Critical Care Intravenous Flow Rates
Critical Care Intravenous Flow Rates
LEARNING OBJECTIVES
On completion of the materials provided in this chapter, you will be able to perform computations accurately by mastering the following mathematical concepts:
1 Calculating the IV flow rate of medications in units per hour or international units per hour
2 Calculating the units per hour of medications from the IV flow rate
3 Calculating the IV flow rate of medications in units per kilogram per hour (weight-based heparin)
4 Calculating the IV flow rate of medications in milligrams per minute
5 Calculating the IV flow rate of medications in micrograms per minute
6 Calculating the IV flow rate of medications in micrograms per kilogram per minute
7 Calculating the milligrams per minute of medications from the IV flow rate
8 Calculating the micrograms per minute of medications from the IV flow rate
9 Calculating the micrograms per kilogram per minute of medications from the IV flow rate
![]() Critically ill patients in a hospital often receive special medications that are very potent and therefore need to be monitored closely. Some of these medications, such as regular insulin or heparin, may be ordered as a set amount of the drug measured in units to be infused over a given period. Other drugs used in the critical care setting may be ordered to be infused by amount of drug per kilogram of body weight per minute. These are called titrations. They are based on the manufacturer’s provided recommended dosage and the patient’s body weight measured in kilograms. In most health care institutions, these situations will occur in the emergency department, an intensive care unit, or a step-down unit. It is extremely important to accurately monitor the flow of these medications; therefore an intravenous (IV) machine is required. Because of the nature of these drugs, route of administration, and state of the patient, the importance of accuracy in calculating the drug dosage and IV flow rates cannot be overemphasized. It is truly a matter of life and death.
Critically ill patients in a hospital often receive special medications that are very potent and therefore need to be monitored closely. Some of these medications, such as regular insulin or heparin, may be ordered as a set amount of the drug measured in units to be infused over a given period. Other drugs used in the critical care setting may be ordered to be infused by amount of drug per kilogram of body weight per minute. These are called titrations. They are based on the manufacturer’s provided recommended dosage and the patient’s body weight measured in kilograms. In most health care institutions, these situations will occur in the emergency department, an intensive care unit, or a step-down unit. It is extremely important to accurately monitor the flow of these medications; therefore an intravenous (IV) machine is required. Because of the nature of these drugs, route of administration, and state of the patient, the importance of accuracy in calculating the drug dosage and IV flow rates cannot be overemphasized. It is truly a matter of life and death.
The following sections focus on medications that are ordered by units per hour, international units per hour, micrograms per kilogram per minute (mcg/kg/min), micrograms per minute (mcg/min), and milligrams per minute (mg/min). All the following medications must be delivered with an IV controller or pump for safe administration. Since infusion pumps are set by milliliters per hour (mL/h), the health care provider needs to be familiar with the steps to convert the ordered drug dosage to milliliters per hour.
Facilities that administer medications with a hemodynamic effect usually have IV controllers that allow the health care professional to program medication rates with a decimal. Therefore answers should be rounded to the nearest tenth decimal place.
IV Administration of Medications by Units/Hour or International Units/Hour
EXAMPLE 1: 200 units of regular insulin have been added to 500 mL of 0.9% normal saline (NS). The order states to infuse the regular insulin IV at 10 units/h. The nurse needs to calculate how many milliliters per hour the IV pump should be programmed for.
Using the Ratio-Proportion Method
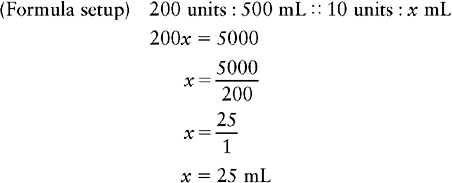
Therefore the nurse will program the IV pump for 25 mL/h to infuse the insulin at 10 units/h.
Using the D A × Q  Method
Method

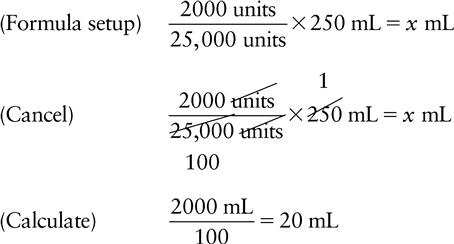
EXAMPLE 2: 25,000 units of heparin have been added to 250 mL of dextrose 5% in water (D5W). The order is to infuse the heparin drip at 2000 units/h. The health care provider needs to calculate how many milliliters per hour to program the IV pump for.
Using the Ratio-Proportion Method
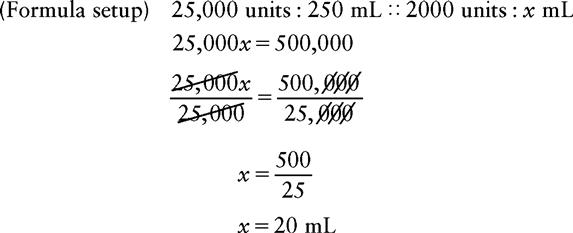
Therefore the nurse will program the IV pump for 20 mL/h to deliver the heparin at 2000 units/h.
Using the D A × Q  Method
Method
Calculating Units/Hour from Milliliter/Hour
EXAMPLE 1: A patient has a continuous insulin drip infusing at 8 mL/h. The insulin concentration is regular insulin 100 units in 200 mL of 0.9% NS. The nurse needs to calculate how many units per hour of insulin the patient is receiving.
Using the Ratio-Proportion Method
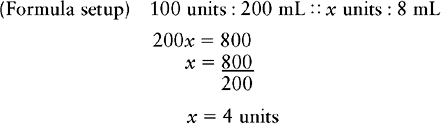
Therefore the patient is receiving 4 units/h of regular insulin.
EXAMPLE 2: A patient has a continuous heparin drip infusing at 14 mL/h. The heparin concentration is heparin 25,000 units/250 mL of 0.9% NS. The nurse needs to calculate how many units per hour of heparin the patient is receiving.
Using the Ratio-Proportion Method
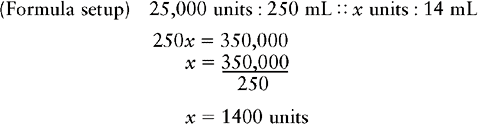
Therefore the patient is receiving 1400 units/h of heparin.
IV ADMINISTRATION OF WEIGHT-BASED HEPARIN
Many facilities order heparin for a patient based on the patient’s weight. The rationale behind this is that a patient who weighs 50 kg requires a different dose of heparin than the patient who weighs 100 kg to achieve a therapeutic dose. Weight-based heparin orders require two calculations: (1) the calculation for the heparin IV bolus and (2) the calculation for the heparin drip in milliliters per hour.
Weight-Based Heparin Protocol (Example)
| PTT Result | Heparin Dosing |
| <35 | Bolus 70 units/kg and increase drip by 4 units/kg/h |
| 35-54 | Bolus 35 units/kg and increase drip by 3 units/kg/h |
| 55-85 | Therapeutic–no change |
| 86-100 | Decrease drip by 2 units/kg/h |
| >100 | Hold infusion 1 hour; decrease drip by 3 units/kg/h, then restart drip |
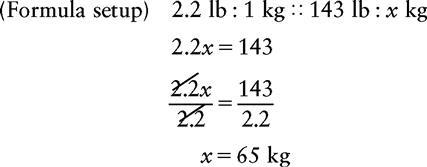
EXAMPLE: The order is to start a heparin infusion using the heparin protocol. The patient’s weight is 143 lb. The nurse needs to do two calculations: the heparin bolus and the rate, in milliliters per hour, at which to program the IV pump.
Bolus
The protocol calls for 70 units/kg, rounded to the nearest hundredth.
a. Convert pounds to kilograms.
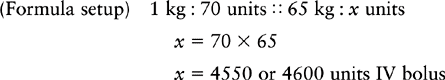
b. Calculate the units required for the IV bolus.
(Formula setup) 1 kg : 70 units :: 65 kg : x units
IV Infusion
The protocol states 17 units/kg/h, rounded to the nearest tenth.
a. Calculate how many units are needed for a patient weighing 65 kg.
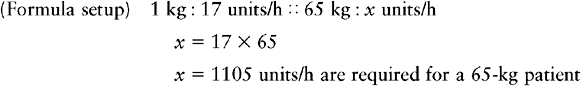
Using the Ratio-Proportion Method
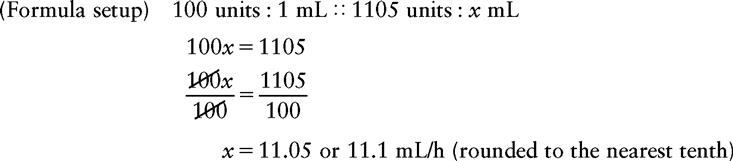
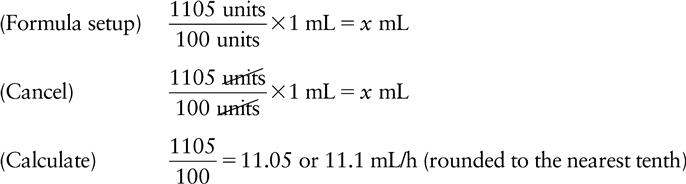
Therefore the nurse will set the IV pump for 11.1 mL/h to infuse the heparin at 17 units/kg/h.
Using D A × Q  Method
Method
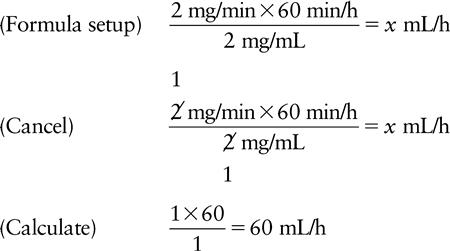
IV Administration of Medications by Milligram/Minute
EXAMPLE: Lidocaine 1 g has been added to 500 mL of D5W. The order states to infuse the lidocaine at 2 mg/min. The nurse needs to calculate the rate, in milliliters per hour, at which to set the IV pump.
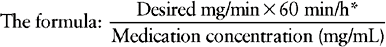
*60 min/h is a constant fraction in the formula and represents the equivalency of 60 min = 1 h.
When this formula is used, the answer will always be expressed in milliliters per hour because the pair of values in milligrams will cancel each other, as will the pair of values in minutes.