PEDIATRIC CRITICAL CARE
Objectives
• Recognize factors that contribute to errors in drug and fluid administration.
• Identify the steps in calculating dilution parameters.
• Determine the accuracy of the dilution parameters in a drug order.
In delivery of emergency drugs with complex dilution calculations, it is important for the nurse to evaluate the accuracy of the physician’s order and to ensure that a child does not receive excessive fluids. Many institutions are attempting to standardize the concentration of the solution for various pediatric intravenous (IV) dosages to decrease the occurrence of miscalculations. National efforts are under way to standardize IV emergency drugs for infusion to eliminate medication errors.
As noted in Chapter 12, the concepts of concentration of the solution, infusion rates for concentration and volume, and concentration of a drug for specific body weight per unit time that are used in adult critical care are also used to prepare pediatric doses.
FACTORS INFLUENCING INTRAVENOUS ADMINISTRATION
Excess fluid can be given when the fluid volume of the emergency drug is not considered in the 24-hour fluid intake. Long IV tubing can be another source of fluid excess and can cause errors in drug delivery. When the priming or filling volume of the IV tubing is not considered, the child may receive extra fluid, especially if medication is added to the primary IV set via a secondary IV set. IV medication may not reach the child if the IV infusion rate is low, such as 1 mL/hr, or if the IV tubing has not been primed or filled with the medication before infusion. Most pediatric departments are developing protocols for safe and consistent IV drug delivery.
CALCULATING ACCURACY OF DILUTION PARAMETERS
The nurse may find it necessary to calculate the dilution parameters of a drug order that specifies the concentration per kilogram per minute and the volume per hour infusion rate. The physician should determine all drug dose parameters, including concentration per kilogram per minute, volume per hour, and dilution parameters. The nurse should check the accuracy of the dilution parameters to ensure that the correct drug dosage is given. These methods are also used to prepare the pediatric dose. In many pediatric critical care areas, IV fluids for drug administration are limited to prevent fluid overload. If the physician changes the drug dosage, rather than increasing the volume (mL), the concentration of the solution will be changed. It is important that all health care providers follow the policies and procedures of their institution regarding medication administration.
EXAMPLES
PROBLEM 1: A 5-year-old-child, weight 14 kg, with septic shock.
Order: Dobutamine 10 mcg/kg/min at 2.1 mL/hr titrate to keep SBP >90.
Dilute as follows: Dobutamine 200 mg in D5W to make a total volume of 50 mL for a syringe pump.
Pediatric dosage: 2-20 mcg/kg/min.
Drug available: Dobutamine 250 mg/20 mL.
Here are the following checks that can determine whether the infusion rate and the dilution orders will result in the correct concentration delivered according to weight.
Step 1: Calculate infusion concentration rates per minute and hour.
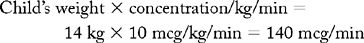
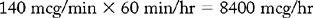
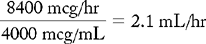
Step 2: Calculate the concentration of the solution. Check order by dividing concentration per hour by the ordered mL per hour. Results should match.
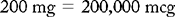

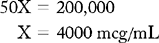
The concentration solution matches.
Step 3: Calculate the infusion rate, volume per hour. Divide concentration per hour by concentration of solution. Results should confirm the infusion rate in order.
Infusion rate is correct.
Step 4: Calculate drug order.
H : V :: D : V
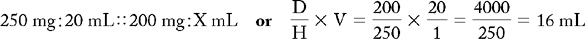
Dobutamine 200 mg is 16 mL. Find the amount of D5W by subtracting 16 mL of dobutamine drug volume from 50 mL; 34 mL of D5W is needed to fill the 50-mL syringe.
PROBLEM 2: A 3-week-old premature infant, weight 1.6 kg, in shock.
Order: Dopamine 2.5 mcg/kg/min at 0.6 mL/hr.
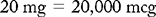
Dilute as follows: Dopamine 20 mg in D5W to make a total of 50 mL for syringe pump.
Dosage range: 2 to 20 mg/kg/min.
Drug available: Dopamine 200 mg/5 mL.
Check to determine whether the infusion rate and the dilution orders will result in the correct concentration delivered according to weight.
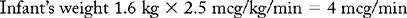
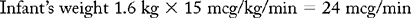
Step 1: Calculate the concentration per minute and per hour, based on weight.
a. Concentration rate per minute
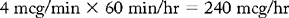
b. Concentration rate per hour
Step 2: Calculate the concentration of the solution. Check order by dividing concentration per hour by the ordered mL per hour. Results should match.
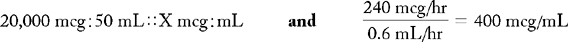
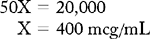
The concentration of solution matches.
Step 3: Calculate the infusion rate, volume per hour. Divide concentration per hour by concentration solution. Results should confirm the infusion rate in order.
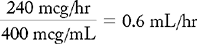
Infusion rate is correct.
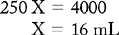
Step 4: Calculate dilution orders.
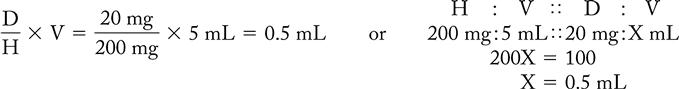
Dopamine 20 mg is 0.5 mL. Find the amount of D5W needed by subtracting 0.5 mL of dopamine drug volume from 50 mL; 49.5 mL of D5W is needed to fill the 50-mL syringe.
PROBLEM 3: For the same infant, the physician increases the dose of dopamine.
Order: Dopamine 15 mcg/kg/min at 1.8 mL/hr.
Dilution: Same, dopamine 20 mg in 50 mL with a syringe pump.
Pediatric dosage range: 2-20 mcg/kg/min.
Drug available: Dopamine 200 mg/5 mL.
Check to determine whether the infusion rate and the dilution orders will result in the correct concentration delivered according to weight.
Step 1: Calculate the concentration per minute and per hour based on weight.
a. Concentration rate per minute
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


