other renal injury may be present. In addition, a nasogastric tube may be inserted at this time.
The circulator obtains a brief history from the family or significant others when possible. This history is referred to as the “AMPLE” history and may be obtained even after the patient is transferred to the OR by the ED personnel. The history includes the following:
If the history is obtained after the initiation of surgery, it is important to communicate it to the surgeon and the anesthesia providers.
Routine Laboratory Tests.
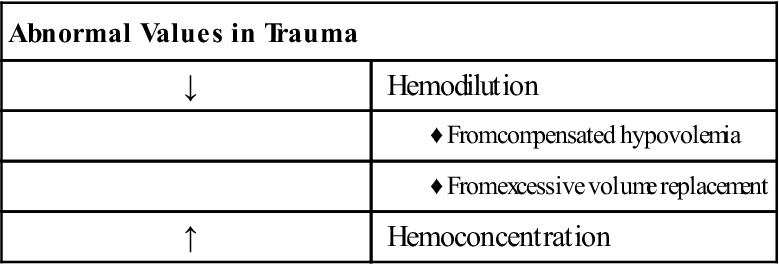
Laboratory values aid the trauma team in evaluating the patient’s status. Appropriate laboratory tests include a minimum of a complete blood count (CBC), hemoglobin and hematocrit (H&H) value, blood alcohol level (BAL), and a blood type and screen; other tests may be requested during evaluation. The results of the laboratory studies should be reviewed and communicated as appropriate (Box 18-2). An abnormal level of RBCs may signify dehydration, hypovolemia, or fluid overload (dilutional). An elevated white blood cell (WBC) count, indicating the presence of infection, may be related to inflammation, tissue necrosis, or immunocompromise. H&H values are also important to note. Caution is advised in evaluating an H&H drawn in the ED. The time delay between bleeding and a drop in the H&H value can be significant. It is only after hemodilution occurs (from shock compensation or crystalloid replacement) that hematocrit level drops. Frequently, abnormal values in the patient with blunt trauma alert the team to the possibility of internal bleeding.
BAL also assists the trauma team in their evaluation. If the patient’s level is significantly high, the physical examination and response may be unreliable. In addition, the neurologic status of patients with high BALs is very difficult to assess. Abnormal clotting studies are of obvious significance in trauma patients. These results may be attributable to anticoagulant medication the patient is taking or the effects of profound hypothermia. Clotting times may also be prolonged in the presence of excessive alcohol ingestion or the use of anabolic steroids. Clotting times may decrease with the use of antihistamines and diuretics.
A blood type and screen shortens the time needed by the blood bank to obtain a crossmatch, if needed later. Most trauma centers have several units of type O–negative blood (universal donor) available in the event that a blood transfusion is required before a type and crossmatch (T&C) can be performed. Because of regional shortages of O-negative blood, O-positive blood can be used in male patients and adult female patients of non-childbearing age. Initially, trauma patients are fluid-resuscitated with warmed crystalloid solutions, such as lactated Ringer’s solution or normal saline solution. If the patient’s blood pressure responds, the diagnostic examination continues. However, if the hypotension returns, blood transfusions may be initiated and the patient may be transported immediately to the OR for exploratory surgery.
Many trauma centers are implementing massive transfusion policies (MTP) for the clinical management of patients experiencing massive hemorrhage and to coordinate interdisciplinary and interdepartmental resources. Nessen and colleagues (2008) define massive transfusion as the replacement of one or more blood volumes within a 24-hour period, or 50% of estimated blood volume in 3 hours or less. This volume is approximately equal to the transfusion of 10 units of RBCs. Current research (Malone et al, 2006) suggests that improved patient outcomes are associated with the use of packed RBC/plasma/platelet ratios of 1:1:1. This simple ratio not only is easy to use but also has the benefit of administration of higher plasma and platelet volumes.
Diagnostic Procedures
RADIOLOGY.
Depending on the trauma center protocol, a blunt trauma radiographic series may be part of the resuscitative phase. This minimally includes a lateral view of the cervical spine and an anteroposterior (AP) view of the chest. In addition, the patient also undergoes lateral thoracic and lumbar spine films and an AP view of the pelvis. Any area with deformity, swelling, or pain may also be examined by x-ray. Trauma patients are always treated as if they have a cervical spine injury until proven otherwise. When reviewing the cervical spine films for cervical spine injury clearance, the clinician should consider any existing factors that place the patient at high risk for spine injury. These include age older than 65 years, a dangerous MOI, and paresthesias in the extremities. Patients with penetrating trauma injuries usually are transferred immediately to the OR for exploratory laparotomy.