CASE 12
A 62-year-old man complaining of crushing chest pain was rushed to the emergency room by ambulance. The physical examination showed that his pulse was 105 beats per minute (sinus tachycardia) and regular, arterial pressure was 130/92, and his respiratory rate was 26 breaths per minute (normal is 12–22). His EKG showed ST segment elevation and the patient was prophylactically administered aspirin and atenolol, a beta1-selective adrenergic antagonist. A blood sample from the patient revealed that the serum cardiac marker, cardiac-derived troponin I (c-TnI), was elevated. An angiogram was performed and the results showed that the proximal one-third of the left anterior descending artery was 95% occluded, the proximal one-third of the circumflex artery was 80% occluded, and the proximal one-third of the right coronary artery was 75% occluded. Because of the multiple stenotic lesions, a triple coronary bypass was performed. The bypass procedure was successful, but the patient’s ejection fraction was below normal. Digoxin was prescribed to improve contractile activity.
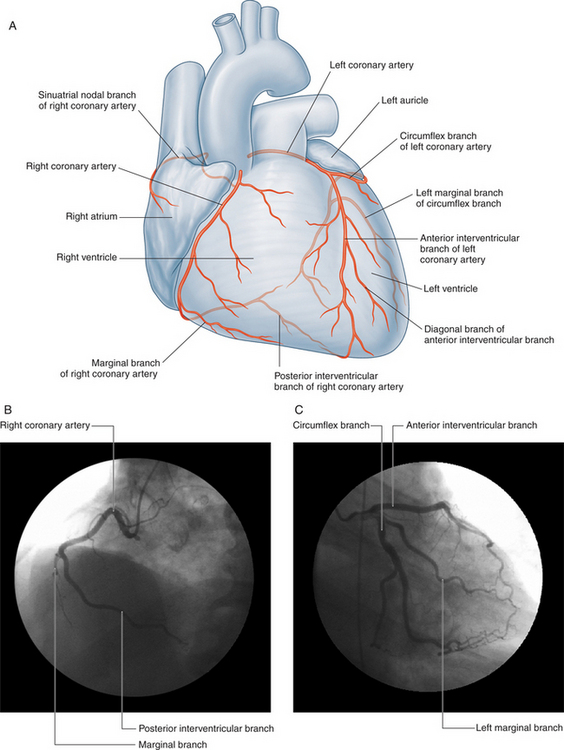
WHAT IS THE ARTERIAL SUPPLY TO THE HEART?
The heart is supplied by the right and left coronary arteries (Fig. 2-29). The ostia of these vessels are located in the aortic sinuses (of Valsalva) superior to the right and left coronary cusps of the aortic semilunar valve.
WHAT ARE SOME OF THE VARIATIONS IN THE CORONARY ARTERIES?
Variations in the coronary arteries are common. Some of these variations are:
WHAT IS THE VENOUS DRAINAGE OF THE HEART?
WHAT IS THE INNERVATION OF THE HEART?
Sympathetic innervation to the heart is provided as follows:
WHAT CORONARY ARTERY IS MOST FREQUENTLY NARROWED OR THROMBOSED?
The frequencies at which the coronary arteries are lesioned or thrombosed are:
WHAT BLOOD VESSELS CAN BE USED FOR CORONARY ARTERY BYPASS GRAFTS?
The preferred vascular conduits, however, are the right and/or left internal thoracic arteries. Arteries are preferred because they are more likely to remain patent over a 10-year period than venous conduits. The left internal thoracic artery is typically used to bypass the anterior interventricular artery, whereas the right internal thoracic artery is used to bypass the right coronary artery. If the right internal thoracic artery is sufficiently long, it can be grafted to the posterior interventricular artery or branches of the left coronary artery. The radial and gastro-omental arteries can also be used as bypass grafts.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree