CHAPTER 17 Case Studies
INTRODUCTION
The cases presented here illustrate two principles:
Quantitative Acupuncture Evaluation
The principle of QAE is discussed in detail in Chapter 6 and we provide only a summary here.
Quantitative evaluation is based on the following factors:
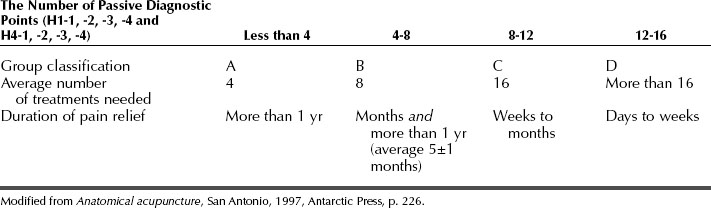
We selected 16 acupoints as evaluation points: palpating 4 points on the deep radial nerve on both arms and 4 points on the saphenous nerve on both legs enables us to divide patients into four groups: A, B, C, and D (Table 17-1).
Standardized but Individualized INMAS Protocol
The INMAS treatment protocol ensures that every patient receives appropriately standardized treatment that is also adjusted to the patient’s personal condition. The INMAS protocol is described in detail in Chapter 5 and we provide only a summary here.
The principles of quantitative evaluation and individualization of the standardized INMAS protocol are depicted in every case presented below. All of these cases involved real patients but their names have been changed to protect their privacy.
NECK AND BACK PAIN
Group A: Excellent Results
Case 2: Lower Back and Neck Pain
AB is fit and healthy and has no previous physical injuries. Quantitative evaluation placed him in group A. Visual examination showed that his left shoulder was higher than his right. Upon palpation, acupoints on the left of the neck and the left shoulder area (H7, H3, H13, and H8) were more tender than acupoints on the right side. Left lumbar acupoints (H14, H15, and H16) were sore upon palpation. The impression was that the pain in the lower back and neck was of an acute nature. The prognosis was that pain relief could be achieved within four treatments.
Treatment Plan
Treatment Plan
The treatments were administered in the prone position. The acupoints selected were:
Group B: Good Results
Treatment Plan
Treatments were administered in the prone position. The selected acupoints were:
Case 7: Lower Back Pain
BG had no previous medical problems. Quantitative evaluation placed him in group B. Upon palpation, his left lumbar muscles were more sensitive than those on the right, and the left lumbar acupoints (H15, H14, H22, and H16) were tender, especially H22. The neck area was healthy, without any tender points. Given the foregoing, treatments were concentrated on the lower back. The back pain was treatable because of its acute nature. The prognosis was that about eight treatments should be enough to reduce the present pain and, given 30-years-worth of lower back stiffness, about four more treatments would be needed to prevent lower back pain in the future. Thus, the prognosis was that initially eight treatments would be necessary.
Treatment Plan
Treatments were administered in the prone position. The acupoints selected were:
Treatment Plan
Treatments were administered in the prone position. The acupoints selected were:
Treatment Plan
Treatments were administered in the prone position. The acupoints selected were:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree