Definition
 1,5-Anhydroglucitol (1,5-AG), sometimes known as GlycoMark, is a monosaccharide that shows a structural similarity to glucose. Its main source in humans is dietary ingestion, particularly meats and cereals. In addition, 10% of 1,5-AG is derived from endogenous synthesis. It is generally not metabolized, and in healthy subjects, it achieves a stable plasma concentration that reflects a steady balance between ingestion and urinary excretion.
1,5-Anhydroglucitol (1,5-AG), sometimes known as GlycoMark, is a monosaccharide that shows a structural similarity to glucose. Its main source in humans is dietary ingestion, particularly meats and cereals. In addition, 10% of 1,5-AG is derived from endogenous synthesis. It is generally not metabolized, and in healthy subjects, it achieves a stable plasma concentration that reflects a steady balance between ingestion and urinary excretion.
 Normal range: 10.7–32.0 μg/mL in males; 6.8–29.3 μg/mL in females.
Normal range: 10.7–32.0 μg/mL in males; 6.8–29.3 μg/mL in females.
 Use
Use
 Used clinically to monitor short-term glycemic control in patients with diabetes (1–2 weeks)
Used clinically to monitor short-term glycemic control in patients with diabetes (1–2 weeks)
 Useful marker for postprandial hyperglycemia
Useful marker for postprandial hyperglycemia
 Performs better than hemoglobin A1C for monitoring glucose profile in pregnancies complicated by type 1 diabetes
Performs better than hemoglobin A1C for monitoring glucose profile in pregnancies complicated by type 1 diabetes
 Interpretation
Interpretation
Increased In
 1,5-AG may be increased during IV hyperalimentation.
1,5-AG may be increased during IV hyperalimentation.
Decreased In
 Individuals with renal glucose thresholds that are markedly different from 180 mg/dL (e.g., chronic renal failure, pregnancy, and dialysis) and in those undergoing steroid therapy.
Individuals with renal glucose thresholds that are markedly different from 180 mg/dL (e.g., chronic renal failure, pregnancy, and dialysis) and in those undergoing steroid therapy.
 α-Glucosidase inhibitors can decrease 1,5-AG by interfering with its intestinal absorption.
α-Glucosidase inhibitors can decrease 1,5-AG by interfering with its intestinal absorption.
 Limitations
Limitations
 In patients with poorly controlled DM, 1,5-AG is less sensitive to modest changes in glycemic control because of continuous glycosuria.
In patients with poorly controlled DM, 1,5-AG is less sensitive to modest changes in glycemic control because of continuous glycosuria.
 Levels can be influenced by factors such as dairy product, races, uric acid, triglycerides, liver disease, gastrectomy state, and cystic fibrosis.
Levels can be influenced by factors such as dairy product, races, uric acid, triglycerides, liver disease, gastrectomy state, and cystic fibrosis.
11-DEOXYCORTISOL
 Definition
Definition
 11-Deoxycortisol, also known as cortodoxone, corticosterone, and compound S, is a steroid and an immediate precursor to the production of cortisol. It can be synthesized from 17-hydroxyprogesterone. Excretion in urine is included in 17-ketogenic steroid (17-KGS) and Porter-Silber 17-OHKS measurements, which were originally used to provide some measure of cortisol production. The direct measurement of cortisol has replaced determinations of 17-KS and 17-OHKS.
11-Deoxycortisol, also known as cortodoxone, corticosterone, and compound S, is a steroid and an immediate precursor to the production of cortisol. It can be synthesized from 17-hydroxyprogesterone. Excretion in urine is included in 17-ketogenic steroid (17-KGS) and Porter-Silber 17-OHKS measurements, which were originally used to provide some measure of cortisol production. The direct measurement of cortisol has replaced determinations of 17-KS and 17-OHKS.
 Normal range: <50 ng/dL in males; <33 ng/dL in females.
Normal range: <50 ng/dL in males; <33 ng/dL in females.
 Use
Use
 Diagnosis of and monitoring therapeutic response in CAH due to 11β-hydroxylase deficiency
Diagnosis of and monitoring therapeutic response in CAH due to 11β-hydroxylase deficiency
 Assessment of adrenal response in the metyrapone test; result after metyrapone stimulation is >8,000 ng/dL
Assessment of adrenal response in the metyrapone test; result after metyrapone stimulation is >8,000 ng/dL
 Interpretation
Interpretation
Increased In
 Values are increased in CAH (P450cII deficiency) and following metyrapone administration in normal persons.
Values are increased in CAH (P450cII deficiency) and following metyrapone administration in normal persons.
Decreased In
 Values are decreased in adrenal insufficiency.
Values are decreased in adrenal insufficiency.
 Limitations
Limitations
 Patients with myxedema, some pregnant patients, and those on oral contraceptives respond poorly during the test.
Patients with myxedema, some pregnant patients, and those on oral contraceptives respond poorly during the test.
17α-HYDROXYPROGESTERONE
 Definition
Definition
 17α-Hydroxyprogesterone, also known as hydroxyprogesterone, is a 21-carbon steroid produced in the adrenals—and also in the ovaries, testes, and placenta—that serves as a biosynthetic precursor to cortisol.
17α-Hydroxyprogesterone, also known as hydroxyprogesterone, is a 21-carbon steroid produced in the adrenals—and also in the ovaries, testes, and placenta—that serves as a biosynthetic precursor to cortisol.
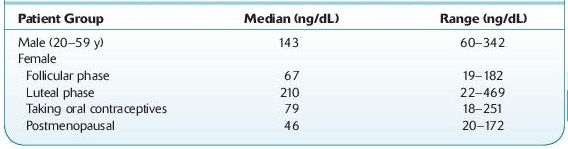
 Normal range: 18–469 ng/dL (see Table 16.1).
Normal range: 18–469 ng/dL (see Table 16.1).
TABLE 16–1. Range of Normal Values for 17a-Hydroxyprogesterone
 Use
Use
 Diagnosis and management of congenital adrenal hyperplasia, hirsutism, and infertility
Diagnosis and management of congenital adrenal hyperplasia, hirsutism, and infertility
 Interpretation
Interpretation
Increased In
 The luteal phase of menstruating women and pregnancy, during which it rises.
The luteal phase of menstruating women and pregnancy, during which it rises.
 When defective 21-alpha hydroxylase and 11-beta hydroxylase are present.
When defective 21-alpha hydroxylase and 11-beta hydroxylase are present.
 The most common form of CAH, where deficiency of the enzyme 21-hydroxylase blocks normal synthesis of cortisol, leading to a compensatory increase of ACTH secretion; this results in increased levels.
The most common form of CAH, where deficiency of the enzyme 21-hydroxylase blocks normal synthesis of cortisol, leading to a compensatory increase of ACTH secretion; this results in increased levels.
 Limitations
Limitations
 Circulating normally exhibits a diurnal pattern similar to that of cortisol, with higher values in the early morning than in the late afternoon. Hence, the time of collection should be standardized.
Circulating normally exhibits a diurnal pattern similar to that of cortisol, with higher values in the early morning than in the late afternoon. Hence, the time of collection should be standardized.
 Spuriously elevated levels are sometimes seen in premature and sick newborns due to interference with other steroid metabolites. 17α-Hydroxypregnenolone sulfate (percent cross-reactivity: 3.8%) has been identified as the most significant interferent in direct assays.
Spuriously elevated levels are sometimes seen in premature and sick newborns due to interference with other steroid metabolites. 17α-Hydroxypregnenolone sulfate (percent cross-reactivity: 3.8%) has been identified as the most significant interferent in direct assays.
 17α-Hydroxyprogesterone values for women with late-onset CAH have been found to overlap with those encountered in hirsute, oligomenorrheic women who do not have the disorder. Accordingly, it is important to determine ACTH-stimulated 17α-hydroxyprogesterone levels in women suspected of having late-onset CAH.
17α-Hydroxyprogesterone values for women with late-onset CAH have been found to overlap with those encountered in hirsute, oligomenorrheic women who do not have the disorder. Accordingly, it is important to determine ACTH-stimulated 17α-hydroxyprogesterone levels in women suspected of having late-onset CAH.
17-KETOSTEROIDS, URINE (17-KS)
 Definition
Definition
 17-Ketosteroids, urine (17-KS), are breakdown products of androgens and are an adrenal function test. Examples of 17-KS include androstenedione, androsterone, estrone, and dehydroepiandrosterone. An alternative and more specific test for adrenal androgen function is dehydroepiandrosterone sulfate in serum.
17-Ketosteroids, urine (17-KS), are breakdown products of androgens and are an adrenal function test. Examples of 17-KS include androstenedione, androsterone, estrone, and dehydroepiandrosterone. An alternative and more specific test for adrenal androgen function is dehydroepiandrosterone sulfate in serum.
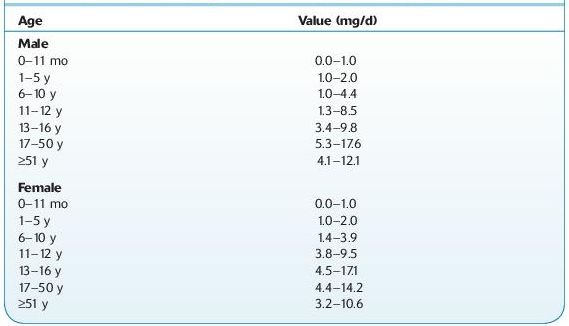
 Normal range: depends on sex and age (Table 16.2).
Normal range: depends on sex and age (Table 16.2).
TABLE 16–2. Normal Ranges for 17-Ketosteroids in the Urine
 Use
Use
 Evaluation of glucocorticoid production and neuroendocrine function
Evaluation of glucocorticoid production and neuroendocrine function
 Evaluation of androgenic adrenal and testicular function in normal male individuals and primarily adrenal androgenic secretion in normal female individuals
Evaluation of androgenic adrenal and testicular function in normal male individuals and primarily adrenal androgenic secretion in normal female individuals
 Interpretation
Interpretation
Increased In
 Adrenal tumor
Adrenal tumor
 Congenital adrenal hyperplasia (very rare)
Congenital adrenal hyperplasia (very rare)
 Cushing syndrome
Cushing syndrome
 Ovarian cancer
Ovarian cancer
 Testicular cancer
Testicular cancer
 Ovarian dysfunction (polycystic ovarian disease)
Ovarian dysfunction (polycystic ovarian disease)
Decreased In
 Addison disease
Addison disease
 Castration
Castration
 Hypopituitarism
Hypopituitarism
 Myxedema
Myxedema
 Nephrosis
Nephrosis
 Limitations
Limitations
 A large number of substances may interfere with this test.
A large number of substances may interfere with this test.
 Decreases may be caused by carbamazepine, cephaloridine, cephalothin, chlormerodrin, digoxin, glucose, metyrapone, promazine, propoxyphene, reserpine, and others.
Decreases may be caused by carbamazepine, cephaloridine, cephalothin, chlormerodrin, digoxin, glucose, metyrapone, promazine, propoxyphene, reserpine, and others.
 Increases may be caused by acetone, acetophenide, ascorbic acid, chloramphenicol, chlorothiazide, chlorpromazine, cloxacillin, dexamethasone, erythromycin, ethinamate, etryptamine, methicillin, methyprylon, morphine, oleandomycin, oxacillin, penicillin, phenaglycodol, phenazopyridine, phenothiazine, piperidine, quinidine, secobarbital, spironolactone, and others.
Increases may be caused by acetone, acetophenide, ascorbic acid, chloramphenicol, chlorothiazide, chlorpromazine, cloxacillin, dexamethasone, erythromycin, ethinamate, etryptamine, methicillin, methyprylon, morphine, oleandomycin, oxacillin, penicillin, phenaglycodol, phenazopyridine, phenothiazine, piperidine, quinidine, secobarbital, spironolactone, and others.
5,10-METHYLENETETRAHYDROFOLATE REDUCTASE (MTHFR) MOLECULAR ASSAY*
 Definition
Definition
 Mutations, C677T and A1298C, in the 5,10-methylenetetrahydrofolate reductase (MTHFR) gene increase the risk of thrombosis (OMIM# 188050) and other cardiovascular disorders as a result of an elevated plasma homocysteine concentration (OMIM# 236250).
Mutations, C677T and A1298C, in the 5,10-methylenetetrahydrofolate reductase (MTHFR) gene increase the risk of thrombosis (OMIM# 188050) and other cardiovascular disorders as a result of an elevated plasma homocysteine concentration (OMIM# 236250).
 Normal values: negative or no mutations are found.
Normal values: negative or no mutations are found.
 Use
Use
 Suspected coronary artery disease, homocystinuria, neural tube defects, spontaneous abortion, or MTHFR deficiency
Suspected coronary artery disease, homocystinuria, neural tube defects, spontaneous abortion, or MTHFR deficiency
 Limitations
Limitations
 The results of a genetic test may be affected by DNA rearrangements, blood transfusion, bone marrow transplantation, or rare sequence variations.
The results of a genetic test may be affected by DNA rearrangements, blood transfusion, bone marrow transplantation, or rare sequence variations.
5-HYDROXYINDOLEACETIC ACID (5-HIAA) URINE
 Definition
Definition
 5-Hydroxyindoleacetic acid (5-HIAA), also known as serotonin metabolite, is the major urinary metabolite of serotonin.
5-Hydroxyindoleacetic acid (5-HIAA), also known as serotonin metabolite, is the major urinary metabolite of serotonin.
 Normal range: 0.0–15.0 mg/day (24-hour urine); 0.0–14.0 mg/g creatinine.
Normal range: 0.0–15.0 mg/day (24-hour urine); 0.0–14.0 mg/g creatinine.
 Use
Use
 Helps diagnose and monitor treatment for serotonin-secreting carcinoid tumors
Helps diagnose and monitor treatment for serotonin-secreting carcinoid tumors
 Interpretation
Interpretation
Increased In
 Whipple disease
Whipple disease
 Nontropical sprue
Nontropical sprue
 Small increases possible in pregnancy, ovulation, and postsurgical stress
Small increases possible in pregnancy, ovulation, and postsurgical stress
 Various food ingestions (e.g., pineapples, kiwi, bananas, eggplant, plums, tomatoes, avocados, plantains, walnuts, pecans, hickory nuts, coffee)
Various food ingestions (e.g., pineapples, kiwi, bananas, eggplant, plums, tomatoes, avocados, plantains, walnuts, pecans, hickory nuts, coffee)
 Use of certain drugs (e.g., acetanilid, acetaminophen, acetophenetidin, caffeine, coumaric acid, diazepam [Valium], ephedrine, fluorouracil, glyceryl guaiacolate [guaifenesin], heparin, melphalan [Alkeran], mephenesin, methamphetamine, methocarbamol, naproxen, nicotine, Lugol solution, promethazine, phenothiazine, hydroxyl tryptophan)
Use of certain drugs (e.g., acetanilid, acetaminophen, acetophenetidin, caffeine, coumaric acid, diazepam [Valium], ephedrine, fluorouracil, glyceryl guaiacolate [guaifenesin], heparin, melphalan [Alkeran], mephenesin, methamphetamine, methocarbamol, naproxen, nicotine, Lugol solution, promethazine, phenothiazine, hydroxyl tryptophan)
Decreased In
 Use of certain drugs (e.g., chlorpromazine, promazine, imipramine, isoniazid, monoamine oxidase inhibitors, methenamine, methyldopa, phenothiazines, promethazine)
Use of certain drugs (e.g., chlorpromazine, promazine, imipramine, isoniazid, monoamine oxidase inhibitors, methenamine, methyldopa, phenothiazines, promethazine)
 Renal insufficiency (possible)
Renal insufficiency (possible)
 Limitations
Limitations
 Foods rich in serotonin and medications, over-the-counter drugs, and herbal remedies that may affect metabolism of serotonin must be avoided at least 72 hours before and during collection of urine for 5-HIAA.
Foods rich in serotonin and medications, over-the-counter drugs, and herbal remedies that may affect metabolism of serotonin must be avoided at least 72 hours before and during collection of urine for 5-HIAA.
 Twenty-four–hour collections are generally recommended, but random collections may be used. Refrigeration is the most important aspect of specimen preservation.
Twenty-four–hour collections are generally recommended, but random collections may be used. Refrigeration is the most important aspect of specimen preservation.
 Urinary 5-HIAA is increased with malabsorption, in 75% of cases, usually when a carcinoid tumor is far advanced (with large liver metastases, often 300–1,000 mg/day), but may not be increased despite massive metastases.
Urinary 5-HIAA is increased with malabsorption, in 75% of cases, usually when a carcinoid tumor is far advanced (with large liver metastases, often 300–1,000 mg/day), but may not be increased despite massive metastases.
 Sensitivity is 73%.
Sensitivity is 73%.
 The test is useful in the diagnosis of only 5–7% of patients with carcinoid tumors but in approximately 45% of those with liver metastases.
The test is useful in the diagnosis of only 5–7% of patients with carcinoid tumors but in approximately 45% of those with liver metastases.
 Disease extent and prognosis correlate generally with urine 5-HIAA excretion, and the level becomes normal after successful surgery. If urine HIAA is normal, the blood level of serotonin or a precursor, 5-hydroxytryptophan should be checked.
Disease extent and prognosis correlate generally with urine 5-HIAA excretion, and the level becomes normal after successful surgery. If urine HIAA is normal, the blood level of serotonin or a precursor, 5-hydroxytryptophan should be checked.
5′-NUCLEOTIDASE (5¢-RIBONUCLEOTIDEPHOSPHOHYDROLASE, 5′-NT)
 Definition
Definition
 This membrane-bound enzyme of the liver is increased in diseases of the liver, particularly if the hepatobiliary tract is involved. The appearance of 5′-NT in serum is due to cholestasis, and its significance is similar to that of ALP and GGT. However, 5′-NT is not as subject to drug induction as GGT and ALP, and it is not subject to confusion with alternate sources of the enzyme, as is seen with ALP.
This membrane-bound enzyme of the liver is increased in diseases of the liver, particularly if the hepatobiliary tract is involved. The appearance of 5′-NT in serum is due to cholestasis, and its significance is similar to that of ALP and GGT. However, 5′-NT is not as subject to drug induction as GGT and ALP, and it is not subject to confusion with alternate sources of the enzyme, as is seen with ALP.
 Normal range: 2.0–8.0 U/L.
Normal range: 2.0–8.0 U/L.
 Use
Use
 Determining cholestatic liver disease, particularly when GGT and ALP could be falsely elevated due to drug induction
Determining cholestatic liver disease, particularly when GGT and ALP could be falsely elevated due to drug induction
 Better test for secondary tumors and lymphomas of the liver than ALP
Better test for secondary tumors and lymphomas of the liver than ALP
 Interpretation
Interpretation
Increased In
 5′-NT is increased in the following conditions:
5′-NT is increased in the following conditions:
 Hepatobiliary disease with intrahepatic or extrahepatic biliary obstruction
Hepatobiliary disease with intrahepatic or extrahepatic biliary obstruction
 Hepatic carcinoma
Hepatic carcinoma
 Early biliary cirrhosis
Early biliary cirrhosis
 Pregnancy (third semester)
Pregnancy (third semester)
 Inflammatory arthritis
Inflammatory arthritis
 Limitations
Limitations
 5′-NT can be elevated in hyperammonemia due to analytical interference.
5′-NT can be elevated in hyperammonemia due to analytical interference.
 Normal in pregnancy and postpartum period (in contrast to serum leucine aminopeptidase and ALP).
Normal in pregnancy and postpartum period (in contrast to serum leucine aminopeptidase and ALP).
ACETAMINOPHEN (N-ACETYL-p-AMINOPHENOL; APAP)
 Definition
Definition
 Nonopioid analgesic, antipyretic
Nonopioid analgesic, antipyretic
 Use
Use
 Relief of pain, such as headaches and toothaches
Relief of pain, such as headaches and toothaches
 Reduction of fever
Reduction of fever
 Interpretation
Interpretation
 Screen of urine: indication of exposure
Screen of urine: indication of exposure
 Screen of serum: used to assess potential toxicity
Screen of serum: used to assess potential toxicity
 Normal range: 5–20 μg/mL serum
Normal range: 5–20 μg/mL serum
 Potentially toxic: >150 μg/mL measured 4 hours postdose
Potentially toxic: >150 μg/mL measured 4 hours postdose
 Limitations
Limitations
 Screening
Screening
 Serum/urine: colorimetric or immunoassay on automated chemistry analyzers
Serum/urine: colorimetric or immunoassay on automated chemistry analyzers
 High bilirubin concentrations [>50 μg/mL] may cause false-positive results with immunoassay-based tests.
High bilirubin concentrations [>50 μg/mL] may cause false-positive results with immunoassay-based tests.
 Plasma may be tested in place of serum. Anticoagulants such as EDTA and heparin do not generally interfere with the assay.
Plasma may be tested in place of serum. Anticoagulants such as EDTA and heparin do not generally interfere with the assay.
 Do not use whole blood.
Do not use whole blood.
 Confirmation:
Confirmation:
 Serum/urine–HPLC or GC/MC
Serum/urine–HPLC or GC/MC
 APAP is highly conjugated by glucuronidation and sulfation.
APAP is highly conjugated by glucuronidation and sulfation.
 An assay that includes a hydrolysis step provides total APAP levels, which are not useful for assessing toxicity.
An assay that includes a hydrolysis step provides total APAP levels, which are not useful for assessing toxicity.
ACETYLSALICYLIC ACID
See Salicylates (Aspirin).
ACID PHOSPHATASE
 Definition
Definition
 Acid phosphatase is a hydrolytic enzyme secreted by various cells, and it has five isoenzymes. The greatest amount per gram of tissue is found in semen (prostate); it is also detectable in bone, liver, spleen, kidney, RBCs, and platelets. The acid phosphatase test is also known as prostatic acid phosphatase (PAP), the serum acid phosphatase test, and the tartrate-resistant acid phosphatase (TRAP) test.
Acid phosphatase is a hydrolytic enzyme secreted by various cells, and it has five isoenzymes. The greatest amount per gram of tissue is found in semen (prostate); it is also detectable in bone, liver, spleen, kidney, RBCs, and platelets. The acid phosphatase test is also known as prostatic acid phosphatase (PAP), the serum acid phosphatase test, and the tartrate-resistant acid phosphatase (TRAP) test.
 Normal range: 0–0.8 U/L.
Normal range: 0–0.8 U/L.
 Use
Use
 Predicts recurrence after radical prostatectomy for clinically localized prostate cancer and following response to androgen ablation therapy, when used in conjunction with PSA
Predicts recurrence after radical prostatectomy for clinically localized prostate cancer and following response to androgen ablation therapy, when used in conjunction with PSA
 Interpretation
Interpretation
Increased In
 Acid phosphatase is increased in the following conditions:
Acid phosphatase is increased in the following conditions:
 Prostate cancer
Prostate cancer
 Gaucher disease and Niemann-Pick disease
Gaucher disease and Niemann-Pick disease
 One day to 2 days after prostatic surgery or biopsy
One day to 2 days after prostatic surgery or biopsy
 Prostatic manipulation or catheterization
Prostatic manipulation or catheterization
 Benign prostatic hyperplasia, prostatitis, prostate infarct
Benign prostatic hyperplasia, prostatitis, prostate infarct
 Vaginal swabs from rape victims.
Vaginal swabs from rape victims.
 Limitations
Limitations
 PAP is no longer used to screen for or to stage prostate cancer. In most instances, serum PSA is used instead.
PAP is no longer used to screen for or to stage prostate cancer. In most instances, serum PSA is used instead.
 PAP measurement must not be regarded as an absolute test for malignancy, since other factors including benign prostatic hyperplasia, prostatic infarction, and manipulation of the prostate gland may result in elevated serum PAP concentrations.
PAP measurement must not be regarded as an absolute test for malignancy, since other factors including benign prostatic hyperplasia, prostatic infarction, and manipulation of the prostate gland may result in elevated serum PAP concentrations.
 PAP measurements provide little additional information beyond that provided by PSA measurements.
PAP measurements provide little additional information beyond that provided by PSA measurements.
Suggested Reading
Moul JW, Connelly RR, Perahia B, et al. The contemporary value of pretreatment prostatic acid phosphatase to predict pathological stage and recurrence in radical prostatectomy cases. J Urol. 1998;159:935–940.
ACTH STIMULATION (COSYNTROPIN) TEST
 Definition
Definition
 Cosyntropin is synthetic ACTH (1–24), which has the full biologic potency of native ACTH (1–39). It is a rapid stimulator of cortisol and aldosterone secretion.
Cosyntropin is synthetic ACTH (1–24), which has the full biologic potency of native ACTH (1–39). It is a rapid stimulator of cortisol and aldosterone secretion.
 Use
Use
 This is the initial test used to distinguish primary from secondary adrenal insufficiency.
This is the initial test used to distinguish primary from secondary adrenal insufficiency.
 It is not helpful in the diagnosis of Cushing syndrome. Several protocols are used to assess the response to exogenous ACTH administration (see below).
It is not helpful in the diagnosis of Cushing syndrome. Several protocols are used to assess the response to exogenous ACTH administration (see below).
Low-Dose ACTH Stimulation Test
 This test involves physiologic plasma concentrations of ACTH and provides a more sensitive index of adrenocortical responsiveness.
This test involves physiologic plasma concentrations of ACTH and provides a more sensitive index of adrenocortical responsiveness.
 It is performed by measuring serum cortisol immediately before and 30 minutes after IV injection of cosyntropin in a dose of either 1 μg/1.73 m2 or 0.5 μg/1.73 m2.
It is performed by measuring serum cortisol immediately before and 30 minutes after IV injection of cosyntropin in a dose of either 1 μg/1.73 m2 or 0.5 μg/1.73 m2.
 There is no commercially available preparation of “low-dose” cosyntropin. The vials of cosyntropin currently available contain 250 μg and come with sterile normal saline to be used as a diluent. One prepares the low-dose solution of cosyntropin locally.
There is no commercially available preparation of “low-dose” cosyntropin. The vials of cosyntropin currently available contain 250 μg and come with sterile normal saline to be used as a diluent. One prepares the low-dose solution of cosyntropin locally.
High-Dose ACTH Stimulation Test
 This test consists of measuring serum cortisol immediately before and 30 and 60 minutes after IV injection of 250 μg of cosyntropin. This dose of cosyntropin results in pharmacologic plasma ACTH concentrations for the 60-minute duration of the test.
This test consists of measuring serum cortisol immediately before and 30 and 60 minutes after IV injection of 250 μg of cosyntropin. This dose of cosyntropin results in pharmacologic plasma ACTH concentrations for the 60-minute duration of the test.
 The advantage of the high-dose test is that the cosyntropin can be injected using the IM route, because pharmacologic plasma ACTH concentrations are still achieved.
The advantage of the high-dose test is that the cosyntropin can be injected using the IM route, because pharmacologic plasma ACTH concentrations are still achieved.
 Salivary cortisol can also be measured during this test. Salivary cortisol increases to 19 ± 0.8 ng/mL (range: 8.7–36 ng/mL) 1 hour after injection.
Salivary cortisol can also be measured during this test. Salivary cortisol increases to 19 ± 0.8 ng/mL (range: 8.7–36 ng/mL) 1 hour after injection.
Eight-Hour ACTH Stimulation Test
 The 8-hour test, which is now rarely performed, consists of infusing 250 μg of cosyntropin continuously over 8 hours in 500 mL of isotonic saline. A 24-hour urine specimen is collected the day before and the day of the infusion for cortisol or 17-hydroxycorticoid and creatinine determination, and serum cortisol is determined at the end of the infusion. Plasma ACTH concentrations are supraphysiologic throughout the infusion.
The 8-hour test, which is now rarely performed, consists of infusing 250 μg of cosyntropin continuously over 8 hours in 500 mL of isotonic saline. A 24-hour urine specimen is collected the day before and the day of the infusion for cortisol or 17-hydroxycorticoid and creatinine determination, and serum cortisol is determined at the end of the infusion. Plasma ACTH concentrations are supraphysiologic throughout the infusion.
 The 24-hour urinary excretion of 17-hydroxycorticoid should increase three-to fivefold over baseline on the day of ACTH infusion.
The 24-hour urinary excretion of 17-hydroxycorticoid should increase three-to fivefold over baseline on the day of ACTH infusion.
Two-Day ACTH Infusion Test
 The 2-day ACTH infusion test is similar to the 8-hour infusion test, except that the same dose of ACTH is infused for 8 hours on 2 consecutive days.
The 2-day ACTH infusion test is similar to the 8-hour infusion test, except that the same dose of ACTH is infused for 8 hours on 2 consecutive days.
 This test may be helpful in distinguishing secondary from tertiary adrenal insufficiency. The 1-day 8-hour test is too short for this purpose, whereas longer tests add little further useful information.
This test may be helpful in distinguishing secondary from tertiary adrenal insufficiency. The 1-day 8-hour test is too short for this purpose, whereas longer tests add little further useful information.
 Urinary excretion of 17-hydroxycorticoid should exceed 27 mg during the first 24 hours of infusion and 47 mg during the second 48 hours.
Urinary excretion of 17-hydroxycorticoid should exceed 27 mg during the first 24 hours of infusion and 47 mg during the second 48 hours.
 Interpretation
Interpretation
 Low-dose stimulation test: A value of 18 μg/dL or more, before or after ACTH injection, is indicative of normal adrenal function.
Low-dose stimulation test: A value of 18 μg/dL or more, before or after ACTH injection, is indicative of normal adrenal function.
 High-dose stimulation test: A serum cortisol value of 20 μg/dL or more at any time during the test, including before injection, is indicative of normal adrenal function.
High-dose stimulation test: A serum cortisol value of 20 μg/dL or more at any time during the test, including before injection, is indicative of normal adrenal function.
 Eight-hour stimulation test: Serum cortisol should reach 20 μg/dL in 30–60 minutes after the infusion is begun and exceed 25 μg/mL after 6–8 hours.
Eight-hour stimulation test: Serum cortisol should reach 20 μg/dL in 30–60 minutes after the infusion is begun and exceed 25 μg/mL after 6–8 hours.
 Two-day infusion test: Serum cortisol should reach 20 μg/mL in 30–60 minutes after the ACTH infusion is begun and exceed 25 μg/mL after 6–8 hours. Both serum and urinary steroid values increase progressively thereafter, but the ranges of normal are not well defined.
Two-day infusion test: Serum cortisol should reach 20 μg/mL in 30–60 minutes after the ACTH infusion is begun and exceed 25 μg/mL after 6–8 hours. Both serum and urinary steroid values increase progressively thereafter, but the ranges of normal are not well defined.
 Limitations
Limitations
 In healthy individuals, cortisol responses are greatest in the morning, but in patients with adrenal insufficiency, the response to cosyntropin is the same in the morning and afternoon. Therefore, ACTH stimulation tests should be done in the morning to minimize the risk of misdiagnosis in a normal individual.
In healthy individuals, cortisol responses are greatest in the morning, but in patients with adrenal insufficiency, the response to cosyntropin is the same in the morning and afternoon. Therefore, ACTH stimulation tests should be done in the morning to minimize the risk of misdiagnosis in a normal individual.
 The criteria for a minimal normal cortisol response of 18–20 μg/dL are derived from the responses of healthy volunteers. However, in some studies, higher cutoff points for the diagnosis of adrenal insufficiency are based on the ACTH test responses of patients known to have an abnormal response to insulin.
The criteria for a minimal normal cortisol response of 18–20 μg/dL are derived from the responses of healthy volunteers. However, in some studies, higher cutoff points for the diagnosis of adrenal insufficiency are based on the ACTH test responses of patients known to have an abnormal response to insulin.
 Variability in cortisol assays creates an additional problem with setting criteria for a normal response to ACTH that apply to all centers. Studies comparing cortisol results obtained with different assays showed a positive bias of Radioimmunoassays (RIA) and EIAs of 10–50% compared to a reference value obtained using isotope dilution GC/MS.
Variability in cortisol assays creates an additional problem with setting criteria for a normal response to ACTH that apply to all centers. Studies comparing cortisol results obtained with different assays showed a positive bias of Radioimmunoassays (RIA) and EIAs of 10–50% compared to a reference value obtained using isotope dilution GC/MS.
 In women, the response to ACTH is affected by the use of oral contraceptives, which increase cortisol-binding globulin levels.
In women, the response to ACTH is affected by the use of oral contraceptives, which increase cortisol-binding globulin levels.
 The response to ACTH varies with the underlying disorder. If the patient has hypopituitarism with deficient ACTH secretion and secondary adrenal insufficiency, then the intrinsically normal adrenal gland should respond to maximally stimulating concentrations of exogenous ACTH if given for a sufficiently long time. The response may be less than that in normal subjects and initially sluggish due to adrenal atrophy resulting from chronically low stimulation by endogenous ACTH. If, on the other hand, the patient has primary adrenal insufficiency, endogenous ACTH secretion is already elevated, and there should be little or no adrenal response to exogenous ACTH.
The response to ACTH varies with the underlying disorder. If the patient has hypopituitarism with deficient ACTH secretion and secondary adrenal insufficiency, then the intrinsically normal adrenal gland should respond to maximally stimulating concentrations of exogenous ACTH if given for a sufficiently long time. The response may be less than that in normal subjects and initially sluggish due to adrenal atrophy resulting from chronically low stimulation by endogenous ACTH. If, on the other hand, the patient has primary adrenal insufficiency, endogenous ACTH secretion is already elevated, and there should be little or no adrenal response to exogenous ACTH.
 A clearly subnormal response to the low-dose or high-dose ACTH stimulation test is diagnostic of primary or secondary adrenal insufficiency, whereas a normal response excludes both disorders.
A clearly subnormal response to the low-dose or high-dose ACTH stimulation test is diagnostic of primary or secondary adrenal insufficiency, whereas a normal response excludes both disorders.
 Cortisol values between 18.0 and 25.4 μg/dL represent a range of uncertainty in which patients may have discordant responses to ACTH, insulin, and/or metyrapone. Higher concentrations represent a normal response in the non-ICU setting.
Cortisol values between 18.0 and 25.4 μg/dL represent a range of uncertainty in which patients may have discordant responses to ACTH, insulin, and/or metyrapone. Higher concentrations represent a normal response in the non-ICU setting.
 The low-dose test is not valid if there has been recent pituitary injury, and it supports the conclusion that a 30-minute serum cortisol concentration <18 μg/dL indicates impaired adrenocortical reserve. In addition, the low-dose test does not reliably indicate hypothalamic–pituitary–adrenal axis suppression in preterm infants whose mothers received dexamethasone for <2 weeks before delivery to hasten fetal lung development. The CRH test should be used in this situation.
The low-dose test is not valid if there has been recent pituitary injury, and it supports the conclusion that a 30-minute serum cortisol concentration <18 μg/dL indicates impaired adrenocortical reserve. In addition, the low-dose test does not reliably indicate hypothalamic–pituitary–adrenal axis suppression in preterm infants whose mothers received dexamethasone for <2 weeks before delivery to hasten fetal lung development. The CRH test should be used in this situation.
ACTIVATED CLOTTING TIME (ACT)*
 Definition
Definition
 Activated clotting time (ACT) is a rapid point-of-care standardized clotting time, performed by automated well-calibrated instruments, such as the Medtronic automated coagulation timer (ACT). A baseline ACT has to be established in each POCT area after induction of anesthesia and opening the chest for cardiopulmonary bypass surgery, because surgery and anesthesia shorten it. The ACT may also vary slightly with the lot number of the control cartridge.
Activated clotting time (ACT) is a rapid point-of-care standardized clotting time, performed by automated well-calibrated instruments, such as the Medtronic automated coagulation timer (ACT). A baseline ACT has to be established in each POCT area after induction of anesthesia and opening the chest for cardiopulmonary bypass surgery, because surgery and anesthesia shorten it. The ACT may also vary slightly with the lot number of the control cartridge.
 Normal range in the absence of heparin (with Medtronic coagulometer): 74–125 seconds.
Normal range in the absence of heparin (with Medtronic coagulometer): 74–125 seconds.
 Use
Use
 ACT is the most widely used measure of anticoagulation with heparin (and neutralization of heparin with protamine) during extracorporeal circulation. After the initial dose of heparin, the ACT is maintained at >275 seconds for off-pump coronary procedures and >350 seconds for on-pump procedures by periodic administration of heparin.
ACT is the most widely used measure of anticoagulation with heparin (and neutralization of heparin with protamine) during extracorporeal circulation. After the initial dose of heparin, the ACT is maintained at >275 seconds for off-pump coronary procedures and >350 seconds for on-pump procedures by periodic administration of heparin.
 Interpretation
Interpretation
 There is some controversy concerning whether monitoring heparinization by ACT alone ensures optimal heparin and protamine doses. A poor correlation was found between ACT and heparin measurements using anti-Xa assays. Nevertheless, experience has shown that institution of anticoagulation and monitoring under ACT guidance and reversal improves hemostasis, limits blood loss, and reduces the need for transfusions.
There is some controversy concerning whether monitoring heparinization by ACT alone ensures optimal heparin and protamine doses. A poor correlation was found between ACT and heparin measurements using anti-Xa assays. Nevertheless, experience has shown that institution of anticoagulation and monitoring under ACT guidance and reversal improves hemostasis, limits blood loss, and reduces the need for transfusions.
 Limitations
Limitations
 The response of ACT to heparin varies from individual to individual and with heparin potency.
The response of ACT to heparin varies from individual to individual and with heparin potency.
 Underlying coagulopathies (antithrombin III deficiency, clotting factor deficiencies, DIC) must be excluded.
Underlying coagulopathies (antithrombin III deficiency, clotting factor deficiencies, DIC) must be excluded.
 Medications that inhibit platelet function (aspirin, NSAIDs) may affect ACT.
Medications that inhibit platelet function (aspirin, NSAIDs) may affect ACT.
 Preanalytical errors (sample dilution or contamination with heparin, blood activation) must be avoided. It is particularly important to avoid the use of blood samples contaminated by heparin flushes.
Preanalytical errors (sample dilution or contamination with heparin, blood activation) must be avoided. It is particularly important to avoid the use of blood samples contaminated by heparin flushes.
ACTIVATED PROTEIN C RESISTANCE (APCR)*
 Definition
Definition
 APCR reflects resistance to proteolysis of activated factor V by activated protein C (APC). Ninety-five percent of APCR cases are due to factor V Leiden, a genetic mutation in factor V that predisposes to venous thromboembolism (5–10 times greater risk in heterozygotes and 50–100 times greater risk in homozygote carriers). The remaining 5% are found in pregnancy, malignancy, and the antiphospholipid antibody syndrome. Ratios are generated either from a modified PTT or, more recently, by activating protein C with southern copperhead venom, using dilute Russell viper venom as the clotting reagent. The test is performed in the presence of added APC, where in normal individuals, there is an elongation due to delayed generation of fibrin when factor V is lysed; in the absence of APC, where factor V remains intact, there is no elongation. Patients with APCR have a lesser prolongation of clotting in the presence of APC than controls.
APCR reflects resistance to proteolysis of activated factor V by activated protein C (APC). Ninety-five percent of APCR cases are due to factor V Leiden, a genetic mutation in factor V that predisposes to venous thromboembolism (5–10 times greater risk in heterozygotes and 50–100 times greater risk in homozygote carriers). The remaining 5% are found in pregnancy, malignancy, and the antiphospholipid antibody syndrome. Ratios are generated either from a modified PTT or, more recently, by activating protein C with southern copperhead venom, using dilute Russell viper venom as the clotting reagent. The test is performed in the presence of added APC, where in normal individuals, there is an elongation due to delayed generation of fibrin when factor V is lysed; in the absence of APC, where factor V remains intact, there is no elongation. Patients with APCR have a lesser prolongation of clotting in the presence of APC than controls.
 Normal value: >1.8.
Normal value: >1.8.
 Use
Use
 APCR is one of the assays recommended to investigate the etiology of venous thrombophilia. The congenital form, factor V Leiden, is present in 5% of individuals of European descent and in a high proportion of patients with unprovoked venous thromboembolism. It is virtually absent in patients of pure African ancestry.
APCR is one of the assays recommended to investigate the etiology of venous thrombophilia. The congenital form, factor V Leiden, is present in 5% of individuals of European descent and in a high proportion of patients with unprovoked venous thromboembolism. It is virtually absent in patients of pure African ancestry.
 Limitations
Limitations
 Protein C levels <50% and initial anticoagulation with vitamin K antagonists may give falsely low ratios. In these situations, the genetic test for factor V Leiden is recommended. The APCR assay is valid in patients stabilized on vitamin K antagonists or heparin.
Protein C levels <50% and initial anticoagulation with vitamin K antagonists may give falsely low ratios. In these situations, the genetic test for factor V Leiden is recommended. The APCR assay is valid in patients stabilized on vitamin K antagonists or heparin.
 The assay is invalid in clotted specimens, as well as in lipemic, hemolyzed, or icteric samples. The assay is also invalid if blood is drawn with the wrong anticoagulant or the tubes are not filled appropriately.
The assay is invalid in clotted specimens, as well as in lipemic, hemolyzed, or icteric samples. The assay is also invalid if blood is drawn with the wrong anticoagulant or the tubes are not filled appropriately.
ADIPONECTIN
 Definition
Definition
 Adiponectin, a hormone secreted exclusively by adipose tissue, has an important role in the regulation of tissue inflammation and insulin sensitivity. Perturbations in adiponectin concentration have been associated with obesity and the metabolic syndrome. Levels of the hormone are inversely correlated with body fat percentage in adults, whereas the association in infants and young children is more unclear.
Adiponectin, a hormone secreted exclusively by adipose tissue, has an important role in the regulation of tissue inflammation and insulin sensitivity. Perturbations in adiponectin concentration have been associated with obesity and the metabolic syndrome. Levels of the hormone are inversely correlated with body fat percentage in adults, whereas the association in infants and young children is more unclear.
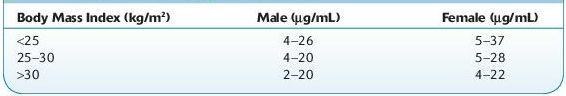
 Normal range: see Table 16.3.
Normal range: see Table 16.3.
TABLE 16–3. Normal Range of Adiponectin
 Use
Use
 Higher adiponectin levels are associated with a lower risk of type 2 diabetes across diverse populations, consistent with a dose–response relationship.
Higher adiponectin levels are associated with a lower risk of type 2 diabetes across diverse populations, consistent with a dose–response relationship.
 Interpretation
Interpretation
Increased In
 Twofold before a meal and decreases to trough levels within 1 hour after eating
Twofold before a meal and decreases to trough levels within 1 hour after eating
 More than twofold in hemodialysis patients
More than twofold in hemodialysis patients
Decreased In
 Type 2 diabetes mellitus
Type 2 diabetes mellitus
 Obesity and metabolic syndrome
Obesity and metabolic syndrome
 Limitations
Limitations
 Adiponectin exerts some of its weight reduction effects via the brain. This is similar to the action of leptin, but the two hormones perform complementary actions and can have additive effects.
Adiponectin exerts some of its weight reduction effects via the brain. This is similar to the action of leptin, but the two hormones perform complementary actions and can have additive effects.
 Due to its important cardiometabolic actions, adiponectin represents a biologic molecule worth being studied as a new emerging biomarker of disease and also as a target for pharmacologic treatments.
Due to its important cardiometabolic actions, adiponectin represents a biologic molecule worth being studied as a new emerging biomarker of disease and also as a target for pharmacologic treatments.
Suggested Reading
Li S, Shin HJ, Ding EL, et al. Adiponectin levels and risk of type 2 diabetes: a systematic review and meta-analysis. JAMA. 2009;302(2):179–188.
ADRENOCORTICOTROPIC HORMONE (ACTH)
 Definition
Definition
 ACTH is a polypeptide hormone produced by the anterior pituitary gland that exists principally as a chain of 39 amino acids, with a molecular mass of approximately 4,500 Da. Its biologic function is to stimulate cortisol secretion by the adrenal cortex. ACTH secretion is in turn controlled by the hypothalamic hormone CRF and by negative feedback from cortisol.
ACTH is a polypeptide hormone produced by the anterior pituitary gland that exists principally as a chain of 39 amino acids, with a molecular mass of approximately 4,500 Da. Its biologic function is to stimulate cortisol secretion by the adrenal cortex. ACTH secretion is in turn controlled by the hypothalamic hormone CRF and by negative feedback from cortisol.
 Normal range: <46 pg/mL.
Normal range: <46 pg/mL.
 Use
Use
 Diagnosis of Addison disease, CAH, Cushing syndrome, adrenal carcinoma, and ectopic ACTH syndrome
Diagnosis of Addison disease, CAH, Cushing syndrome, adrenal carcinoma, and ectopic ACTH syndrome
 Interpretation
Interpretation
Increased In
 Addison disease
Addison disease
 CAH
CAH
 Pituitary-dependent Cushing disease
Pituitary-dependent Cushing disease
 Ectopic ACTH–producing tumors
Ectopic ACTH–producing tumors
 Nelson syndrome
Nelson syndrome
Decreased In
 Secondary adrenocortical insufficiency
Secondary adrenocortical insufficiency
 Adrenal carcinoma
Adrenal carcinoma
 Adenoma
Adenoma
 Hypopituitarism
Hypopituitarism
 Limitations
Limitations
 Plasma levels of ACTH exhibit a significant diurnal variation. ACTH is normally highest in the early morning (6–8 AM) and lowest in the evening (6–11 PM). Cortisol levels are frequently measured at the same time as ACTH.
Plasma levels of ACTH exhibit a significant diurnal variation. ACTH is normally highest in the early morning (6–8 AM) and lowest in the evening (6–11 PM). Cortisol levels are frequently measured at the same time as ACTH.
 Because ACTH is released in bursts, its levels in the blood can vary from minute to minute.
Because ACTH is released in bursts, its levels in the blood can vary from minute to minute.
 ACTH is unstable in blood, and proper handling of specimen is important.
ACTH is unstable in blood, and proper handling of specimen is important.
 Most commercial RIAs are insensitive and nonspecific, measuring intact ACTH as well as precursors and fragments. Highly sensitive IRMAs measure intact ACTH only.
Most commercial RIAs are insensitive and nonspecific, measuring intact ACTH as well as precursors and fragments. Highly sensitive IRMAs measure intact ACTH only.
 RIAs are recommended for investigating ectopic ACTH–producing tumors, because some of the tumors secrete ACTH precursors and fragments. IRMAs are more sensitive than RIAs and are useful for investigating disorders of the hypothalamic–pituitary–adrenal system.
RIAs are recommended for investigating ectopic ACTH–producing tumors, because some of the tumors secrete ACTH precursors and fragments. IRMAs are more sensitive than RIAs and are useful for investigating disorders of the hypothalamic–pituitary–adrenal system.
 Patients taking glucocorticoids may have suppressed levels of ACTH with an apparent high level of cortisol.
Patients taking glucocorticoids may have suppressed levels of ACTH with an apparent high level of cortisol.
 Pregnancy, menstruation, and stress increase secretion.
Pregnancy, menstruation, and stress increase secretion.
ALLERGEN TESTS, SPECIFIC IMMUNOGLOBULIN E (IgE)
 Definition
Definition
 Allergic diseases are manifested as hyperresponsiveness in the target organ, whether the skin, nose, lung, or GI tract. Most tests for “allergy” are actually tests for allergic sensitization, or the presence of allergen-specific IgE.
Allergic diseases are manifested as hyperresponsiveness in the target organ, whether the skin, nose, lung, or GI tract. Most tests for “allergy” are actually tests for allergic sensitization, or the presence of allergen-specific IgE.
 Most patients who experience symptoms upon exposure to an allergen have demonstrable IgE that specifically recognizes that allergen, making these tests essential tools in the diagnosis of allergic disorders.
Most patients who experience symptoms upon exposure to an allergen have demonstrable IgE that specifically recognizes that allergen, making these tests essential tools in the diagnosis of allergic disorders.
 In vitro testing for allergy has certain advantages:
In vitro testing for allergy has certain advantages:
 It poses no risk to the patient of an allergic reaction.
It poses no risk to the patient of an allergic reaction.
 It is not affected by medications (antihistamines, etc.) the patient may be taking.
It is not affected by medications (antihistamines, etc.) the patient may be taking.
 It is not reliant upon skin integrity or affected by skin disease.
It is not reliant upon skin integrity or affected by skin disease.
 It can be more convenient for the patient. In vitro testing requires submitting a blood sample and does not necessitate a separate visit for skin testing.
It can be more convenient for the patient. In vitro testing requires submitting a blood sample and does not necessitate a separate visit for skin testing.
 Clinical performance of specific IgE-based serum allergen tests typically has sensitivity ranging from 84% to 95% and specificity ranging from 85% to 94%.
Clinical performance of specific IgE-based serum allergen tests typically has sensitivity ranging from 84% to 95% and specificity ranging from 85% to 94%.
 Various types of specific panels, mixes, as well as specific allergen tests currently performed at various labs and contact your lab for details.
Various types of specific panels, mixes, as well as specific allergen tests currently performed at various labs and contact your lab for details.
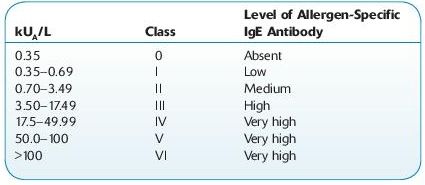
Normal range:
 Use
Use
 To establish the diagnosis of an allergic disease and to define the allergens responsible for eliciting signs and symptoms
To establish the diagnosis of an allergic disease and to define the allergens responsible for eliciting signs and symptoms
 To identify allergens that may be responsible for allergic disease and/or anaphylactic episode and to confirm sensitization to particular allergens prior to beginning immunotherapy
To identify allergens that may be responsible for allergic disease and/or anaphylactic episode and to confirm sensitization to particular allergens prior to beginning immunotherapy
 To investigate the specificity of allergic reactions to insect venom allergens, drugs, or chemical allergens
To investigate the specificity of allergic reactions to insect venom allergens, drugs, or chemical allergens
 Interpretation
Interpretation
Increased In
 Detection of IgE antibodies in serum (Class 1 or greater) indicates an increased likelihood of allergic disease as opposed to other etiologies and defines the allergens that may be responsible for eliciting signs and symptoms.
Detection of IgE antibodies in serum (Class 1 or greater) indicates an increased likelihood of allergic disease as opposed to other etiologies and defines the allergens that may be responsible for eliciting signs and symptoms.
Decreased In
 NA.
NA.
 Limitations
Limitations
 The demonstration of sensitization is not sufficient to diagnose an allergy, however, because a sensitized individual may be entirely asymptomatic upon exposure to the allergen in question. Thus, allergy tests must be interpreted in the context of the patient’s specific clinical history, and the diagnosis of an allergic disorder cannot be based solely on a laboratory result.
The demonstration of sensitization is not sufficient to diagnose an allergy, however, because a sensitized individual may be entirely asymptomatic upon exposure to the allergen in question. Thus, allergy tests must be interpreted in the context of the patient’s specific clinical history, and the diagnosis of an allergic disorder cannot be based solely on a laboratory result.
 If the result is markedly positive (e.g., a Class VI result), the history suggests a past reaction to the allergen, and the allergen is well characterized, then the diagnosis of an allergy can usually be made without further evaluation. If the result is weakly positive, then further evaluation is usually needed.
If the result is markedly positive (e.g., a Class VI result), the history suggests a past reaction to the allergen, and the allergen is well characterized, then the diagnosis of an allergy can usually be made without further evaluation. If the result is weakly positive, then further evaluation is usually needed.
 A negative immunoassay result in the setting of a strongly suggestive history does not exclude allergy. In this situation, a skin prick test should be considered (if not contraindicated).
A negative immunoassay result in the setting of a strongly suggestive history does not exclude allergy. In this situation, a skin prick test should be considered (if not contraindicated).
 False-positive results of allergen-specific IgE can theoretically occur in patients with extremely elevated total IgE levels.
False-positive results of allergen-specific IgE can theoretically occur in patients with extremely elevated total IgE levels.
 Tests used largely in research settings include immunoblotting, basophil histamine or leukotriene release tests, basophil activation, and levels of eosinophil mediators, etc., are not standardized, and are generally not superior to skin testing, and cannot be recommended for routine clinical use.
Tests used largely in research settings include immunoblotting, basophil histamine or leukotriene release tests, basophil activation, and levels of eosinophil mediators, etc., are not standardized, and are generally not superior to skin testing, and cannot be recommended for routine clinical use.
 Allergen-specific IgG and IgG4 tests, which are believed to correlate with normal immunologic responses to foreign substances, are not useful in the diagnosis of IgE-mediated allergy, with the exception of venom allergy. Unreliable testing methods include provocation/neutralization tests, kinesiology, cytotoxic tests, and electrodermal testing.
Allergen-specific IgG and IgG4 tests, which are believed to correlate with normal immunologic responses to foreign substances, are not useful in the diagnosis of IgE-mediated allergy, with the exception of venom allergy. Unreliable testing methods include provocation/neutralization tests, kinesiology, cytotoxic tests, and electrodermal testing.
 In food allergy, circulating IgE antibodies may remain undetectable despite a convincing clinical history because these antibodies may be directed toward allergens that are revealed or altered during industrial processing, cooking, or digestion and therefore do not exist in the original food for which the patient is tested.
In food allergy, circulating IgE antibodies may remain undetectable despite a convincing clinical history because these antibodies may be directed toward allergens that are revealed or altered during industrial processing, cooking, or digestion and therefore do not exist in the original food for which the patient is tested.
 Identical results for different allergens may not be associated with clinically equivalent manifestations, due to differences in patient sensitivities.
Identical results for different allergens may not be associated with clinically equivalent manifestations, due to differences in patient sensitivities.
ALBUMIN, SERUM
 Definition
Definition
 Albumin is the most important protein and constitutes 55–65% of total plasma protein. Approximately 300–500 g of albumin is distributed in the body fluids, and the average adult liver synthesizes approximately 15 g/day. Albumin’s half-life is approximately 20 days, with 4% of the total albumin pool being degraded daily. The serum albumin concentration reflects the rate of synthesis, the degradation, and the volume of distribution. Albumin synthesis is regulated by a variety of influences, including nutritional status, serum oncotic pressure, cytokines, and hormones.
Albumin is the most important protein and constitutes 55–65% of total plasma protein. Approximately 300–500 g of albumin is distributed in the body fluids, and the average adult liver synthesizes approximately 15 g/day. Albumin’s half-life is approximately 20 days, with 4% of the total albumin pool being degraded daily. The serum albumin concentration reflects the rate of synthesis, the degradation, and the volume of distribution. Albumin synthesis is regulated by a variety of influences, including nutritional status, serum oncotic pressure, cytokines, and hormones.
 Normal range:
Normal range:
 0–4 months: 2.0–4.5 g/dL
0–4 months: 2.0–4.5 g/dL
 4 months−16 years: 3.2–5.2 g/dL
4 months−16 years: 3.2–5.2 g/dL
 >16 years: 3.5–4.8 g/dL
>16 years: 3.5–4.8 g/dL
 Use
Use
 Assess nutritional status
Assess nutritional status
 Evaluate chronic illness
Evaluate chronic illness
 Evaluate liver disease
Evaluate liver disease
 Interpretation
Interpretation
Increased In
 Dehydration
Dehydration
 High-protein diet
High-protein diet
Decreased In
 Decreased synthesis by the liver:
Decreased synthesis by the liver:
 Acute and chronic liver disease (e.g., alcoholism, cirrhosis, hepatitis)
Acute and chronic liver disease (e.g., alcoholism, cirrhosis, hepatitis)
 Malabsorption and malnutrition
Malabsorption and malnutrition
 Fasting, protein–calorie malnutrition
Fasting, protein–calorie malnutrition
 Amyloidosis
Amyloidosis
 Chronic illness
Chronic illness
 DM
DM
 Decreased growth hormone levels
Decreased growth hormone levels
 Hypothyroidism
Hypothyroidism
 Hypoadrenalism
Hypoadrenalism
 Genetic analbuminemia
Genetic analbuminemia
 Acute-phase reaction, inflammation, and chronic diseases:
Acute-phase reaction, inflammation, and chronic diseases:
 Bacterial infections
Bacterial infections
 Monoclonal gammopathies and other neoplasms
Monoclonal gammopathies and other neoplasms
 Parasitic infestations
Parasitic infestations
 Peptic ulcer
Peptic ulcer
 Prolonged immobilization
Prolonged immobilization
 Rheumatic diseases
Rheumatic diseases
 Severe skin disease
Severe skin disease
 Increased loss over body surface:
Increased loss over body surface:
 Burns
Burns
 Enteropathies related to sensitivity to ingested substances (e.g., gluten sensitivity, Crohn disease, ulcerative colitis)
Enteropathies related to sensitivity to ingested substances (e.g., gluten sensitivity, Crohn disease, ulcerative colitis)
 Fistula (gastrointestinal or lymphatic)
Fistula (gastrointestinal or lymphatic)
 Hemorrhage
Hemorrhage
 Kidney disease
Kidney disease
 Rapid hydration or overhydration
Rapid hydration or overhydration
 Repeated thoracentesis or paracentesis
Repeated thoracentesis or paracentesis
 Trauma and crush injuries
Trauma and crush injuries
 Increased catabolism:
Increased catabolism:
 Fever
Fever
 Cushing disease
Cushing disease
 Preeclampsia
Preeclampsia
 Thyroid dysfunction
Thyroid dysfunction
 Plasma volume expansion:
Plasma volume expansion:
 CHF
CHF
 Oral contraceptives
Oral contraceptives
 Pregnancy
Pregnancy
 Limitations
Limitations
 In clinical practice, one of the two dye-binding assays—bromocresol green (BCG) and bromocresol purple (BCP)—is used for measuring albumin levels, and systematic differences between these methods have long been recognized.
In clinical practice, one of the two dye-binding assays—bromocresol green (BCG) and bromocresol purple (BCP)—is used for measuring albumin levels, and systematic differences between these methods have long been recognized.
 BCG methods are subject to nonspecific interference from binding to nonalbumin proteins, whereas BCP is more specific. BCP has been shown to underestimate serum albumin in pediatric patients on hemodialysis and patients in chronic renal failure. Chronic dialysis units often have little influence over the method.
BCG methods are subject to nonspecific interference from binding to nonalbumin proteins, whereas BCP is more specific. BCP has been shown to underestimate serum albumin in pediatric patients on hemodialysis and patients in chronic renal failure. Chronic dialysis units often have little influence over the method.
 Antialbumin antibodies are commonly found with hepatic dysfunction and are typically of IgA type.
Antialbumin antibodies are commonly found with hepatic dysfunction and are typically of IgA type.
 Ischemia-modified albumin, in which the metal-binding capacity of albumin has decreased due to exposure to ischemic events, is a biologic marker of myocardial ischemia.
Ischemia-modified albumin, in which the metal-binding capacity of albumin has decreased due to exposure to ischemic events, is a biologic marker of myocardial ischemia.
ALCOHOLS (VOLATILES, SOLVENTS)*
 Definition
Definition
 Alcohols are organic compounds that contain the −OH group, including methanol (CH3 OH), ethanol (ethyl alcohol; C2 H5 OH), isopropanol (rubbing alcohol), and methanol (wood alcohol). Although acetone (CH3 COCH3 ) is a ketone, not an alcohol, it is included in this group, because it is often detected in the same testing methodology.
Alcohols are organic compounds that contain the −OH group, including methanol (CH3 OH), ethanol (ethyl alcohol; C2 H5 OH), isopropanol (rubbing alcohol), and methanol (wood alcohol). Although acetone (CH3 COCH3 ) is a ketone, not an alcohol, it is included in this group, because it is often detected in the same testing methodology.
 Normal range:
Normal range:
 Ethanol: <10 mg/dL.
Ethanol: <10 mg/dL.
 50 mg/dL: decreased inhibition, slight incoordination
50 mg/dL: decreased inhibition, slight incoordination
 100 mg/dL: slow reaction time; altered sensory ability
100 mg/dL: slow reaction time; altered sensory ability
 150 mg/dL: altered thought processes; personality, behavior changes
150 mg/dL: altered thought processes; personality, behavior changes
 200 mg/dL: staggering gait, nausea, vomiting, mental confusion
200 mg/dL: staggering gait, nausea, vomiting, mental confusion
 300 mg/dL: slurred speech, sensory loss, visual disturbance
300 mg/dL: slurred speech, sensory loss, visual disturbance
 400 mg/dL: hypothermia, hypoglycemia, poor muscle control, seizures
400 mg/dL: hypothermia, hypoglycemia, poor muscle control, seizures
 700 mg/dL: unconsciousness, decreased reflexes, respiratory failure (may also occur at lower concentrations)
700 mg/dL: unconsciousness, decreased reflexes, respiratory failure (may also occur at lower concentrations)
 Isopropanol (isopropyl alcohol): <10 mg/dL (normal); toxic effects generally seen at 50–100 mg/dL.
Isopropanol (isopropyl alcohol): <10 mg/dL (normal); toxic effects generally seen at 50–100 mg/dL.
 Methanol: <10 mg/dL (normal); levels >25 mg/dL are generally considered toxic.
Methanol: <10 mg/dL (normal); levels >25 mg/dL are generally considered toxic.
 Acetone: <10 mg/dL; effects are said to be similar to ethanol for similar blood levels, but the anesthetic potency is greater.
Acetone: <10 mg/dL; effects are said to be similar to ethanol for similar blood levels, but the anesthetic potency is greater.
 Use
Use
 Beverage (ethanol)
Beverage (ethanol)
 Solvent and reagent
Solvent and reagent
 Vehicle in chemical and pharmaceutical industries
Vehicle in chemical and pharmaceutical industries
 Antiseptic (isopropyl alcohol)
Antiseptic (isopropyl alcohol)
 Limitations
Limitations
 Immunoassay testing for ethanol may have cross-reactivity <1% with isopropanol alcohol, methanol, ethylene glycol, and acetaldehyde; <15% with n-propanol.
Immunoassay testing for ethanol may have cross-reactivity <1% with isopropanol alcohol, methanol, ethylene glycol, and acetaldehyde; <15% with n-propanol.
 Elevated concentrations of acetone are detected in specimens during diabetic ketoacidosis and fasting ketoacidosis and may range from 10 to 70 mg/dL.
Elevated concentrations of acetone are detected in specimens during diabetic ketoacidosis and fasting ketoacidosis and may range from 10 to 70 mg/dL.
 In many headspace gas chromatographic methods, acetonitrile coelutes with acetone, leading to a false-positive result. Acetonitrile may be a component in cosmetic nail remover.
In many headspace gas chromatographic methods, acetonitrile coelutes with acetone, leading to a false-positive result. Acetonitrile may be a component in cosmetic nail remover.
 A positive urine ethanol due to the presence of yeast in the patient’s urine has been described. In these cases, glucose was also present in the urine.
A positive urine ethanol due to the presence of yeast in the patient’s urine has been described. In these cases, glucose was also present in the urine.
ALDOSTERONE
 Definition
Definition
 Primary mineralocorticoid secreted by the adrenal zona glomerulosa. The role of aldosterone in metabolism is the control of sodium and potassium. Regulating sodium ion concentration, in turn, regulates fluid volume. Aldosterone acts to decrease excretion of sodium and increase the excretion of potassium at the kidney, sweat glands, and salivary glands.
Primary mineralocorticoid secreted by the adrenal zona glomerulosa. The role of aldosterone in metabolism is the control of sodium and potassium. Regulating sodium ion concentration, in turn, regulates fluid volume. Aldosterone acts to decrease excretion of sodium and increase the excretion of potassium at the kidney, sweat glands, and salivary glands.
 Normal range:
Normal range:
 8:00–10:00 AM (sitting): 3–34 ng/dL
8:00–10:00 AM (sitting): 3–34 ng/dL
 8:00–10:00 AM (supine): 2–19 ng/dL
8:00–10:00 AM (supine): 2–19 ng/dL
 4:00–6:00 PM (sitting): 2–23 ng/dL
4:00–6:00 PM (sitting): 2–23 ng/dL
 Use
Use
 Diagnosis of primary hyperaldosteronism
Diagnosis of primary hyperaldosteronism
 Differential diagnosis of fluid and electrolyte disorders
Differential diagnosis of fluid and electrolyte disorders
 Assessment of adrenal aldosterone production
Assessment of adrenal aldosterone production
 Interpretation
Interpretation
Increased In
 Primary aldosteronism
Primary aldosteronism
 Secondary aldosteronism
Secondary aldosteronism
 Barter syndrome
Barter syndrome
 Pregnancy
Pregnancy
 Very low–sodium diet
Very low–sodium diet
 Urine aldosterone also increased in nephrosis
Urine aldosterone also increased in nephrosis
Decreased In
 Hyporeninemic hypoaldosteronism (Cushing syndrome)
Hyporeninemic hypoaldosteronism (Cushing syndrome)
 CAH
CAH
 Congenital deficiency of aldosterone synthetase
Congenital deficiency of aldosterone synthetase
 Addison disease
Addison disease
 Very high–sodium diet
Very high–sodium diet
 Limitations
Limitations
 Many physiologic factors affect plasma aldosterone. Posture, salt intake, use of antihypertensive drugs, use of steroids, oral contraceptives, age, stress, exercise, menstrual cycle, and pregnancy can all have a strong influence on aldosterone results.
Many physiologic factors affect plasma aldosterone. Posture, salt intake, use of antihypertensive drugs, use of steroids, oral contraceptives, age, stress, exercise, menstrual cycle, and pregnancy can all have a strong influence on aldosterone results.
 Licorice may mimic aldosterone effects and should be avoided 2 weeks before the test.
Licorice may mimic aldosterone effects and should be avoided 2 weeks before the test.
ALKALINE PHOSPHATASE (ALP)
 Definition
Definition
 ALP refers to a family of enzymes that catalyze hydrolysis of phosphate esters at an alkaline pH. There are at least five isoenzymes derived from the liver (sinusoidal and bile canalicular surface of hepatocytes), bone, intestine (brush border of mucosal cells), placenta, and tumor-associated tissues separated by electrophoresis. Placenta and tumor-associated ALP are the most heat resistant to inactivation. More than 95% of total ALP activity comes from the bone and liver (approximately 1:1 ratio). The half-life of ALP is 7–10 days.
ALP refers to a family of enzymes that catalyze hydrolysis of phosphate esters at an alkaline pH. There are at least five isoenzymes derived from the liver (sinusoidal and bile canalicular surface of hepatocytes), bone, intestine (brush border of mucosal cells), placenta, and tumor-associated tissues separated by electrophoresis. Placenta and tumor-associated ALP are the most heat resistant to inactivation. More than 95% of total ALP activity comes from the bone and liver (approximately 1:1 ratio). The half-life of ALP is 7–10 days.
 Normal range:
Normal range:
 0–1 year: 150–350 IU/L
0–1 year: 150–350 IU/L
 1–16 years: 30–300 IU/L
1–16 years: 30–300 IU/L
 >16 years: 30–115 IU/L
>16 years: 30–115 IU/L
 Use
Use
 Diagnosis and treatment of the liver, bone, intestinal, and parathyroid diseases
Diagnosis and treatment of the liver, bone, intestinal, and parathyroid diseases
 Interpretation
Interpretation
Increased In
 Increased bone formation
Increased bone formation
 Bone diseases (metastatic carcinoma of the bone, myeloma, Paget disease)
Bone diseases (metastatic carcinoma of the bone, myeloma, Paget disease)
 Renal disease (renal rickets due to vitamin D–resistant rickets associated with secondary hyperparathyroidism)
Renal disease (renal rickets due to vitamin D–resistant rickets associated with secondary hyperparathyroidism)
 Liver disease (e.g., infectious mononucleosis, uncomplicated extrahepatic biliary obstruction, liver abscess)
Liver disease (e.g., infectious mononucleosis, uncomplicated extrahepatic biliary obstruction, liver abscess)
 Miscellaneous (extrahepatic sepsis, ulcerative colitis, pancreatitis, phenytoin, and alcohol use)
Miscellaneous (extrahepatic sepsis, ulcerative colitis, pancreatitis, phenytoin, and alcohol use)
 Bone origin—increased deposition of calcium
Bone origin—increased deposition of calcium
 Hyperparathyroidism
Hyperparathyroidism
 Paget disease (osteitis deformans) (highest reported values 10–20 times normal). Marked elevation in the absence of liver disease is most suggestive of Paget disease of bone or metastatic carcinoma from the prostate.
Paget disease (osteitis deformans) (highest reported values 10–20 times normal). Marked elevation in the absence of liver disease is most suggestive of Paget disease of bone or metastatic carcinoma from the prostate.
 Increase in cases of metastases to bone is marked only in prostate carcinoma.
Increase in cases of metastases to bone is marked only in prostate carcinoma.
 Osteoblastic bone tumors (osteogenic sarcoma, metastatic carcinoma).
Osteoblastic bone tumors (osteogenic sarcoma, metastatic carcinoma).
 Osteogenesis imperfecta (due to healing fractures).
Osteogenesis imperfecta (due to healing fractures).
 Familial osteoectasia.
Familial osteoectasia.
 Osteomalacia, rickets.
Osteomalacia, rickets.
 Polyostotic fibrous dysplasia.
Polyostotic fibrous dysplasia.
 Osteomyelitis.
Osteomyelitis.
 Late pregnancy; reverts to normal level by 20th day postpartum.
Late pregnancy; reverts to normal level by 20th day postpartum.
 Children <10 years of age and again during prepubertal growth spurt may have three to four times adult values; adult values are attained by age 20.
Children <10 years of age and again during prepubertal growth spurt may have three to four times adult values; adult values are attained by age 20.
 Administration of ergosterol.
Administration of ergosterol.
 Hyperthyroidism.
Hyperthyroidism.
 Transient hyperphosphatasemia of infancy
Transient hyperphosphatasemia of infancy
 Hodgkin disease.
Hodgkin disease.
 Healing of extensive fractures (slightly).
Healing of extensive fractures (slightly).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


