1 CASE 1
PHYSICAL EXAMINATION
LABORATORY STUDIES
PATHOPHYSIOLOGY OF KEY SYMPTOMS
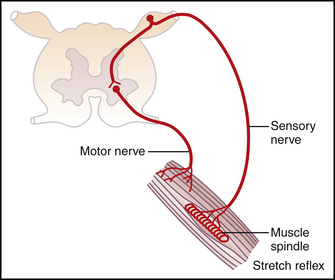
An appropriate patellar tendon reflex requires afferent input from the muscle spindles, transmission of the afferent action potential to the spinal cord, a monosynaptic reflex within the spinal cord, efferent action potential transmission by the alpha (α)-motor neuron, transmission across the neuromuscular synapse, activation of the skeletal muscle, and, finally, contraction (Fig. 1-1). This patient shows a hyperreflexive response in the right leg. Normally, the α-motor neurons receive descending inhibitory input from upper motor neurons and both inhibitory and stimulatory input from interneurons (Figs. 1-2 and 1-3). Hyperreflexia can be an indication that the normal descending input is diminished, which is characteristic of an upper motor neuron disease.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree