INTRAVENOUS PREPARATIONS WITH CLINICAL APPLICATIONS
Objectives
• Name catheter sites for intravenous (IV) access.
• Calculate drops per minute of prescribed IV solutions for IV therapy.
• Determine the drop factor according to the manufacturer’s product specification.
• Calculate the drug dosage for IV medications.
• Calculate the flow rate for IV drugs being administered in a prescribed amount of solution.
• Explain the types and uses of electronic IV infusion devices.
Intravenous (IV) therapy is used for administering fluids containing water, dextrose, fat emulsions, vitamins, electrolytes, and drugs. Approximately 90% of all hospitalized patients, some outpatients, and some home-care patients receive IV therapy. Drugs are administered intravenously for direct absorption and fast action. Many drugs cannot be absorbed through the gastrointestinal tract, and the IV route provides bioavailability. Certain drugs that need to be absorbed immediately are administered by direct IV injection, sometimes over several minutes. However, many drugs administered intravenously are irritating to the veins because of the drug’s pH or osmolality and must be diluted and administered slowly.
Advantages of IV drug therapy are (1) rapid drug distribution into the bloodstream, (2) rapid onset of action, and (3) no drug loss to tissues. There are many complications of IV therapy, some of which are sepsis, thrombosis, phlebitis, air emboli, infiltration, and extravasation. The nurse must monitor for signs of these complications during the course of IV therapy.
Three methods are used to administer IV fluid and drugs: (1) direct IV drug injection, (2) continuous IV infusion, and (3) intermittent IV infusion. Continuous IV administration replaces fluid loss, maintains fluid balance, and is a vehicle for drug administration. Intermittent IV administration is primarily used for giving IV drugs.
Nurses play an important role in preparing and administering IV solutions and drugs. Nursing functions and responsibilities include (1) knowledge of IV sets and their drop factors, (2) calculating IV flow rates, (3) verifying compatibility of the IV solution and the drug, (4) mixing drugs and diluting in IV solution, (5) regulating IV infusion devices, and (6) maintaining patency of IV accesses.
INTRAVENOUS ACCESS SITES
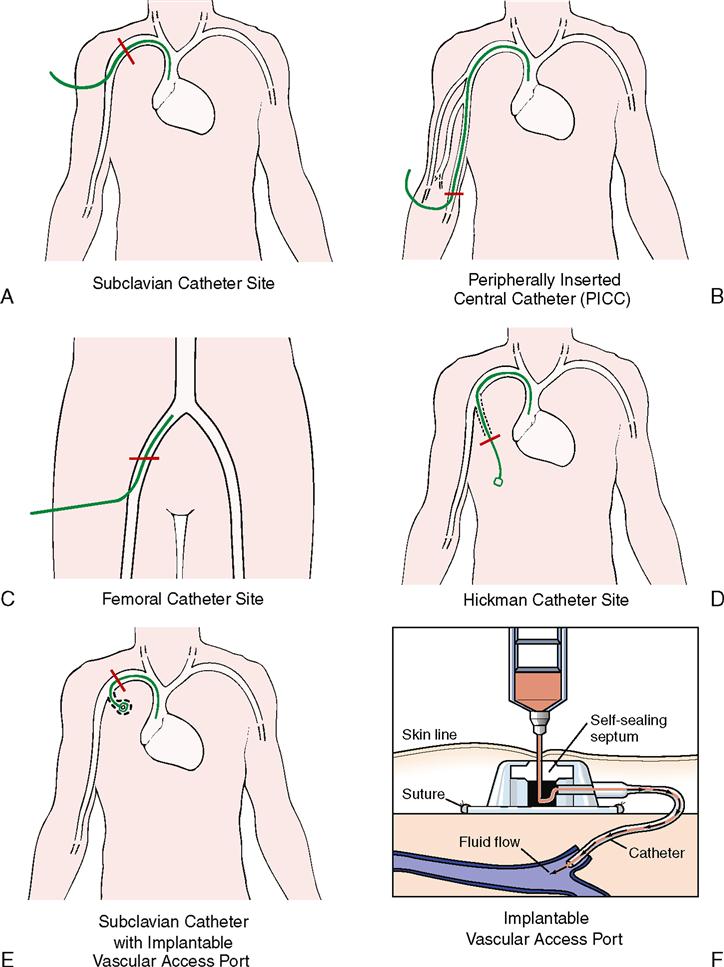
The successful administration of IV drugs and fluids depends on a patent vascular access. The most common site for short-term (less than 1 week) IV therapy is the peripheral short site, which uses the dorsal and ventral surfaces of the upper extremities. Catheter length is normally 1 to 3 inches (Figure 10-1).
The peripheral midline site for IV therapy that may last 2 to 4 weeks uses the veins in the area of the anticubital fossa—the basilic, brachial, cephalic, cubital, or medial. Midline peripheral catheters are between 3 and 8 inches in length.
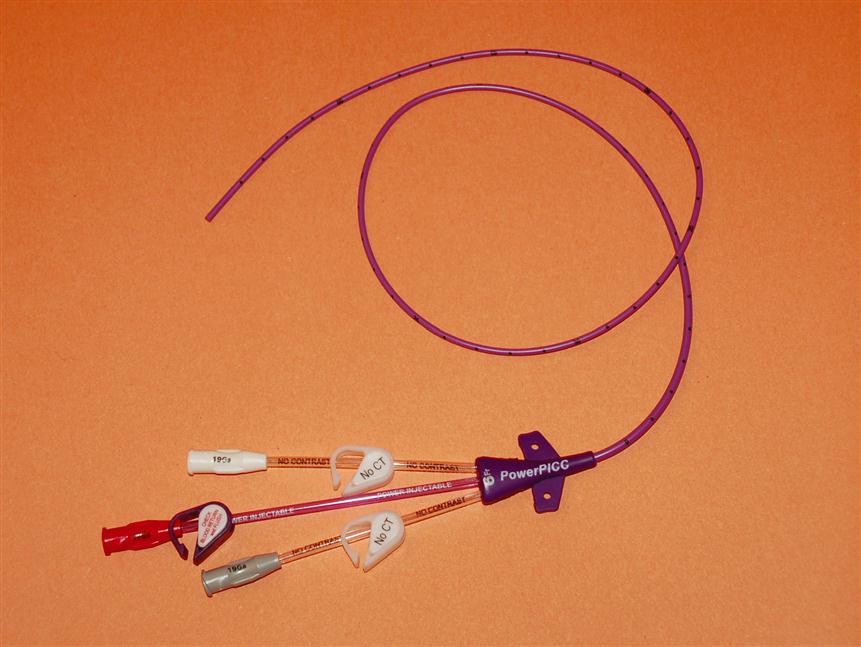
The peripherally inserted central catheter (PICC) (Figure 10-2) can be used for IV therapy for up to one year. The catheter length is 21 inches. The insertion site is the region of the antecubital fossa that uses the same veins as the peripheral midline. The catheter is advanced through the vein in the upper arm until the tip rests in the lower third of the superior vena cava. Since the tip of the PICC line rests in the superior vena cava it is considered a central line. Compared with other access sites, the multilumen PICC is dependable and cost-effective. It is also versatile because it can be used for medication, IV fluids, blood products, hyperalimentation, and blood sampling. Infection rates are very low with PICC lines. Since the PICC line can be maintained on an outpatient basis, patients can be discharged early from the hospital. In some states registered nurses certified in IV therapy can insert PICC lines.
The central venous site is used for patients who need long-term continuous infusions of fluids, medication, or nutritional support that cannot be sustained with a peripheral site. Central venous catheter (CVC) sites are the superior vena cava and the inferior vena cava. The superior vena cava is accessed from the internal jugular vein and the right or left subclavian vein, whereas the inferior vena cava is accessed from the femoral vein. Length of the CVC can vary from 6 to 28 inches. Insertion requires a minor surgical procedure—a percutaneous vein cannulation with the introduction of a single- or multilumen catheter; the tip of the catheter rests in the superior vena cava just above the right atrium.
Patients who need vascular access for long-term use, such as chemotherapy, antibiotic therapy, or nutritional support, are given much longer catheters, which are tunneled under the skin after the vein is cannulated. The catheter and its drug infusion port exit from the subcutaneous tissue to a site on the chest. Examples of these devices are the Hickman, Groshong, NeoStar, and Cook catheters.
Another type of catheter for long-term use has an implantable infusion port that is inserted in the subcutaneous tissue under the skin. These devices are called vascular access ports and they have a larger drug port or septum than other catheters. Care must be taken to use a non-coring needle that slices the port instead of making holes, so that the septum will close instead of leaking after the needle has been removed (Figure 10-3).
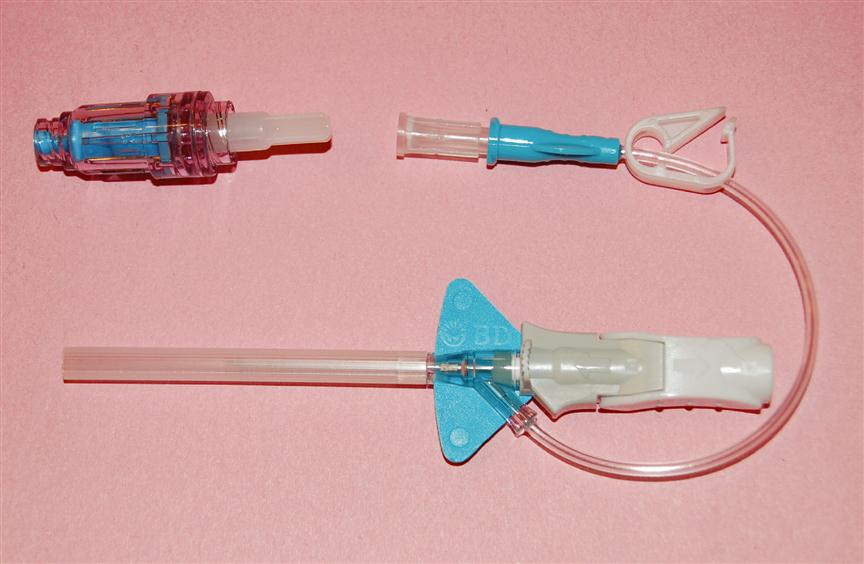
Intermittent Infusion Add-On Devices
When IV access sites are used for intermittent therapy instead of continuous infusion, they must be flushed periodically to maintain patency. An intermittent infusion add-on device can be attached to the end of the vascular access device, catheter, or needle to close the connection that was attached to the IV tubing. There are many types of add-on devices, such as extension loops, solid cannula caps, and injection access caps. All add-on devices should use Luer-Lok design as a safety measure. Use of add-on devices should be included as part of the protocol of the institution (Figure 10-4). These devices have ports (stoppers) where needleless syringes can be inserted when drug therapy is resumed. This practice can eliminate the need for a constant low-rate infusion to keep the vein open (KVO) and reduce excessive fluid intake. The use of intermittent infusion devices can allow the patient greater mobility and can be cost-effective because less IV tubing, IV solution, and regulating equipment are needed.
IV sites should be flushed every 8 to 12 hours or before and after each drug infusion, depending on institutional policy, to maintain patency. Table 10-1 gives suggested flushing times. Pre-filled single-use syringes of saline solution are available to flush infusion devices (Figure 10-5). The intent of pre-filled single-use syringes is to prevent the cross-contamination that can occur with a multidose vial. The volume of the flush used for vascular access devices is twice the volume of the catheter plus any connected devices such as a three-way stopcock or an extension set. Saline solution flushes are generally used for venous access devices that are tunneled or implanted.
TABLE 10-1
Venous Access Devices: Flushing for Peripheral and Central Venous*
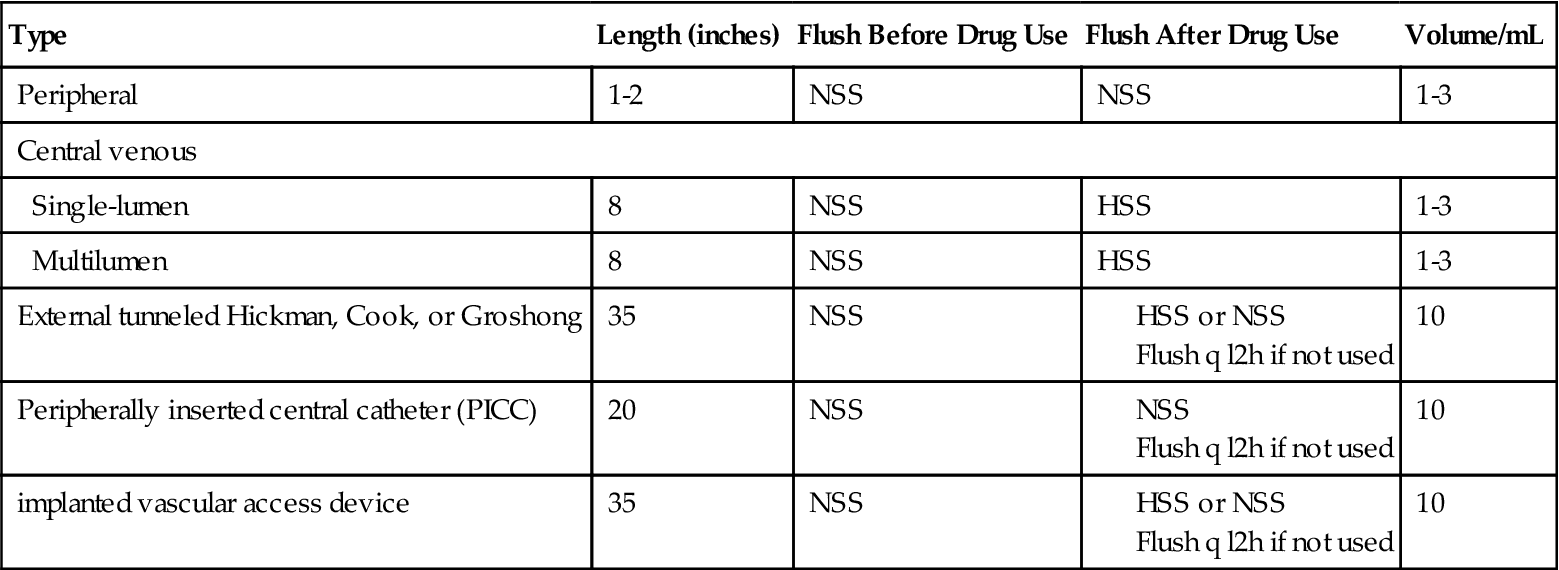
HSS, Heparinized saline solution; NSS, normal saline solution.
*lf the adapter/cap is pressurized, then normal saline solution is used, not a heparin solution. Follow the institution policy procedure and manufacturer’s guidelines.
DIRECT INTRAVENOUS INJECTIONS
Medications that are given by the IV injection route are calculated in the same manner as medications for intramuscular (IM) injection. This route is often referred to as IV push. Clinically, it is the preferred route for patients with poor muscle mass or decreased circulation, or for a drug that is poorly absorbed from the tissues. Medications administered by this route have a rapid onset of action, and calculation errors can have serious, even fatal, consequences. Drug information inserts must be read carefully, and attention must be paid to the amount of drug that can be given per minute. If the drug is pushed into the bloodstream at a faster rate than is specified in the drug literature, adverse reactions to the medication are likely to occur.
Calculating the amount of time needed to infuse a drug given by direct IV infusion can be done with the use of ratio and proportion.
Examples
Set up a ratio and proportion using the recommended amount of drug per minute on one side of the equation; these are the known variables. On the other side of the equation are the desired amount of drug and unknown desired minutes: a. amount in milliliters (mL); b. number of minutes.
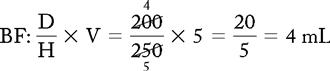
PROBLEM 1: Order: Dilantin 200 mg, IV, STAT.
Drug available: Dilantin 250 mg/5 mL. IV infusion not to exceed 50 mg/min.

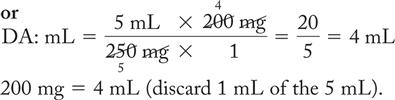
b. known drug: known minutes:: desired drug: desired minutes
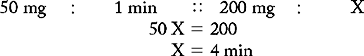
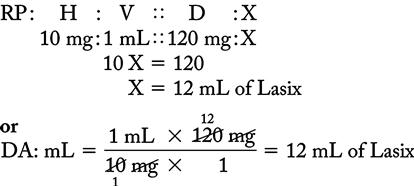
PROBLEM 2: Order: Lasix 120 mg, IV, STAT.
Drug available: Lasix 10 mg/mL. IV infusion not to exceed 40 mg/min.
b. known drug: known minutes:: desired drug: desired minutes
When dosing instructions give the amount of drug and specify infusion time, the amount of drug can be divided by the number of minutes to attain the per-minute amount to be infused.
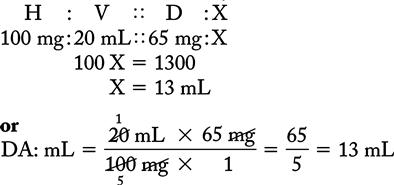
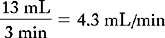
PROBLEM 3: Order: inamrinone (Inocor) 65 mg, IV bolus over 3 minutes.
Drug available: Inocor 100 mg/20 mL
A. Determine the amount in milliliters of drug solution to administer.
B. Determine the number of minutes that is required for the direct IV drug dose to be administered for each of the practice problems.
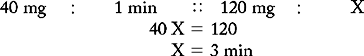
1. Order: protamine sulfate 50 mg, IV, STAT.
Drug available:
IV infusion not to exceed 5 mg/min.
a. Amount in milliliters ____________
b. Number of minutes to administer ____________
2. Order: dextrose 50% in 50 mL, IV, STAT.
Drug available: dextrose 50% in 50 mL.
IV infusion not to exceed 10 mL/min.
Number of minutes to administer 50% of 50 mL __________
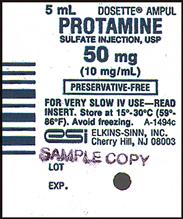
3. Order: calcium gluconate 4.65 mEq, IV, STAT.
Drug available:
IV infusion not to exceed 1.5 mL/min. Note: 4.65 mEq/10 mL.
a. Amount in milliliters ____________
b. Number of minutes ____________
4. Order: prednisolone 50 mg, IV, q12h.
Drug available: prednisolone 50 mg in 5 mL.
IV infusion not to exceed 10 mg/min.
a. Amount in milliliters ____________
b. Number of minutes ____________
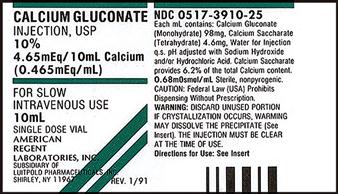
5. Order: morphine sulfate 6 mg, IV, q3h, PRN.
Drug available:
Infusion not to exceed 10 mg/4 min.
a. Amount in milliliters ____________
b. Number of minutes ____________
6. Order: digoxin 0.25 mg, IV, daily.
Drug available:
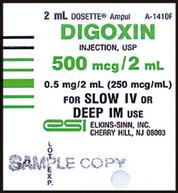
a. Amount in milliliters ____________
b. How many mL/min should be infused? ____________
7. Order: Haldol 2 mg, IV, q4h, PRN.
Drug available: Haldol 5 mg/mL.
IV infusion not to exceed 1 mg/min.
a. Amount in milliliters ____________
b. Number of minutes ____________
8. Order: Ativan 6 mg, IV, q6h, PRN.
Drug available: Ativan 4 mg/mL.
IV infusion not to exceed 2 mg/min.
a. Amount in milliliters ____________
b. Number of minutes ____________
9. Order: diltiazem (Cardizem) 20 mg IV over 2 minutes.
Drug available:

a. How many milliliters (mL) would you give? ____________
b. How many milliliters (mL) would you infuse per minute? ____________
10. Order: granisetron (Kytril) 10 mcg/kg, 30 minutes before chemotherapy.
Infuse 1 mg over 60 seconds.
Patient weighs 140 pounds.
Drug available:
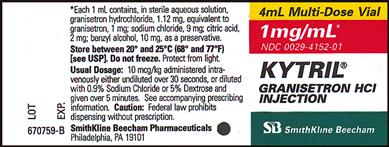
a. How many kilograms (kg) does the patient weigh? ____________
b. How many milligrams (mg) should the patient receive? ____________
c. For how many seconds should the drug dose be infused? ____________
CONTINUOUS INTRAVENOUS ADMINISTRATION
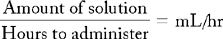
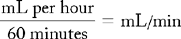
When IV solutions are required, the health care provider orders the amount of solution per liter or milliliter to be administered for a specific time, such as for 24 hours. The nurse calculates the IV flow rate according to the drop factor, the amount of fluid to be administered, and the infusion time.
Intravenous Infusion Sets
All infusion sets have the same components: a sterile spike for entry into the IV bag or bottle, a drip chamber for counting drops and managing flow, a roller clamp that controls flow through the tubing, tubing length from drip chamber to IV site, Y-site for adding a secondary set or giving drugs IV, and the adapter (which attaches to the needle or catheter) (Figure 10-6). Often a filter is added to the IV line to remove bacteria, particles, and air. Figure 10-7 shows the IV containers, bag, and bottle.
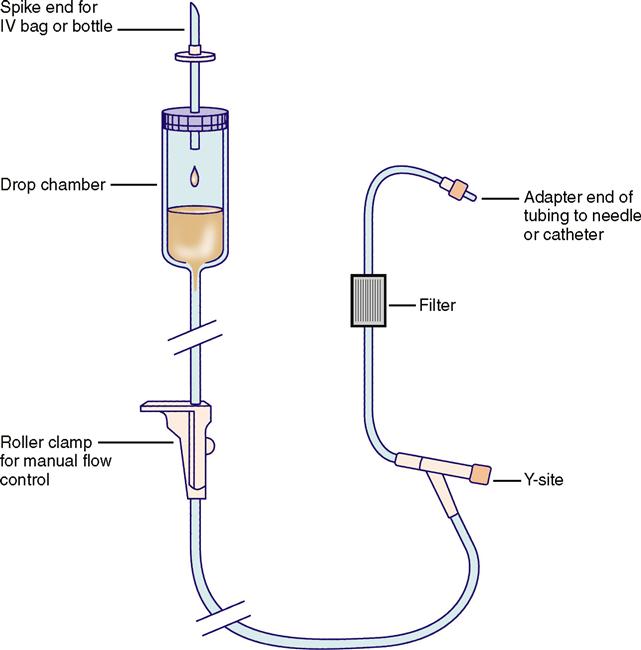
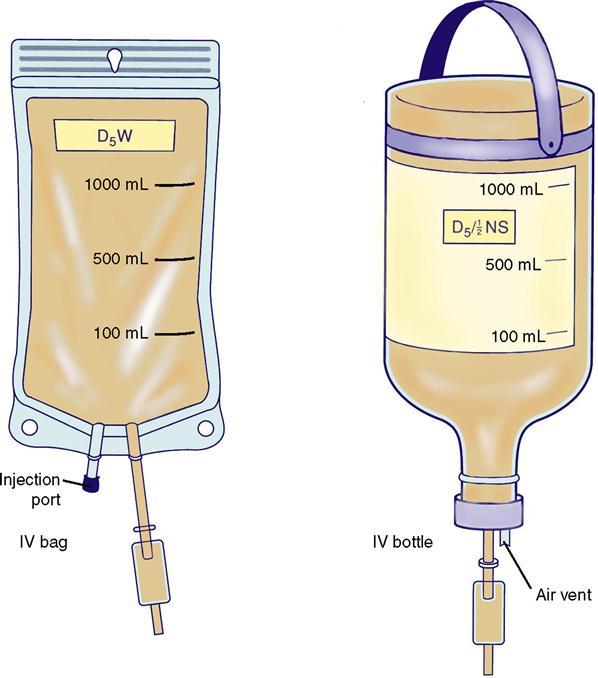
IV sets are either vented or unvented. Vented sets are used for IV bottles that have no vents and need a vent for air to enter the bottle so the fluid will flow out. Unvented sets are for bottles or bags that either have their own venting system or do not need a venting system. Glass bottles are primarily used when the medication is not compatible with plastic because the drug either adheres to the plastic or is absorbed by the plastic.
If the IV infusion is not placed on a flow control device but instead is delivered by gravity, then the hourly rate will have to be adjusted manually. It is necessary to know the drop factor of the IV set to calculate the hourly infusion rate. The drop factor, or the number of drops per milliliter (mL), is printed on the package of the infusion set and found on top of the drip chamber. Sets that deliver large drops per milliliter (10-20 gtt/mL) are referred to as macrodrip sets, and those that deliver small drops per milliliter (60 gtt/mL) are called microdrip or minidrip sets (Table 10-2, Figure 10-8).
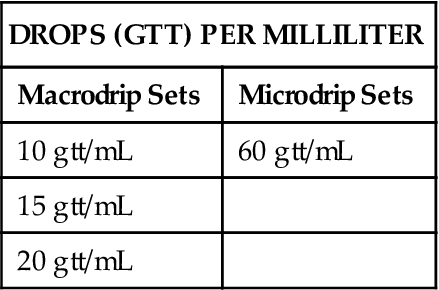
TABLE 10-2
| DROPS (GTT) PER MILLILITER | |
| Macrodrip Sets | Microdrip Sets |
| 10 gtt/mL | 60 gtt/mL |
| 15 gtt/mL | |
| 20 gtt/mL | |
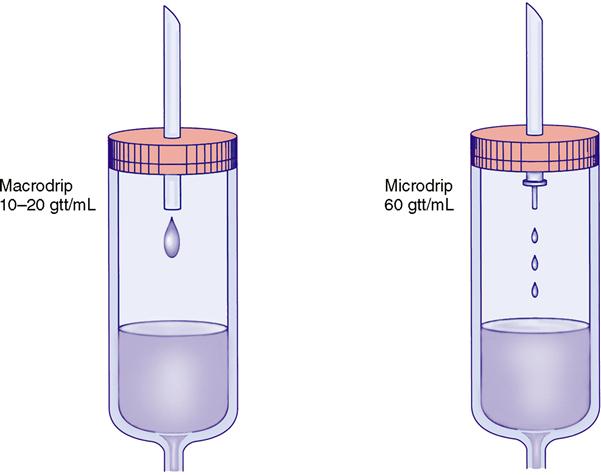
Drip rates are adjusted by counting the drops coming through the spike into the drip chamber. While looking at the second hand of your watch, adjust the roller clamp to determine the correct number of drops in one minute. It is more difficult to count when the drops are smaller and the drop rate is faster. One advantage of the microdrip set is that the number of milliliters per hour is the same as the drops per minute (e.g., if the infusion rate is 50 mL/hr, the drip rate is 50 gtt/min). When the IV rate is 100 mL/hr or higher, the macrodrip set generally is used. Slow drip rates (less than 100 mL/hr) make macrodrip adjustments too difficult (e.g., at 50 mL/hr, the macrodrip rate would be 8 gtt/min). Therefore, if the IV rate is 100 mL/hr or lower, the microdrip is preferred.
When manual flow control is used to adjust the infusion rate, the IV drip rate should be monitored every half-hour to hour, so that IV fluids are infused as prescribed.
At times, IV fluids are given at a slow rate to keep vein open (KVO), also called to keep open (TKO). Reasons for ordering KVO include (1) a suspected or potential emergency situation requiring rapid administration of fluids and drugs, and (2) the need to maintain an open line to give IV drugs at specified hours. For KVO, a microdrip set (60 gtt/mL) and a 250-mL IV bag can be used. KVO should have a specific infusion rate, such as 10 to 20 mL/hr, or should be given according to the institution’s protocol.
CALCULATION OF INTRAVENOUS FLOW RATE
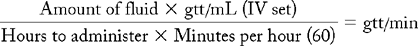
Three different methods can be used to calculate IV flow rate (drops per minute or gtt/min). The nurse should select one of these methods, memorize it, and use it to calculate dosages.*
 THREE-STEP METHOD
THREE-STEP METHOD
 TWO-STEP METHOD
TWO-STEP METHOD
 ONE-STEP METHOD
ONE-STEP METHOD
Safety Considerations
All IV infusions should be checked every half-hour or hour, according to the policy of the institution, to ensure the appropriate rate of infusion and to assess for potential problems, especially when manual flow control is used. Common problems associated with IV infusions are kinked tubing, infiltration, and “free-flow” IV rates. If IV tubing kinks and the flow is interrupted, the prescribed amount of fluid will not be given, and the access site can clot. When infiltration occurs, IV fluid extravasates into the tissues, not into the vascular space, and trauma occurs to tissues at the IV site. Again, in this situation, the prescribed amount of IV fluid is not infused. Free-flow IV rate refers to a rapid infusion of IV fluids—much faster than prescribed—causing fluid overload, which occurs when too much fluid in the vascular space or medication is administered faster than prescribed, resulting in a toxic reaction. This is the most prevalent drug error and has led to the use of electronic infusion devices.
Electronic infusion devices are not without flaws; mechanical problems occur and these devices can be incorrectly programmed, resulting in the wrong infusion rate. Fluid overload, thrombus formation, and infiltration are complications of IV therapy that can be avoided with frequent monitoring of IV infusions. See Appendix A for more detailed information on safe practice for IV drug administration.
Adding Drugs Used for Continuous Intravenous Administration
Drugs such as multiple vitamins and potassium chloride can be added to the IV solution bag for continuous infusion. This process of mixing or compounding an IV solution should be completed before the IV bag or bottle is hung. The medication is prepared using sterile technique and is added through the injection port to the bag or bottle that is to be rotated, to ensure that the drug is dispersed. Medication labels must be placed on the IV bag or bottle, clearly stating the patient’s name and any other identifiers as specified by policy, such as name of the drug, amount, concentration, and strength of all ingredients without abbreviation; also, date, nurse’s initials, time, and the time the IV should be completed should be provided. It is important to follow institutional policies and procedures when adding medication to continuous IV fluid.
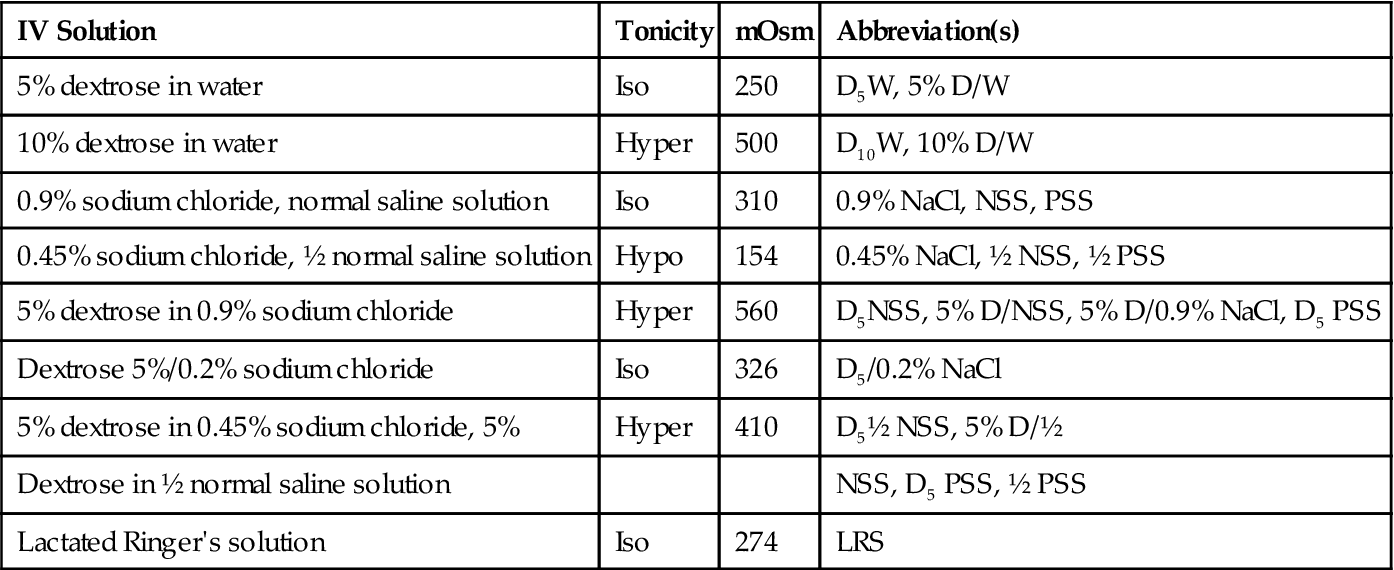
Types of Solutions
All IV solutions contain various solutes and electrolytes that are added for specific therapies. Common solutes include dextrose (D) and sodium chloride (NaCl). The strength of the solution is expressed in percent (%), such as 0.45%, which means 0.45 g in 100 mL. Common commercially prepared IV solutions are dextrose in water (D5W), dextrose with one-half normal saline solution (D5 0.45%), normal saline solution (0.9% NaCl), one-half normal saline solution (0.45% NaCl), and lactated Ringer’s solution (LRS). Lactated Ringer’s solution contains sodium, chloride, potassium, calcium, and lactate.
Tonicity of IV Solutions
The terms tonicity and osmolality have been used interchangeably, but tonicity refers to the concentration of IV solution, whereas osmolality is the concentration of body fluids (e.g., blood, serum). IV solutions produce tonicity in the cells of the body; this is the movement of water molecules into and out of the cells because of their surrounding fluid environment. IV solutions are divided into three categories: hypertonic, hypotonic, and isotonic. The range of tonicity is measured in milliosmoles, and the normal range is 240 to 340 mOsm: + 50 mOsm and/or − 50 mOsm of 290 mOsm. Hypertonic solutions cause water molecules to diffuse out of the cells and exert a hyperosmolar effect. For example, a hypertonic solution is D5 0.9% normal saline (NaCl) because it has an osmolarity of 560 mOsm. Hypotonic solutions cause water molecules to diffuse into the cells and exert a hypo-osmolar effect. A solution of 0.45% normal saline (NaCl) is hypo-osmolar and has an osmolarity of 154 mOsm. D5W is iso-osmolar with an osmolality of 250 mOsm; however, the dextrose is metabolized quickly, leaving only water, thus making the solution hypotonic. Isotonic solutions maintain the same concentration of water molecules on both sides of the cell, so no net movement occurs. The osmolarity of isotonic solutions is 240 to 340 mOsm, similar to blood, and LRS and 0.9% normal saline solution (NaCl) are the best examples. Table 10-3 lists the names of selected IV solutions, their tonicity, and their osmolarity, as well as the abbreviations for these solutions.
TABLE 10-3
Abbreviations for IV Solutions with Tonicity and Osmolarity
| IV Solution | Tonicity | mOsm | Abbreviation(s) |
| 5% dextrose in water | Iso | 250 | D5W, 5% D/W |
| 10% dextrose in water | Hyper | 500 | D10W, 10% D/W |
| 0.9% sodium chloride, normal saline solution | Iso | 310 | 0.9% NaCl, NSS, PSS |
| 0.45% sodium chloride, ½ normal saline solution | Hypo | 154 | 0.45% NaCl, ½ NSS, ½ PSS |
| 5% dextrose in 0.9% sodium chloride | Hyper | 560 | D5NSS, 5% D/NSS, 5% D/0.9% NaCl, D5 PSS |
| Dextrose 5%/0.2% sodium chloride | Iso | 326 | D5/0.2% NaCl |
| 5% dextrose in 0.45% sodium chloride, 5% | Hyper | 410 | D5½ NSS, 5% D/½ |
| Dextrose in ½ normal saline solution | NSS, D5 PSS, ½ PSS | ||
| Lactated Ringer’s solution | Iso | 274 | LRS |
EXAMPLES
Two problems in determining IV flow rate are given. Each problem is solved with each of the three methods for calculating IV flow rate.
PROBLEM 1: Order: 1000 mL of D5½ NSS (5% dextrose in ½ normal saline solution) in 6 hours.
Available: 1 L (1000 mL) of D5½ NSS solution bag: IV set labeled 10 gtt/mL.
How many drops per minute (gtt/min) should the patient receive?
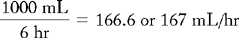
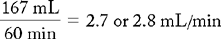
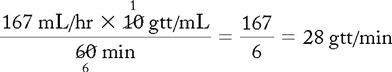
10 and 60 cancel to 1 and 6.
If mL/hr is given, use only part b of the two-step method for calculating IV flow rate.
One-Step Method:
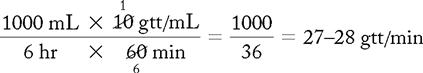
10 and 60 cancel to 1 and 6.
For the purpose of avoiding errors, the use of a hand calculator is strongly suggested.
Answer: 28 gtt/min.
PROBLEM 2: Order: 1000 mL of D5W (5% dextrose in water), 1 vial of MVI (multiple vitamin), and 20 mEq of KCl (potassium chloride) every 8 hours.
Available: 1000 mL D5W solution bag
1 vial of MVI = 5 mL
40 mEq/20 mL of KCl in an ampule
IV set labeled 15 gtt/mL
How many milliliters (mL) of KCl would you withdraw as equivalent to 20 mEq of KCl?
How would you mix KCl in the IV bag?
How many drops per minute should the patient receive?
Procedure: MVI: Inject 5 mL of MVI into the rubber stopper on the IV bag. KCl: Calculate the prescribed dosage for KCl by using the basic formula, ratio and proportion, or dimensional analysis.
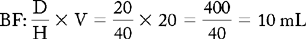
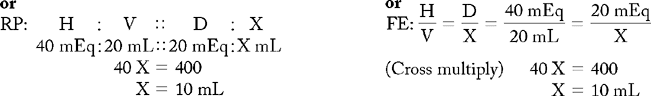
Withdraw 10 mL of KCl and inject it into the rubber stopper on the IV bag. Make sure the KCl solution and MVI additives are dispersed throughout the IV solution by rotating the IV bag.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





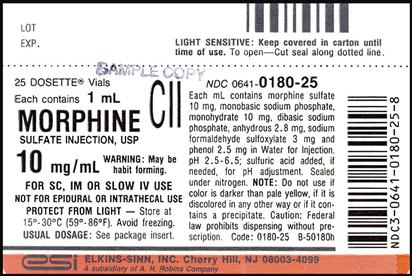
 I DIRECT IV INJECTION
I DIRECT IV INJECTION