15 CASE 15
PATHOPHYSIOLOGY OF KEY SYMPTOMS
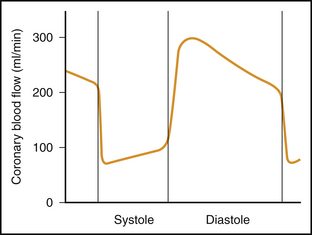
Morphine is useful for pain relief and is particularly important because pain increases sympathetic nervous system (SNS) activity, exacerbating the progression of myocardial damage through multiple pathways. SNS activation increases arterial blood pressure and thus increases the workload on the left ventricle. The majority of blood flow to the left ventricle occurs during diastole, and the SNS-mediated increase in heart rate diminishes diastolic duration and impairs blood flow particularly to the left ventricle. SNS activation also increases ventricular contractility and, therefore, ventricular work load (Fig. 15-1).
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree