 Pediatric Dosages
Pediatric Dosages
LEARNING OBJECTIVES
On completion of the materials provided in this chapter, you will be able to perform computations accurately by mastering the following mathematical concepts:
1 Converting the weight of a child from pounds to kilograms
2 Converting the neonate and infant weight from grams to kilograms
3 Performing pediatric dosage calculations
4 Calculating the single or individual dose of medications
5 Determining whether the prescribed dose is safe and therapeutic
6 Calculating a safe and therapeutic 24-hour dosage range
7 Calculating the single dose range from a 24-hour dosage range
9 Calculating pediatric IV solutions
10 Administering IV medications to pediatric patients
11 Calculating the daily fluid requirements for infants and young children
12 Calculating the body surface area (BSA) for medication administration
![]() Children are more sensitive than adults to medications because of their weight, height, physical condition, immature systems, and metabolism. Nurses who administer medications to infants and children must be vigilant in determining whether the patient is receiving the correct medication. The correct dose is one of the six rights of drug administration: right patient, medication, route, time, dose, and documentation.
Children are more sensitive than adults to medications because of their weight, height, physical condition, immature systems, and metabolism. Nurses who administer medications to infants and children must be vigilant in determining whether the patient is receiving the correct medication. The correct dose is one of the six rights of drug administration: right patient, medication, route, time, dose, and documentation.
The physician or provider will prescribe the medication to be delivered. However, the nurse is responsible for detecting any errors in calculation of dosage, as well as for preparing the medication and administering the drug. The nurse needs to be aware that pediatric dosages are often less than 1 mL; therefore a tuberculin syringe is used for accurate dosing.
Pediatric medications are calculated using the infant or child’s kilogram weight. The dosages have been established by the drug companies. Safe and therapeutic (S&T) dosages are readily available from a reliable source such as The Harriet Lane Handbook.
In general, pediatric dosages are rounded to the nearest tenth. For infants and young children, doses may be rounded to the nearest hundredth. The child who weighs more than 50 kg may receive adult dosages. If the calculated dose is greater than the recommended adult dose, DO NOT administer the medication. A child should not receive higher doses than those recommended for the adult, ever. Many drugs have a “do not exceed” or “max. dose” in 24 hours listed; this must always be considered.
Additionally, the physician or pharmacist may use the child’s body surface area (BSA) to calculate a dosage of medication to administer. The BSA calculation may be used when an established dosage has not been determined by the drug company, as with some anticancer or specialized drugs.
KILOGRAM CONVERSIONS
Converting Pounds to Kilograms
Infant’s and young children’s weight in pounds must be converted to kilograms to accurately calculate medication doses and daily fluid requirements. S&T drug dosages have been established using kilogram weights.
Always round the kilogram weight to the nearest tenth, NOT a whole number.
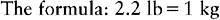
EXAMPLE 1: An infant weighs 24 lb. Convert the infant’s weight to kilograms.
| Proportion | Formula Setup |
| 2.2 lb : 1 kg :: 24 lb : x kg | 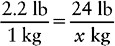 |
| 2.2 : 1 :: 24 : x | |
| 2.2x = 24 | 2.2x = 24 |
 | x = 10.9 kg |
| x = 10.9 kg |
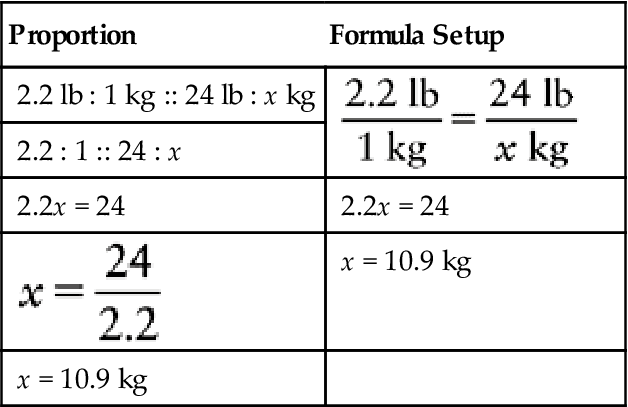
EXAMPLE 2: A child weighs 47 lb. Convert the child’s weight to kilograms.
| 2.2 lb : 1 kg :: 47lb : xkg | 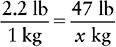 |
| 2.2 : l :: 47 : x | |
| 2.2x = 47 | 2.2x = 47 |
 | x = 21.4 kg |
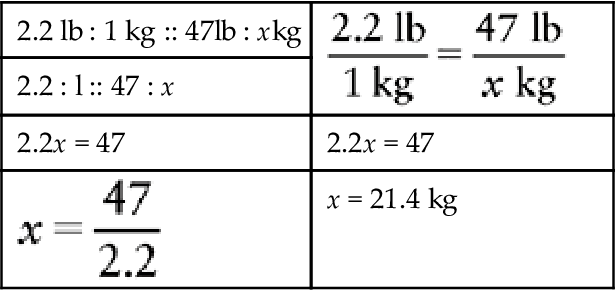
x = 21.36 kg or 21.4 kg (rounded to the nearest tenth)
Converting Grams to Kilograms
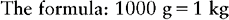
Newborn (neonate) and some infant weights are measured in grams. Converting grams to kilograms is done as shown below or by simply dividing the number of grams by 1000.
EXAMPLE 1: A neonate weighs 2300 g. Convert to kilograms.
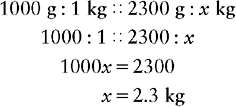
EXAMPLE 2: A newborn weighs 4630 g at birth. Convert to kilograms.
Practice Problems
Convert pounds and grams to kilograms.
Answers
PEDIATRIC DOSAGE CALCULATIONS
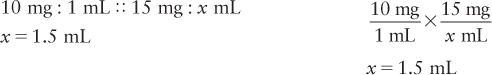
In pediatric dosage calculations, you can use a proportion or formula method.
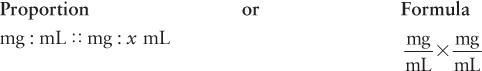
EXAMPLE 1: The physician orders Benadryl 12.5 mg po q4–6 h prn for itching. The nurse has available Benadryl 25 mg/5 mL. How many milliliters would be needed to administer 12.5 mg? Show math.
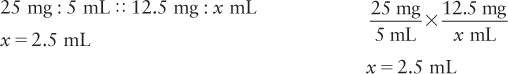
Example 2: The physician orders morphine 15 mg by intravenous (IV) piggyback (IVPB) now. You have available morphine 10 mg/mL. How much would you give? Show math.
CALCULATING THE SINGLE OR INDIVIDUAL DOSE (MILLIGRAMS/DOSE)
Medications such as acetaminophen and ibuprofen are administered as a single dose. This means that each time the infant or child receives the medication, it is calculated in a single or individual dose based on the kilogram weight.
Most of the medications prescribed in this manner are prn medications, which are given as needed for relief of symptoms such as pain, nausea, and fever. Again, the manufacturer of the drug has established an S&T dosage or range. The nurse is responsible for administering the single dose that is S&T. Therefore it is helpful for the nurse to know how the ordered dose is derived.
To determine the correct single dose for the child, you must calculate the correct dose. A systematic approach is helpful in determining the S&T dose range:
• Change the child’s weight in pounds to kilograms.
• Find the recommended dosage in a reliable source.
• Multiply the kilogram weight by the recommended dose(s).
EXAMPLE 1: A child weighs 22 lb. The child needs acetaminophen for pain and fever.
| a. Weight | 22 lb = 10 kg |
| b. Recommended | 10 to 15 mg/kg/dose q4–6 h |
| c. Calculation |

The child may receive 100 to 150 mg each time he or she is given acetaminophen. This is the single or individual dose. The dose is both safe and therapeutic for this child.
EXAMPLE 2: Calculate an S&T dose range of ibuprofen for a child who weighs 36 lb. Ibuprofen is available as 100 mg/5 mL. How many milliliters would you need to administer for the ordered dose to be S&T?
| a. Weight | 36 lb = 16.4 kg |
| b. Recommended | 5 to 10 mg/kg/dose q6–8 h |
| c. Calculations |

The S&T single dose range for this child is 82 to 164 mg/dose.
d. Now perform dosage calculations for the single dose range using the 100 mg/5 mL strength:

DETERMINE WHETHER THE PRESCRIBED DOSE IS SAFE AND THERAPEUTIC (MILLIGRAMS/KILOGRAM/DOSE)
This method will determine whether the child is receiving an S&T dosage of the drug that is prescribed by the physician. The nurse must determine whether the ordered dose is within the recommended range.
Even though the physician has prescribed the medication to be given, it is the nurse’s responsibility to determine whether the dose is S&T to administer to the child. This is done by dividing the ordered dosage by the child’s weight in kilograms (mg/kg/dose). A systematic approach is needed.
• Obtain the child’s weight in kilograms.
• Divide the ordered dose by the child’s weight.
• The answer is the mg/kg/dose (for each dose administered).
• Check your drug book to determine whether the ordered dose is S&T (in the recommended dosage range).
EXAMPLE: The doctor has ordered 210 mg of acetaminophen q4–6 h for pain and fever for a postoperative child. The child weighs 39 lb. The recommended dose range for acetaminophen is 10 to 15 mg/kg/dose q4–6 h. Acetaminophen is supplied as 160 mg/5 mL.
Is the ordered dose S&T to administer? If the dose ordered is S&T to administer, how many milliliters will be needed?
| a. Weight | 39 lb = 17.7 kg |
| b. Ordered | 210 mg q4–6 h |
| c. Calculation | 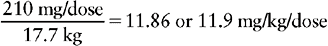 |
| d. Recommended | 10 to 15 mg/kg/dose |
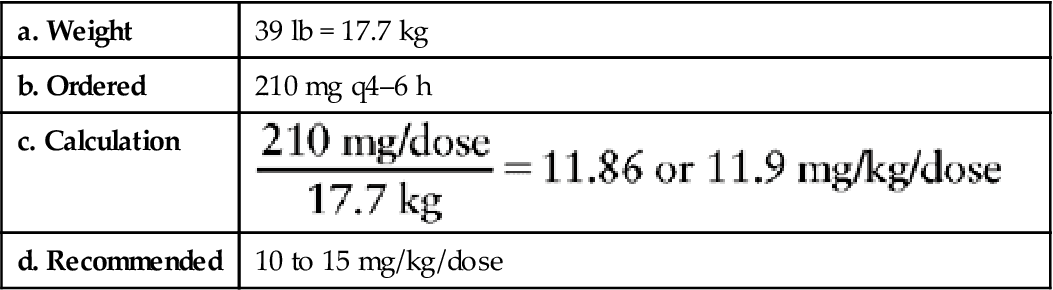
The patient will receive 11.9 mg/kg/dose. Yes, it is safe to administer the acetaminophen because it is within the S&T dosage range of 10 to 15 mg/kg/dose.
e. Perform dosage calculation using 160 mg/5 mL concentration:
160 mg : 5 mL :: 210 mg : x mL
160x = 1050
x = 6.6 mL rounded to the nearest tenth
Remember to round all doses to the nearest tenth.
Exceptions: Round all narcotics, antiepileptics, and cardiac medications to nearest hundredth. Medications that may be rounded to the nearest hundredth include phenobarbital, morphine, dilantin, digoxin, and anticancer drugs.
CALCULATE THE 24-HOUR DOSAGE (RANGES)
Many drugs are calculated based on the recommended 24-hour dose, then divided into single doses to be given every 12, 8, 6, or 4 hours or as recommended by the drug manufacturers. These divided time schedules vary, and the physician, nurse practitioner, or physician’s assistant will order the medication based on the recommended schedules.
Antibiotics especially are given this way.
Additionally, an antibiotic may be given in dosages or ranges that have been found to be effective for the child’s diagnosis. The physician chooses how often the medication is to be delivered. An example of an antibiotic with many dosing choices is ampicillin.
Recommended dosages for ampicillin may be any of the following:
| <2kg | 50 to 100 mg/kg/24 h/q8 h |
| >2kg | 100 to 200 mg/kg/24 h/q8 h |
| Mild to moderate infection | 100 to 200 mg/kg/24 h/q6 h |
| Severe infection | 200 to 400 mg/kg/24 h/q4–6 h |
The physician must determine the dosage to be given to the infant or child.
If an infant or child is diagnosed with otitis media (OM), then the physician may choose the dosage of antibiotic in the mild to moderate range. However, if an infant is admitted with a diagnosis of fever of undetermined origin, sepsis, or meningitis, then the physician may decide to prescribe a larger dosage of the antibiotic, as in the severe infection range.
Knowing the diagnosis is helpful in determining whether the infant or child will be receiving S&T dosages of antibiotics. Nurses who administer antibiotics or antiinfectives can learn how to determine the doses needed for the patient. However, only the physician, advanced practice nurse, or physician assistant can prescribe and order the infant’s or child’s medications.
EXAMPLE 1: An infant is admitted to the hospital to rule out sepsis. The infant weighs 8 lb. Ampicillin is prescribed. Calculate an S&T 24-hour dosage range for this infant with a possible severe infection.
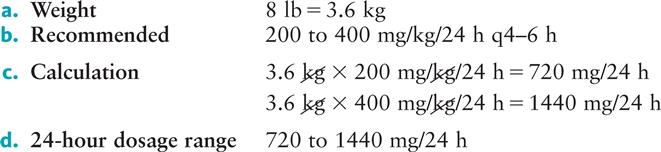
This means the infant can receive 720 to 1440 mg of ampicillin in a 24-hour period.
EXAMPLE 2: The child weighs 35 lb and is diagnosed with OM. The physician prescribes amoxicillin. Calculate an S&T 24-hour dosage range for this patient.
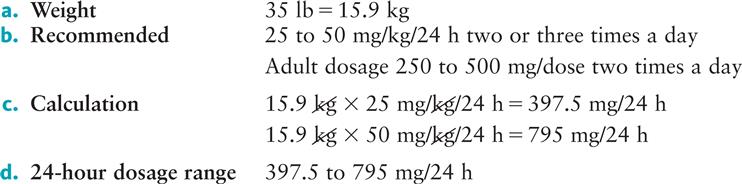
The child may receive 397.5 to 795 mg/24 h of amoxicillin. Remember not to exceed the adult dose or “max” dose. The physician will now decide how often the child will receive the medication. This is called the individual or single dose, based on 24 hours.
CALCULATE THE INDIVIDUAL DOSE OR SINGLE DOSE (MILLIGRAMS/KILOGRAM/24 HOURS DIVIDED)
The physician will now determine how often the antibiotic will be administered as a single or individual dose. First determine the 24-hour dosage range. Then divide the 24-hour dosage into single doses (the number of times per day the medication is to be given).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


