CRITICAL CARE
Objectives
• Calculate the prescribed concentration of a drug in solution.
• Identify the units of measure designated for the amount of drug in solution.
• Describe the four determinants of infusion rates.
• Calculate the concentration of drug per unit of time for a specific body weight.
• Recognize the variables needed for the basic fractional formula.
• Describe how the titration factor is used when infusion rates are changed.
• Recognize the methods of determining the total amount of drug infused over time.
In critical care areas, medication is primarily given intravenously and therefore has an immediate systemic effect on the patient. Drug dosages can be highly individualized with the patient monitored closely for an improvement in vital signs, urine output, cardiac index, or whatever the appropriate parameter. Since intravenous (IV) medication can have immediate effects, it can also pose the greatest risk. Therefore, it is essential that the nurse understands the drug action and the calculations necessary for infusion safety.
Administration of potent drugs—drugs that cause major physiological changes—may be delivered in milligrams, micrograms, or units per body weight or unit time. The physician determines the drug dosage and rate of infusion either per body weight or unit time, per hour or per minute. Depending on the medication, the physician may give the type of IV solution for the dilution. Some institutions have their own pharmacy guidelines or protocols for preparation of drugs for continuous IV infusion in critical care areas. Hospitals are now initiating policies of drug infusion standardization, especially for the concentration of solution. Premixed, ready-to-use IV drugs in solution are also available from drug manufacturers with standardized dosages. The nurse is the last step in the administration process and must make sure that the dosage and the infusion rate are correct.
National research has shown a high incidence of IV drug errors committed by pharmacists, physicians, and nurses. Complete examination of the medication processes is under way across the country in an effort to eliminate adverse drug errors. One step in the process has been to identify drugs with the highest potential to do harm when used in error. Now these drugs are referred to as “high-alert” drugs and identified in some facilities with special labeling (Table 12-1). Another effort under way is the increasing use of programmable infusion pump technology or “smart pumps.” These pumps have drug menus called “libraries” entered into their software with safe dosing limits attached. The unit will alarm if the limits are breached and prevent infusions beyond the safe dose range. The smart pump’s technology allows a facility to program the pump for specific areas, i.e., adult, pediatric, oncology, and anesthesia.
TABLE 12-1
| Drug Class | Examples |
| Adrenergic agonists | Epinephrine, norepinephrine, dopamine, dobutamine |
| Adrenergic antagonists | Esmolol |
| Anesthetics | Propofol |
| Antiarrhythmics | Amiodarone, lidocaine |
| Anticoagulants | Heparin, bivalirudin, argatroban, lepirudin |
| Antineoplastics | |
| Dextrose, hypertonic, 20% or greater | |
| Electrolyte solutions | Potassium chloride, potassium phosphate, magnesium sulfate |
| Fibrinolytics | Streptokinase, anistreplase, alteplase |
| Glycoprotein llb/llla inhibitors | Eptifibatide |
| notropics | Milrinone |
| Insulin | |
| Liposomal forms of drugs | Liposomal amphotericin |
| Moderate sedatives | Midazolam, lorazepam, diazepam |
| Neuromuscular blockers | Atracurium, vecuronium, cisatracurium |
| Opiates | |
| Total parenteral nutrition solutions | |
| Vasodilators | Nitroglycerin, nitroprusside, nesiritide |
Adapted from Dennison, Robin D. High-alert drugs: Strategies for some IV infusions. American Nurse Today, July 2008.
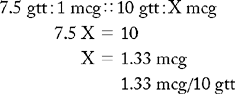
When the nurse uses the smart pump she or he first selects the drug from the drug library. The library list of drugs is distinguished by capitalized letters that emphasize spelling differences for drugs with similar names. The nurse selects the amount of the drug and the amount of the prescribed soluton for infusion, and the pump calculates the concentration of solution. If the drug is dosed based on patient weight, the most current weight is entered. Next, the nurse enters the unit time, either minutes or hours, and the pump calculates volume per hour or volume per minute. If a weight-based dosage is used, the smart pump will calculate dosage per kilogram body weight per minute.
The smart pump is an effective tool for drug administration, but the nurse must know all the drug calculations used in critical care and how they are applied to verify the correct dose before it is given to the patient. These are as follows:
For high-alert drugs it is recommended that two nurses independently do the drug calculations and verify the results. If any questions arise regarding dosing or infusion rates, the pharmacist and the physician should be consulted before the drug is administered to the patient.
CALCULATING AMOUNT OF DRUG OR CONCENTRATION OF A SOLUTION
The first step in administering a medication is to determine the concentration of the solution, which is the amount of drug in each milliliter of solution. This is written as units per milliliter, milligrams per milliliter, or micrograms per milliliter and must be calculated for each problem. For all problems, remember to convert to like units before solving.
Calculating Units per Milliliter
EXAMPLE
Infuse heparin 5000 units in D5W 250 mL at 30 mL/hr. What will be the concentration of heparin in each milliliter of D5W?
Method: units/mL
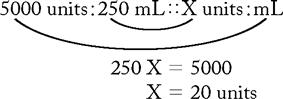
Answer: The D5W with heparin will have a concentration of 20 units/mL of solution.
Calculating Milligrams per Milliliter
EXAMPLE
Infuse lidocaine 2 g in 500 mL D5W at 2 mg/min. What will be the concentration of lidocaine in each milliliter of D5W?
Method: mg/mL
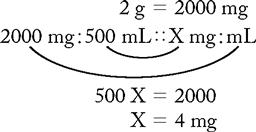
Answer: The D5W with lidocaine has a concentration of 4 mg/mL of solution.
Calculating Micrograms per Milliliter
EXAMPLE
Infuse dobutamine 250 mg in 500 mL D5W at 650 mcg/min. What is the concentration of dobutamine in each milliliter of D5W?
Method: mcg/mL
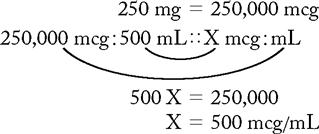
Answer: The D5W with dobutamine will have a concentration of 500 mcg/mL of solution.
CALCULATING INFUSION RATE FOR CONCENTRATION AND VOLUME PER UNIT TIME
The second step for administering medication is to calculate the infusion rate of drug per unit time. Infusion rates can mean two things: the rate of volume (mL) given or the rate of concentration (units, mg, mcg) administered. Unit time means per hour or per minute. For drugs administered by continuous infusion, the four most important determinants are the concentration per hour and minute and the volume per hour and minute. Infusion rates of high-alert drugs are usually part of the physician’s order and may be stated in concentration or volume per unit time.
Many hospitals have policies requiring that all high-alert drugs be delivered via smart infusion pumps. New technology has produced pumps that are programmable and calculate the drug dosage. The information entered in the pump’s control panel is (1) the name of the drug, (2) the concentration of the drug, (3) the volume of the solution, and (4) the patient’s weight in kilograms. The nurse enters the ordered dose and the correct dosage parameters, i.e., mg/min, units/hr, mcg/min. The pump automatically delivers the appropriate dosage.
Not all facilities have infusion pumps with advanced technology; therefore, the nurse must be able to calculate the infusion rates. For general-purpose infusion pumps that deliver mL/hr, the volume per hour of the drug must be known. Remember: If an infusion device is unavailable, a microdrip IV administration set is the appropriate set to use because the drops per minute rate (gtt/min) corresponds to the volume per hour rate (mL/hr).
Complete infusion rates for volume and concentration are given in the examples and practice problems. In clinical practice, not all the data are needed for each drug. For heparin, the concentration per minute is not as vital as the concentration per hour, whereas for vasoactive drugs such as dobutamine, the concentration per minute is essential information and the concentration per hour is not. The same methods of calculation are used for both drugs, and the same information can be obtained. The nurse must have knowledge of pharmacology and clinical practice to determine the most useful data.
Concentration and Volume per Hour and Minute with a Drug in Units
EXAMPLES
Infuse heparin 5000 units in D5W 250 mL at 30 mL/hr. Concentration of solution is 20 units/mL. (Also note that volume/hour is given.) How many milliliters will be infused per minute?
Find volume per minute:
Method: mL/min
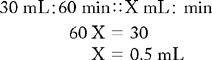
Answer:The infusion rate for volume per minute is 0.5 mL/min and the hourly rate is 30 mL/hr.
What is the concentration per minute and hour?
Find concentration per minute:
Method: units/min
20 units/mL × 0.5 mL/min = 10 units/min
Find concentration per hour:
Method: units/hr
10 units/min × 60 min/hr = 600 units/hr
Answer: The concentration per minute of heparin is 10 units/min and the concentration per hour is 600 units/hr.
Concentration and Volume per Hour and Minute with a Drug in Milligrams
EXAMPLES
Infuse lidocaine 2 g in D5W 500 mL at 2 mg/min. Concentration of solution is 4 mg/mL. (Also note that concentration/minute is given.) How many milligrams will be infused per hour?
Find concentration per hour:
Method: mg/hr
lidocaine 2 mg/min
2 mg/min × 60 min = 120 mg/hr
Answer: The amount of lidocaine infused per hour is 120 mg/hr.
How many milliliters of lidocaine will be infused in 1 hour?
Find volume per hour:
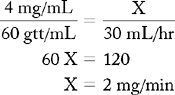
Method: mL/hr
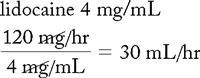
Answer: The infusion rate in milliliters for lidocaine 2 mg/min is 30 mL/hr.
How many milliliters of lidocaine will be infused in 1 minute?
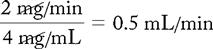
Answer: The infusion rate for lidocaine 2 mg/min is 0.5 mL/min.
Concentration and Volume per Hour and Minute with a Drug in Micrograms
EXAMPLES
Infuse dobutamine 250 mg in D5W 500 mL at 650 mcg/min. Concentration of solution is 500 mcg/mL. (Also note that concentration/minute is given in the order.) How many micrograms will be infused in 1 hour?
Find concentration per hour:
Method: mcg/hr
dobutamine 650 mcg/min
650 mcg/min × 60 min/hr = 39,000 mcg/hr
Answer:The concentration of dobutamine infused per hour is 39,000 mcg/hr.
How many milliliters of dobutamine will be infused in 1 hour?
Find volume per hour:
Method: mL/hr
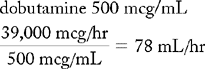
Answer:The infusion rate for dobutamine 650 mcg/min is 78 mL/hr.
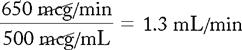
How many milliliters of dobutamine should be infused in 1 minute?
Find volume per minute:
Method: mL/min
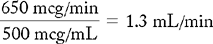
Answer: The infusion rate for dobutamine is 1.3 mL/min.
CALCULATING INFUSION RATES OF A DRUG FOR SPECIFIC BODY WEIGHT PER UNIT TIME
The last method is calculating infusion rates for the amount of drug per unit time for a specific body weight. The weight parameter is an accurate means of dosing for a therapeutic effect. The metric system is used for all drug dosing, so pounds must be changed to kilograms. The physician orders the desired dose per kilogram of body weight and the concentration of the solution. From this information, infusion rates can be calculated for administering an individualized dose. Accurate daily weights are essential for the correct dosage.
The previous methods for calculating concentration of solution and infusion rates for concentration and volume are used, with one addition. The concentration per minute is obtained by multiplying the body weight by the desired dose per kilogram per minute, which must be done before the other infusion rates can be calculated. For many vasoactive drugs given as examples in this chapter, the most useful information clinically is the concentration per minute for the specific body weight, volume per minute, and volume per hour, because these parameters determine the infusion pump settings.
New volumetric infusion pumps can now deliver fractional portions of a milliliter from tenths to hundredths in addition to calculating dosages for infusion rates. If the infusion pumps available do not have this feature and the volume per hour is a fractional amount, it must be rounded off to a whole number (1.8 mL/hr = 2 mL/hr). When calculating concentration per minute and hour and volume per minute, carry out the problem to three decimal places, if necessary, before rounding off. The volume per hour, if fractional, can then be rounded off, making the volume per hour as accurate as possible. There are two exceptions to rounding off fractional infusion rates:
Micrograms per Kilogram Body Weight
EXAMPLES
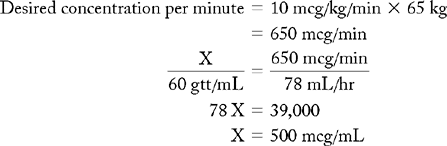
Infuse dobutamine 250 mg in 500 mL D5W at 10 mcg/kg/min. Patient weighs 143 lb. Concentration of solution is 500 mcg/mL. How many micrograms of dobutamine would be infused per minute? Per hour?
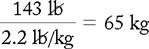
Convert pounds to kilograms:
Find concentration per minute:
Method: mcg/min
65 kg × 10 mcg/kg/min = 650 mcg/min
Find concentration per hour:
Method: mcg/hr
650 mcg/min × 60 min/hr = 39,000 mcg/hr
Answer:The concentration of dobutamine infused per minute and per hour is 650 mcg/min and 39,000 mcg/hr for the patient’s body weight.
How many milliliters of dobutamine will be infused per minute? Per hour? Find volume per minute:
Method: mL/min
Find volume per hour:
Method: mL/hr
1.3 mL/min × 60 min/hr = 78 mL/hr
Answer: The volume of dobutamine infused per minute is 1.3 mL/min, and the infusion rate is 78 mL/hr.
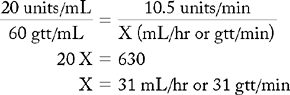
BASIC FRACTIONAL FORMULA
A fractional equation can create a basic formula that can be used as another quick method to determine any one of the following quantities: concentration of solution, volume per hour, and desired concentration per minute (× kilogram of body weight, if required). The equation has one constant, the drop rate of the IV set, 60 gtt/mL. The unknown quantity can be represented by X. (See Chapter 5 for fractional equations.) The basic formula is not accurate to the nearest hundredth, as are the other methods in this section:
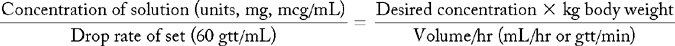
Using Basic Formula to Find Volume per Hour or Drops per Minute
EXAMPLE
Infuse heparin 5000 units in 250 mL D5W at 0.15 units/kg/min.
Patient weighs 70 kg. The concentration of solution is 20 units/mL.
Desired concentration/minute: 0.15 units/kg/min × 70 kg = 10.5 units/min
Using Basic Formula to Find Desired Concentration per Minute
EXAMPLE
Infuse lidocaine 2 g in 500 mL D5W at 30 mL/hr. The concentration of the solution is 4 mg/mL.
Using Basic Formula to Find Concentration of Solution
EXAMPLE
Infuse dobutamine 250 mg in D5W 500 mL at 10 mcg/kg/min with rate of 78 mL/hr. Patient weighs 65 kg.
TITRATION OF INFUSION RATE
High-alert drugs are given to improve a physiological function that is causing a life-threatening condition for the patient. Every high-alert drug produces a physiological response that should be monitored and evaluated for effectiveness. For example, a patient receiving aminophylline should be monitored for improved respiratory rate and breath sounds. Another example is nitroprusside, where a patient’s decrease in blood pressure is the goal of therapy. Monitoring parameters should be a part of the physician’s order.
The purpose of titration in medication administration is to give the least amount of drug in the therapeutic range to elicit the appropriate targeted physiological response. With the smart pump, the therapeutic ranges are calculated. If a general-purpose infusion pump is used, the nurse should calculate the upper and lower limits of the therapeutic range.
Titration of drugs administered by infusion is based on (1) concentration of solution, (2) infusion rates, (3) specific concentration per kilogram of body weight, and (4) titration factor. The titration factor is the concentration of drug per drop in units (units/gtt), milligrams (mg/gtt), or micrograms (mcg/gtt). For the programmable volumetric infusion pump, the titration factor is the increment of increase or decrease in units, micrograms, or milligrams. If the only IV equipment available has the mL/hr feature, the titration factor of concentration per drop can be used. Smart pumps can infuse medication volume in increments of 0.01 mL/hr. Other pump features include a drug-specific dose calculator that allows the nurse to select a drug name, input the dosage, the concentration of the drug, and the weight of the patient (Figure 12-1). These infusion pumps make drug delivery and titration safer and easier. Any dose changes can be easily reprogrammed by the drug-specific dose calculator. The safety features of these advanced infusion pumps decrease medication errors. Many drug manufacturers are recommending Smart pumps for the delivery of all vasoactive medications used in critical care.
Calculating the titration factor is necessary when the technology of the advanced infusion pumps is unavailable. The titration factor can be added to or subtracted from the baseline infusion rate to determine the exact concentration of an infusion. Because the titration method of drug administration is primarily used when a patient’s condition is labile, calculating the titration factor gives the nurse the means of determining the exact amount of drug to be infused.
Charts for drug infusion, developed by drug manufacturers, can be used to adjust infusion rates for drug titrations. Often, the amount of drug being infused falls between calibrations on the charts. When this occurs, the titration factor can be used to determine the exact concentration of drug being administered. The titration factor can also be used to verify the correct selection from the chart.
EXAMPLE
Infuse Isuprel 2 mg in 250 mL D5W. Titrate 1-3 mcg/min to maintain heart rategreater than 50 beats/min andless than 130 beats/min and blood pressuregreater than 90 mm Hg systolic.
a. Find concentration of solution:
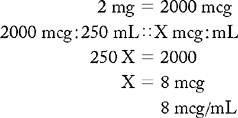
b. Infusion rate by volume per unit time:
Desired infusion rate by concentration is stated in the problem.
Note that the upper dosage and lower dosage must be determined.
Find volume rate per minute: mL/min:
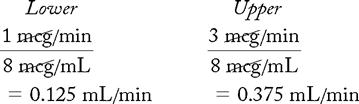
Find volume rate per hour: mL/hr (equivalent to gtt/min):
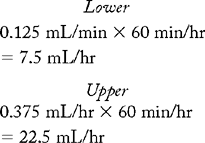
Dosage range is 7.5 mL/hr at 1 mcg/min, the lowest dose ordered, to 22.5 mL/hr at 3 mcg/min, the highest dose ordered.
Determine Titration Factor Using Infusion Pump
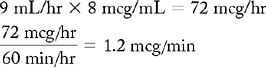
When the amount of fluid being titrated is 1 mL or greater (0.1 mL/hr lowest increment of infusion), the concentration of the solution multiplied by the volume per hour will give the total concentration to be given in 1 hour. The total volume in 1 hour divided by 60 min/hr will yield the concentration per minute.
EXAMPLE
Increase Isuprel from 7.5 mL/hr to 9 mL/hr.
When increments of less than 1 mL are being titrated, multiply the concentration by the lowest increment of infusion.
8 mcg/mL × 0.1 mL/hr = 0.8 mcg/hr
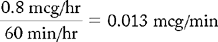
Titration factor is 0.8 mcg/hr or 0.013 mcg/min for the solution of Isuprel 2 mg in 250 mL D5W with 0.1 mL/hr as the lowest increment of infusion. If the baseline rate is 7.5 mL/hr and 1 mcg/min, increasing the rate by 0.1 mL/hr to 7.6 mL/hr will increase the per minute dose to 1.013 mcg/min. Since Isuprel is ordered in mcg/min, using the titration factor in mcg/min would give a very accurate dose if increases or decreases are needed.
Increasing or Decreasing Infusion Rates Using Infusion Pump
When increasing infusion rate (0.1 mL/hr lowest increment of infusion) from baseline, multiply the titration factor by the number of increases and add to beginning rate.
Example
| Baseline Data | |
| Order | Isuprel 2 mg in 250 mL |
| Concentration of solution | 8 mcg/mL |
| Beginning rate | 1 mcg/min |
| Volume per hour | 7.5 mL/hr |
| Lowest increment of infusion | 0.1 mL/hr (lowest pump setting) |
| Titration factors | 0.8 mcg/hr or 0.013 mcg/min |
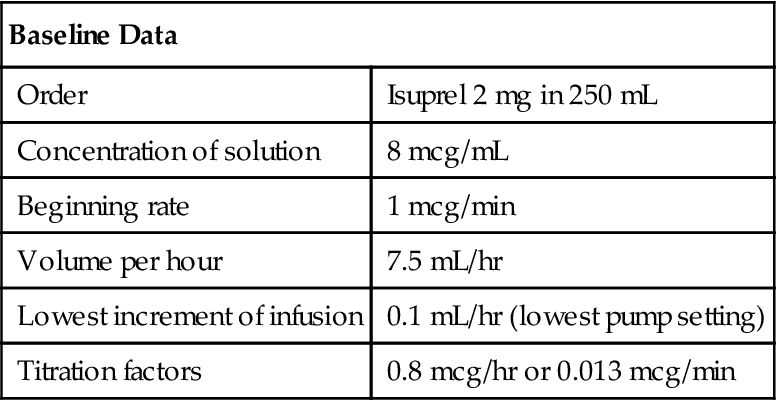
Since the order is given in mcg/min, the titration factor of mcg/min should be used. To increase infusion rate from 7.5 mL/hr to 7.7 mL/hr, a 0.2-mL increase on the infusion pump, multiply titration factor by 2. Multiply 2 × 0.013 mcg/min = 0.028 mcg/min, then add to baseline of 1 mcg/min and now the concentration per minute is 1.028 mcg/min. Incremental increases can be easily calculated by multiplying the titration factor by the number of increases, then adding to baseline.
EXAMPLE
| Hourly Rate (mL/hr) | Titration Factor | Concentration/min (ADD) |
| 7.5 mL/hr | 0.013 mcg/min | 1 mcg/min |
| 7.6 mL/hr | 0.013 mcg/min × 1 = 0.013 | 1.013 mcg/min |
| 7.7 mL/hr | 0.013 mcg/min × 2 = 0.026 | 1.026 mcg/min |
| 7.8 mL/hr | 0.013 mcg/min × 3 = 0.039 | 1.039 mcg/min |
To titrate downward, multiply titration factor by the number of decreases and subtract each decrease from current infusion rate.
EXAMPLE
| Hourly Rate (mL/hr) | Titration Factor | Concentration/min (SUBTRACT) |
| 10 mL/hr | 0.013 mcg/min | 1.325 mcg/min |
| 9.8 mL/hr | 0.013 mcg/min × 2 = 0.026 | 1.299 mcg/min |
| 9.4 mL/hr | 0.013 mcg/min × 6 = 0.078 | 1.247 mcg/min |
Determine Titration Factor Using a Microdrip IV Set
A microdrip IV set has a drop factor of 60 gtt/mL, so the number of drops per minute is the same as the hourly rate. In a situation where infusion pumps are not available, a microdrip IV set may be the only option to deliver small amounts of IV medication. Using the Isuprel data, the mL/hr rate will be 7.5 gtt counted per minute from the drip chamber. The titration factor is the amount of Isuprel in each drop.
Determine the titration factor:
The titration factor is 0.133 mcg/gt in a solution of Isuprel 2 mg in 250 mL D5W. In other words, changing drops per minute results in a corresponding change in milliliters per hour. If the baseline infusion rates are 1 mcg/min for concentration and 7.5 mL/hr for volume, increasing the infusion rate by 1 gt/min changes the concentration/minute by 0.133 mcg and increases the hourly volume by 1 mL to give a rate of 8.5 mL/hr.
Increasing or Decreasing Infusion Rates Using a Microdrip IV Set
To increase the infusion rate by 5 gtt/min from a baseline rate of 1 mcg/min, set up a ratio and proportion or multiply the titration factor (mcg/gt) by 5 to obtain the increment of increase.
EXAMPLES
or
0.133 mcg/gt × 5 gtt = 0.665 mcg
Adding 5 gtt/min increases the volume infusion rate by 5 mL/hr, from 7.5 to 12.5 mL/hr. The concentration of drug delivered is increased by 0.665 mcg/min to 1.665 mcg/min. For example,
1.000 mcg/min baseline rate
+ 0.665 mcg/min increment of rate increased
1.665 mcg/min adjusted infusion rate
Suppose the infusion rate was 3 mcg/min and a decrease was needed. To decrease the infusion rate by 10 gtt, set up another ratio and proportion or multiply the titration factor (mcg/gt) by 10.
EXAMPLES
or
0.133 mcg/gt × 10 gtt = 1.33 mcg
Subtracting 10 gtt/min decreases the infusion rate by 10 mL/hr, from 22.5 to 12.5 mL/hr. The amount of drug delivered is decreased by 1.33 mcg/min to 1.67 mcg/min. For example,
3.00 mcg/min baseline infusion rate
−1.33 mcg/min increment of rate decreased
1.67 mcg/min adjusted infusion rate

 I Calculating Concentration of a Solution
I Calculating Concentration of a Solution II CALCULATING INFUSION RATE
II CALCULATING INFUSION RATE III CALCULATING INFUSION RATE FOR SPECIFIC BODY WEIGHT
III CALCULATING INFUSION RATE FOR SPECIFIC BODY WEIGHT
 IV TITRATION OF INFUSION RATE
IV TITRATION OF INFUSION RATE

